 |
 |
- Search
| Arch Aesthetic Plast Surg > Volume 23(3); 2017 > Article |
|
Abstract
Background
Breast reconstruction involves several steps, culminating in the creation of the nipple-areolar complex. Numerous methods of nipple reconstruction have been attempted, and have all proven somewhat successful in providing tissue for projection. In this clinical study, we evaluated a new technique using an acellular dermal matrix (ADM; AlloDerm®) adjunct to a skin flap (C-V flap technique) in nipple reconstruction.
Methods
In 2016, 13 nipple reconstructions were performed using this technique. We designed the C-V flap in the proper position on the breast. After the skin flap was elevated, a 1.5 ├Ś 1.5-cm AlloDerm┬« section was grafted to the inner surface of the elevated C-V flap; the grafted area was then folded into a cylindrical shape. Nipple projection was measured with an electronic caliper at the time of surgery and at 3 weeks and 3 months postoperatively.
Results
Immediately postoperatively, nipple projection ranged from 5 to 11 mm (mean, 8.1 mm). The mean maintenance of nipple projection at 3 months postoperatively was 73.14% ┬▒ 16.39% (82% and 58% in the breast implant and autologous tissue flap groups, respectively), as compared with the immediate postoperative measurements.
Breast reconstruction involves several steps, culminating in the creation of the nipple-areolar complex. Nonetheless, adequate maintenance of nipple projection remains a problem faced by plastic surgeons. Numerous nipple reconstruction methods have been introduced, and various materials including cartilage [1], bone [2], fat [3], dermal graft [4], and acellular dermal matrix (ADM) [5] have been used to provide stable long-term projection of the reconstructed nipple. However, reconstructed nipples lose their projection over time, leading to late-onset flattening. Losken et al. [6] reported that the loss of initial nipple projection in the C-V flap technique was less than 50% in previous studies. AlloDerm® (LifeCell Corp., Branchburg, NJ, USA) was first employed for nipple reconstruction in 2005 by Nahabedian [5]. It was rolled and used as a filling material within the pocket made by the lateral wings of the flap. It was reported that the use of AlloDerm® in nipple reconstruction resulted in improved long-term projection. Subsequently, several reports have been published discussing the positive role of ADM in nipple reconstruction.
In this clinical study, we evaluated a new technique in which an ADM (AlloDerm®) adjunct is applied to the skin flap (via the C-V flap technique) in nipple reconstruction in order to maximize the retention of ADM, with the goal of enhancing the maintenance of projection of the reconstructed nipple.
In 2016, 13 nipple reconstructions (9 unilateral and 2 bilateral) were performed using this technique at our institution. Eight nipples were reconstructed on breast mounds created with breast implants after using a breast expander, and 5 were reconstructed on breast mounds with autologous tissue flaps (3 transverse rectus abdominis musculocutaneous [TRAM] flaps, 1 latissimus dorsi (LD) flap, and 1 LD flap with a breast implant). The mean age of the 11 women was 50.1 years (range, 40ŌĆō68 years).
During the procedure, we designed a C-V flap in the proper position on the breast. The dimensions of the skin flaps were approximately 3 to 4├Ś1 cm, with some diversity in the measurements depending on the size of the opposite nipple. After the skin flap was elevated, a 1.5├Ś1.5-cm AlloDerm┬« section was grafted to the inner surface of the elevated C-V flap with #5-0 vicryl sutures, and both ends of the V-flaps were reinforced with AlloDerm┬«, were wrapped around each other, and sutured with 5-0 nylon sutures. The flap that had been overgrafted with AlloDerm┬« was then folded into a cylindrical shape (Fig. 1). A 5-mm-thick foam dressing material with a central hole was placed around the new nipple as a protective dressing. The protective dressing was maintained for 3 weeks. Nip ple projection was measured with an electronic caliper at the time of surgery, at 3 weeks postoperatively, and at 3 months postoperatively.
Nipple projection at the time of surgery ranged from 5 to 11 mm (mean, 8.1 mm). In the breast implant group, the nipple projection measurements initially ranged from 5 to 11 mm (mean, 7.7 mm) at the time of surgery, and from 5 to 8 mm (mean, 5.8 mm) at 3 months postoperatively (Table 1).
In the flap group, nipple projection measurements ranged from 6 to 11 mm (mean, 9.2 mm) at the time of surgery, and from 3 to 8 mm (mean, 5.4 mm) at 3 months postoperatively. The initial projection of the reconstructed nipple was individualized depending on the contralateral nipple projection. Therefore, the loss of nipple projection should be compared using the percentage difference between the initial and final projection measurements divided by the initial projection measurement. Our study demonstrated that the mean maintenance of nipple projection at 3 months was 73.14%┬▒ 16.39%, as compared with the projection seen in the immediate postoperative period (Fig. 2). In the breast implant group, the average maintenance of nipple projection was 82%┬▒11.57% at 3 months postoperatively. In the autologous tissue flap group, the average maintenance of nipple projection was 58%┬▒10.75% at 3 months post operatively.
No complications were noted. The projection did not decrease from the immediate to the 3-week postoperative period due to the presence of the protective dressing material. However, from 3 weeks to 3 months postoperatively, the projection decreased markedly. Postoperative views of the reconstructed nipples are shown in Fig. 3 to 7.
Various techniques and materials have been used to enhance the long-term projection of reconstructed nipples. Reconstructed nipples with skin flaps often lose their projection due to scar contracture over time. Losken et al. [6] reported that the long-term projection of reconstructed nipples with C-V flaps was reduced to less than 50% of the initial projection. Therefore, it is necessary to provide a core strut to overcome the contracture of the skin flap. Various materials have been used as core struts, including cartilage, dermofat tissue, artificial bone materials, and ADM.
Guerra et al. [7] described the incorporation of rib cartilage into skin flaps to increase nipple projection in cases that were reconstructed with perforator flaps. Within the flap, the authors used a piece of rib cartilage, which was obtained during the breast reconstruction and banked under the skin until nipple reconstruction. By using this technique, the authors obtained stable and reliable projection of the nipple, although a 4% incidence of cartilage graft loss was seen, caused by exposure of the graft or ischemia of the skin flap. Yanaga [2] applied a technique using artificial bone in 100 patients for the long-term preservation of projection, and reported the average reconstructed nipple height to be 80.5% of that measured on the contralateral side. However, tissues that are stiff, such as cartilage and bone, elicit a risk of exposure by external compression and friction, and increase the chance of needing revision surgery.
Among the materials used as core struts, ADM has been widely used in various reconstructive procedures. Another study has demonstrated nipple projection improvements in cases using ADM. Nahabedian [5] was the first to describe the usage of AlloDerm┬« in secondary and tertiary nipple reconstruction with an elongated C flap and a C-V flap. During secondary and tertiary nipple reconstruction, the authors performed the procedures using AlloDerm┬« and reported improved results. Additionally, Garramone and Lam [8] described the use of AlloDerm┬« in primary nipple reconstruction to improve long-term nipple projection. This study involved a total of 30 nipple reconstructions that were performed using 14 TRAM flaps and 16 tissue-expanded breast mounds. A 1.5├Ś4.5-cm piece of AlloDerm┬« was placed into the core of the newly reconstructed nipple and closed using sutures. The average maintenance of nipple projection at 12 months was 56% in the TRAM flap group and 47% in the tissue expander group, respectively.
Additionally, Chia et al. [9] reported the use of a C-V flap with a rolled dermal graft (3├Ś1.5 cm) from harvested autologous tissue. The 12-month average maintenance of nipple projection was 70.2% for the TRAM flap group, 76.3% for the LD flap group, and 61.8% for the tissue-expanded group, respectively. Vidya et al. [10] reported a nipple reconstruction technique using a 5├Ś5-cm rolled piece of ADM (EGIS┬«; QuaMedical, Zuidwolde, the Netherlands) as a strut in 5 patients who underwent skin-sparing mastectomy, with pleasing results.
However, it is difficult to estimate the degree to which one technique is superior to another. Nipple projection is influenced by many factors, including the size and thickness of the skin flap, the kind of ADM used, the underlying materials of the breast mound, and the type of mastectomy performed. Usually, the skin flap is very thin in patients who undergo skin expansion using a tissue expander or in patients who undergo a TRAM flap with skin stretch marks. In addition, various ADMs are used throughout the world. Thus, the thickness and absorption rate of the ADMs vary in accordance with the ADM processing method used. For example, Park et al. [11] reported good results using an ADM (MegaDerm®; L&C Bio Corp., Seoul, Korea) core strut in nipple reconstruction. There are some differences between AlloDerm® and MegaDerm® in terms of thickness and the absorption rate. Therefore, it is difficult to accurately compare the outcomes of different techniques using different ADMs.
In general, AlloDerm® or another dermal graft has been used to fill the internal space of cylindrical-shaped skin flaps in most reports. However, to maintain the dermal matrix volume and/or to serve as a volume enhancer, the dermal matrix should be well-vascularized. We believe that the core of the rolled dermal matrix is relatively less vascularized and is predisposed to be absorbed, potentially leading to infection. In our previous experiences, a strut constructed with a rolled dermal matrix tended to be less integrated with the skin flap for nipple reconstruction. Incompletely integrated dermal matrixes are pushed down and easily displaced beyond the nipple area by external compression. Therefore, we needed to secure the dermal matrix to the skin flap, and chose a technique in which the dermal matrix is grafted onto the undersurface of the skin flap for secure integration of the dermal matrix as a volume enhancer of the skin flap. Further follow-up of these patients beyond the 3-month observation period is needed to assess the maintenance rate of nipple projection over a longer-term period.
Our nipple reconstruction method using a C-V flap overgrafted with AlloDerm® has demonstrated good results (73.14%) as assessed by maintenance of nipple projection at a 3-month follow-up, although a smaller AlloDerm® section was used in our study in comparison to other studies [5,8]. In the breast implant group, nipple projection was better maintained than in the autologous flap group. We believe that this is because the base of the nipple supported by the breast mound was firmer in the breast implant group than in the autologous tissue flap group, such that it was able to overcome external compression caused by a brassiere.
In conclusion, our method is easy to implement, and focuses on better retention of the ADM as a volume enhancer of the thin skin flap. In this method, the dermal matrix is overgrafted onto the undersurface of the flap for secure integration of the ADM in order to overcome the contracture of the skin flap.
ACKNOWLEDGMENTS
This article was presented at the 74th Congress of the Korean Society of Plastic and Reconstructive Surgeons on November 17ŌĆō20, 2016 in Seoul, Korea.
Fig.┬Ā1.
Operative technique of nipple reconstruction with a C-V flap overgrafted with AlloDerm┬«. (A) After the skin flap was elevated, a 1.5 ├Ś 1.5 cm section of AlloDerm┬« was securely grafted to the inner surface of the elevated C-V flap with #5-0 VicrylŌäó sutures. (B) The skin flap reinforced with AlloDerm┬« was wrapped and fixed with #5-0 nylon sutures. (C) Schematic illustration of our technique.

Fig.┬Ā2.
Average projection maintenance immediately postoperatively, at 3 weeks postoperatively, and at 3 months postoperatively. SD, standard deviation.
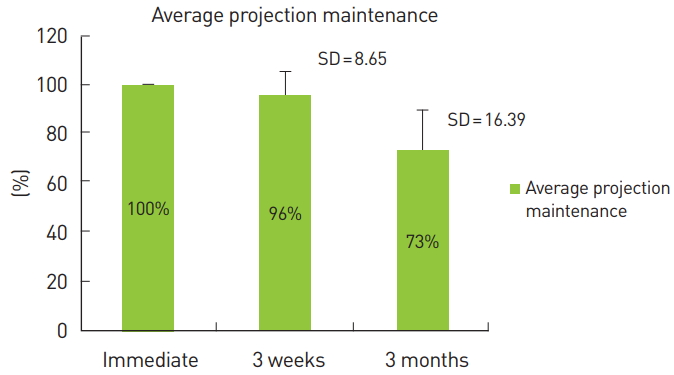
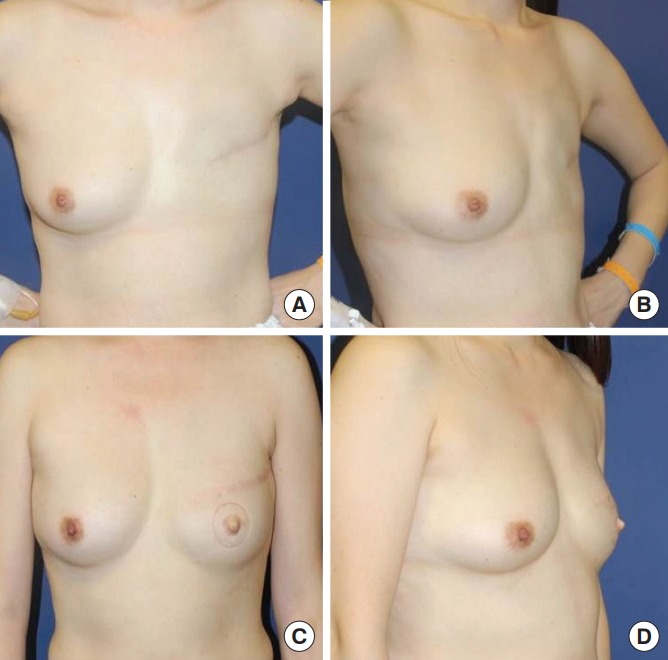
Fig.┬Ā3.
Case 1 (Patient 13 in Table 1). (A) View at 3 weeks postoperatively. (B) View at 3 months postoperatively.
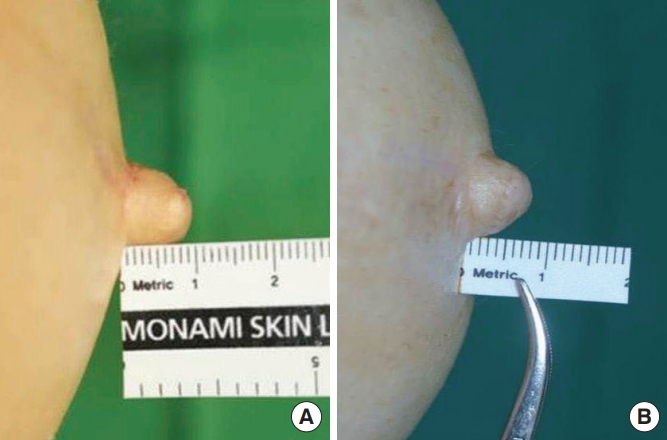
Fig.┬Ā4.
Case 2 (Patient 3 in Table 1). (A) View at 3 weeks postoperatively. (B) View at 3 months postoperatively.
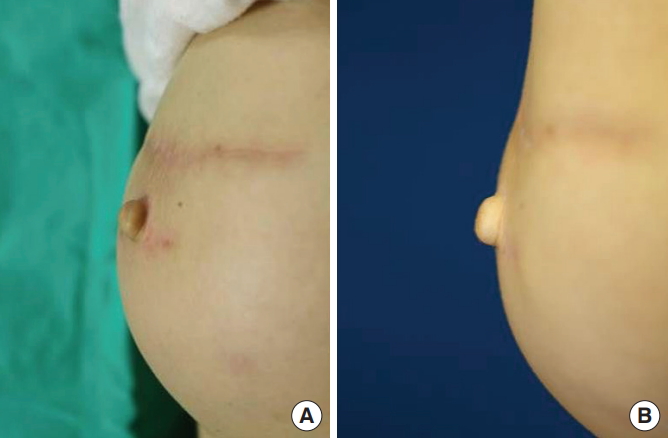
Fig.┬Ā5.
Case 3 (Patient 8 in Table 1). (A) Frontal view at 3 weeks preoperatively. (B) Oblique view at 3 weeks preoperatively. (C) Frontal view at 3 months postoperatively. (D) Oblique view at 3 months postoperatively.
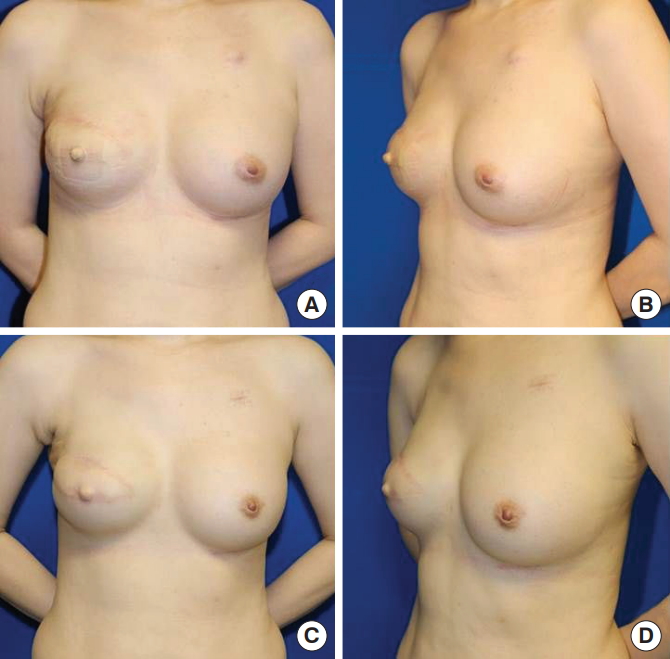
Fig.┬Ā6.
Case 4 (Patient 12 in Table 1). (A) Preoperative frontal view. (B) Preoperative oblique view. (C) Frontal view at 3 weeks postoperatively. (D) Oblique view at 3 weeks postoperatively.
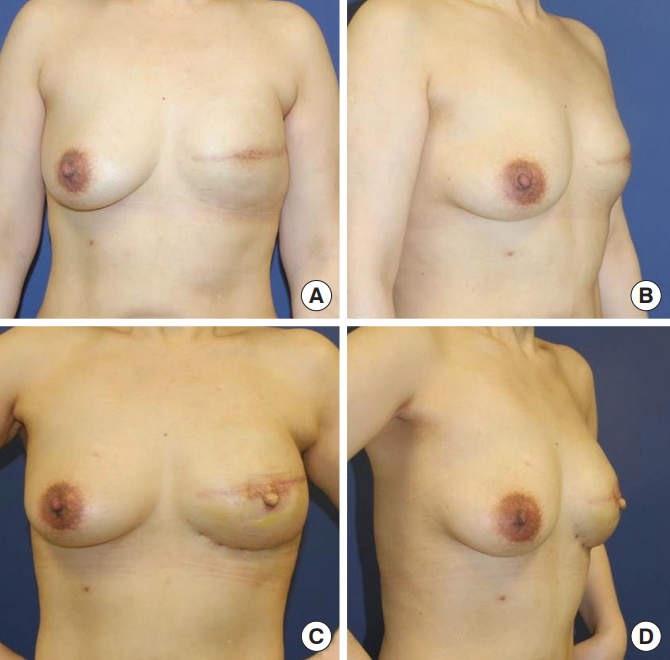
Fig.┬Ā7.
Case 5 (Patient 3 in Table 1). (A) Preoperative frontal view. (B) Preoperative oblique view. (C) Frontal view at 6 months postoperatively. (D) Oblique view at 6 months postoperatively.
Table┬Ā1.
Results of nipple projection during 3 months of follow-up
REFERENCES
1. Mori H, Uemura N, Okazaki M. Nipple reconstruction with banked costal cartilage after vertical-type skin-sparing mastectomy and deep inferior epigastric artery perforator flap. Breast Cancer 2015;22:95-7.


2. Yanaga H. Nipple-areola reconstruction with a dermal-fat flap: technical improvement from rolled auricular cartilage to artificial bone. Plast Reconstr Surg 2003;112:1863-9.


3. Bernard RW, Beran SJ. Autologous fat graft in nipple reconstruction. Plast Reconstr Surg 2003;112:964-8.


4. Chia HL, Wong M, Tan BK. Nipple reconstruction with rolled dermal graft support. Arch Plast Surg 2014;41:158-62.



5. Nahabedian MY. Secondary nipple reconstruction using local flaps and AlloDerm. Plast Reconstr Surg 2005;115:2056-61.


6. Losken A, Mackay GJ, Bostwick J 3rd. Nipple reconstruction using the C-V flap technique: a long-term evaluation. Plast Reconstr Surg 2001;108:361-9.


7. Guerra AB, Khoobehi K, Metzinger SE, et al. New technique for nipple areola reconstruction: arrow flap and rib cartilage graft for long-lasting nipple projection. Ann Plast Surg 2003;50:31-7.


8. Garramone CE, Lam B. Use of AlloDerm in primary nipple reconstruction to improve long-term nipple projection. Plast Reconstr Surg 2007;119:1663-8.


9. Chia HL, Wong M, Tan BK. Nipple reconstruction with rolled dermal graft support. Arch Plast Surg 2014;41:158-62.









