|
 |
- Search
| Arch Aesthetic Plast Surg > Volume 24(1); 2018 > Article |
|
Abstract
Ectropion is characterized by eversion of the eyelid margin and exposure of the cornea and conjunctiva. This leaves the inner eyelid surface exposed and prone to irritation, and in severe cases, poor eye closure. Ectropion can occur for several reasons including congenital malformations, trauma, burns, anti-cancer medications, allergies, and inappropriate eyelid surgery. Surgical treatments usually include local flaps or skin grafts, depending on the severity of the defect. We present a case of successful cicatricial upper eyelid ectropion correction using a dermofat graft and an anti-adhesive agent (Guardix-Sol) after the wide release of tethering scar tissue.
Cicatricial ectropion occurs when any factor shortens the anterior lamella of the lid. Such factors include congenital malformations, trauma, burns, allergies, medications, and inappropriate eyelid surgery [1]. Eventually, ectropion can lead to chronic conjunctivitis, keratitis, corneal ulceration, and lagophthalmos, with symptoms of tearing, photophobia, pain, and foreign body sensation [2]. The treatment of eyelid ectropion is challenging due to the anatomical complexity of the area and often requires surgical interventions including skin grafts and local flaps. Although these modalities can result in correction, recurrence can occur, necessitating more extensive and aggressive surgery. We present a case of the successful correction of cicatricial ectropion of the upper eyelid using a dermofat graft and an anti-adhesive agent (Guardix-Sol; Hanmi Medicare, Seoul, Korea).
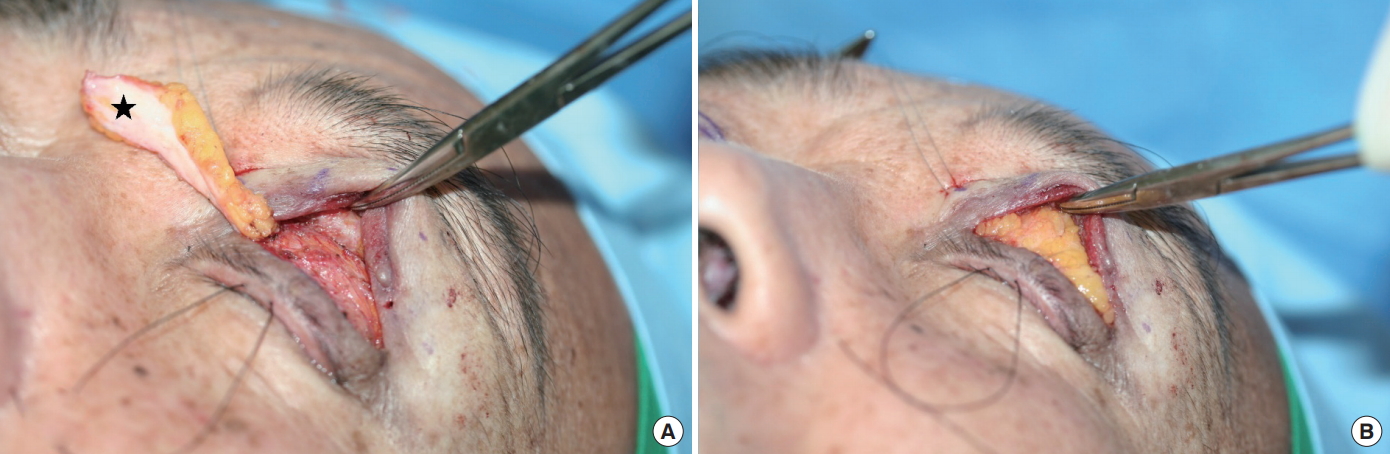
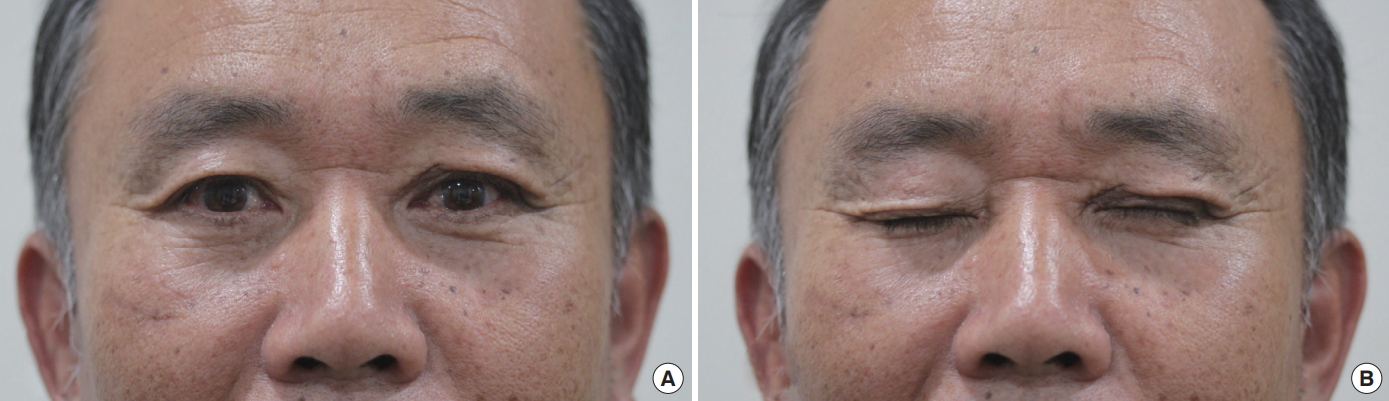
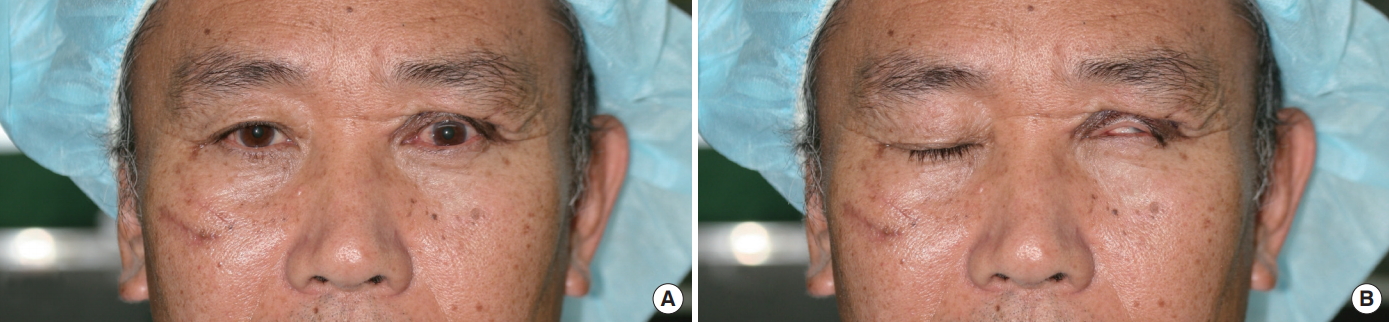
A 60-year-old Asian male patient presented with poor eye closure and ipsilateral forehead pain when eye closure was forced. He had suffered a deep muscle layer laceration at the left upper eyelid in a traffic accident 1 month prior and had undergone primary closure at the local emergency department. Due to the retraction caused by the scar tissue, his left eyeball was exposed by about 4 mm when both eyes were closed (Fig. 1). The patient suffered from subsequent ocular redness and irritation due to poor lid-globe apposition. To correct the severe cicatricial upper eyelid ectropion, we performed scar release with a dermofat graft under local anesthesia. First, an incision was made at the supratarsal crease, and the scar tissue throughout the orbicularis oculi muscle and levator aponeurosis and tarsal plate was completely dissected and released from the upper lid to the ipsilateral suprabrow area. A skin graft was unnecessary since our patient had sufficient upper eyelid skin. To prevent the recurrence of lid retraction, a 2├Ś5-cm area of dermofat was harvested from the patientŌĆÖs right axilla. The dermofat was de-epithelized and trimmed to an appropriate thickness according to the fat pad volume of the opposite upper lid for a symmetric appearance. We inserted the dermofat into the plane between the orbicularis oculi muscle and levator aponeurosis with its dermal layer facing down. The dermofat was fixed with pull-out sutures at 3 points (Fig. 2). After applying Guardix-Sol, an anti-adhesive agent, beneath the dermofat, a silastic drain was inserted into the same layer, and a continuous skin suture was made with 6-0 nylon. Minimal dressing was performed to induce blinking as an early exercise. The pull-out and skin sutures were removed 5 days postoperatively without any specific complications. At a 3-month follow-up visit, lid retraction had not recurred, and symmetric appearance was well maintained both when the eyes were closed and opened (Fig. 3).
Upper lid retraction is defined as a margin reflex distance 1 (MRD1) (the linear distance between the pupil center and the edge of the upper lid margin) greater than 5 mm. It can be more precisely classified according to severity: mild (MRD1Ōēż5 mm), moderate (MRD1 >5 to <7 mm), and severe (MRD1Ōēź7 mm) [3,4]. Along with the significant cosmetic deformity, patients with upper lid retraction suffer from dry eye or keratitis due to ocular surface exposure, which produces a considerable negative impact on quality of life.
Cicatricial ectropion is usually corrected by surgical intervention. Various surgical procedures can be performed; however, replacement modalities have to be used, such as skin grafts or local flaps, because of the lack of skin and subcutaneous tissue [5-7]. Autologous dermofat grafts are an effective surgical option for the correction of eyelid retraction [8]. To prevent the recurrence of ectropion, complete dissection of the scar tissue is essential. Therefore, if the surgeon believes that enough dissection has been performed, eye closing movements should be tested during the surgical procedure to determine whether the eye can be closed gently without excessive effort. Grafted dermofat and an anti-adhesive agent act as a physical barrier averting secondary contracture and the recurrence of ectropion. Recently, nonsurgical treatments using hyaluronic acid filler or fibrin tissue glue have been suggested for the correction of cicatricial ectropion [9,10].
After traumatic injury, the damaged site releases vasoactive factors and causes the accumulation of inflammatory cells, leading to collagen-rich vessel formation and the infiltration of fibroblasts, macrophages, and giant cells. This adhesion process eventually replaces the damaged tissues with angiogranular tissues, and the adhesion becomes permanent [11]. The anti-adhesive agent Guardix-Sol, a mixed solution of sodium hyaluronate and sodium carboxymethylcellulose, acts as a physical barrier to prevent this adhesion process. The ability of this mixture to maintain a physical barrier within the tissue enables the adequate prevention of post-traumatic adhesions [12-15]. In the authorsŌĆÖ experience, use of Gardix-SG (Hanmi Medicare) alone could not prevent the recurrence of adhesion. Therefore, Gardix-Sol was combined with a dermofat graft for a wide adhesion.
In conclusion, we successfully corrected severe cicatricial upper eyelid ectropion with a dermofat graft and Guardix-Sol without the recurrence of adhesion. Compared to other flap operations, the use of a dermofat graft is relatively simple and can efficiently prevent adhesion after the total release of traumatic scar tissue at the upper eyelid. It also provides an adequate range of volume for the upper eyelid and leads to an aesthetically satisfactory, symmetrical result.
Fig.┬Ā1.
Preoperative photography. (A) Frontal view with both eyes open. (B) Poor eye closure due to severe retraction of the left upper eyelid.
REFERENCES
2. Cruz AA, Menezes FA, Chaves R, et al. Eyelid abnormalities in lamellar ichthyoses. Ophthalmology 2000;107:1895-8.


3. Elner VM, Hassan AS, Frueh BR. Graded full-thickness anterior blepharotomy for upper eyelid retraction. Arch Ophthalmol 2004;122:55-60.


4. Ben Simon GJ, Mansury AM, Schwarcz RM, et al. Transconjunctival M├╝ller muscle recession with levator disinsertion for correction of eyelid retraction associated with thyroid-related orbitopathy. Am J Ophthalmol 2005;140:94-9.

5. Rathore DS, Chickadasarahilli S, Crossman R, et al. Full thickness skin grafts in periocular reconstructions: long-term outcomes. Ophthal Plast Reconstr Surg 2014;30:517-20.


6. Li XQ, Wang JQ. Orbicularis oculi myocutaneous flap for upper cicatricial ectropion. J Craniofac Surg 2016;27:70-3.


7. Sarici M, Ye┼¤ilo─¤lu N, G├╝vercin E, et al. Superficial temporal artery Island flap for cicatricial ectropion. J Craniofac Surg 2015;26:e457.

8. Yoon MK, McCulley TJ. Autologous dermal grafts as posterior lamellar spacers in the management of lower eyelid retraction. Ophthal Plast Reconstr Surg 2014;30:64-8.


9. Fezza JP. Nonsurgical treatment of cicatricial ectropion with hyaluronic acid filler. Plast Reconstr Surg 2008;121:1009-14.


10. Osborne SF, Eidsness RB, Carroll SC, et al. The use of fibrin tissue glue in the repair of cicatricial ectropion of the lower eyelid. Ophthal Plast Reconstr Surg 2010;26:409-12.


11. Hellebrekers BW, Trimbos-Kemper TC, Trimbos JB, et al. Use of fibrinolytic agents in the prevention of postoperative adhesion formation. Fertil Steril 2000;74:203-12.


12. Gago LA, Saed GM, Chauhan S, et al. Seprafilm (modified hyaluronic acid and carboxymethylcellulose) acts as a physical barrier. Fertil Steril 2003;80:612-6.


13. Kimmelman CP, Edelstein DR, Cheng HJ. Sepragel sinus (hylan B) as a postsurgical dressing for endoscopic sinus surgery. Otolaryngol Head Neck Surg 2001;125:603-8.


-
METRICS

-
- 0 Crossref
- 5,022 View
- 133 Download
- Related articles in AAPS
-
Correction of sunken upper eyelid using dermofat graft.2000 March;6(1)
Correction of Sunken upper Eyelids Using Autologous Microfat Graft.2006 March;12(1)
Correction of Upper Lid Entropion in Childhood.2007 March;13(1)
Correction of Dark Coloration of the Lower Eyelid Skin with Nanofat Grafting.2014 June;20(2)