|
 |
- Search
| Arch Aesthetic Plast Surg > Volume 27(4); 2021 > Article |
|
Abstract
Conventional abdominoplasty includes the removal of an ellipse-shaped section of abdominal tissue between the umbilicus and mons pubis. However, this method can result in tension of the undermined flap, especially in the midline. To address this problem, we present reverse lip design as a modified method that also has aesthetic advantages. The reverse lip design entails a longer lower flap edge while preserving the triangular tissue in the vascularly stable pubis area. These markings create an image of a reverse lip shape with a cleft at the bottom of the lower markings. After typical lipoabdominoplasty is performed, redundant waist tissues can easily be pulled inward and downward. The reverse lip design abdominoplasty demonstrated no complications and required no further revisions after the procedure. Patients were generally satisfied with the aesthetic improvements in their body shape. They were also able to return to their routine activities approximately 1 week after the operation while wearing a supporting undergarment. This modified abdominoplasty using the reverse lip design reduces low midline tension of the undermined abdominal flap while enhancing body aesthetics with a slimmer waistline, leading to higher patient satisfaction.
Conventional abdominoplasty includes the removal of an ellipseshaped section of abdominal tissue between the umbilicus and mons pubis (Fig. 1A) [1]. This approach generally works in patients with a very large pannus, in which the excision markings could be placed above the pubic hairline to close the wound. However, this procedure often requires tight closure; therefore, the mons pubis may be superiorly retracted, leading to an unnaturally flat hypogastrium and an exaggerated rate of wound dehiscence and skin necrosis, especially in the midline [1,2].
Due to these potential complications, in the early 1990s, Lockwood reported high lateral tension abdominoplasty (HLTA), which involves conservative undermining of the central skin flap only to facilitate plication and the use of a controlled high lateral-tension closure. The pubis is then closed under mild tension and rests in a lower, more inconspicuous location [3]. However, one possible complication of this method is ischemia in the central midline region, due to simultaneous extensive suction-assisted lipoplasty (SAL) [3]. Furthermore, the procedure runs the risk of a vertical scar that can occasionally occur when closing the original umbilical site.
Therefore, we propose an enhanced reverse lip design that circumvents these problems while providing improved aesthetic advantages.
From September 2016 to November 2019, 37 abdominoplasty procedures were performed, which were divided into two groups: 18 of 37 patients underwent reverse lip design abdominoplasty (RLDA) and 19 of 37 patients underwent HLTA.
RLDA was performed as follows. The assumed edges of the patient’s typical garments were marked in standing position, and the length of the abdominoplasty incisions was determined by placing a mark on either side. The surgeon joined these lateral marks, with the lowest position, approximately less than 5 cm above the inguinal crease, and the midline position less than 10 cm above the vulvar cleft (Fig. 1B). The central area of the lower incision was generally designed lower than the location of the cesarean section incision (if present) or included the upper line of the pubic hair so that the postoperative scar could be hidden by the pubic hair. These markings created an image of a reverse lip shape, with a cleft at the bottom of the lower markings. If liposuction was required, an incision for liposuction was first made on the abdominal tissue to be excised later. After liposuction, the upper abdominal flap was elevated and plication of rectus fascia was performed at the midline or both lateral sides depending on diastasis of the fascia. After lipoabdominoplasty, redundant waist tissues were easily pulled inward and downward, creating a slimmer waistline. At this time, by adjusting the position of the flap using a towel clamp, the dog ears on both lateral sides were minimized. The reverse lip design can be applied to mini-abdominoplasty using the same principles.
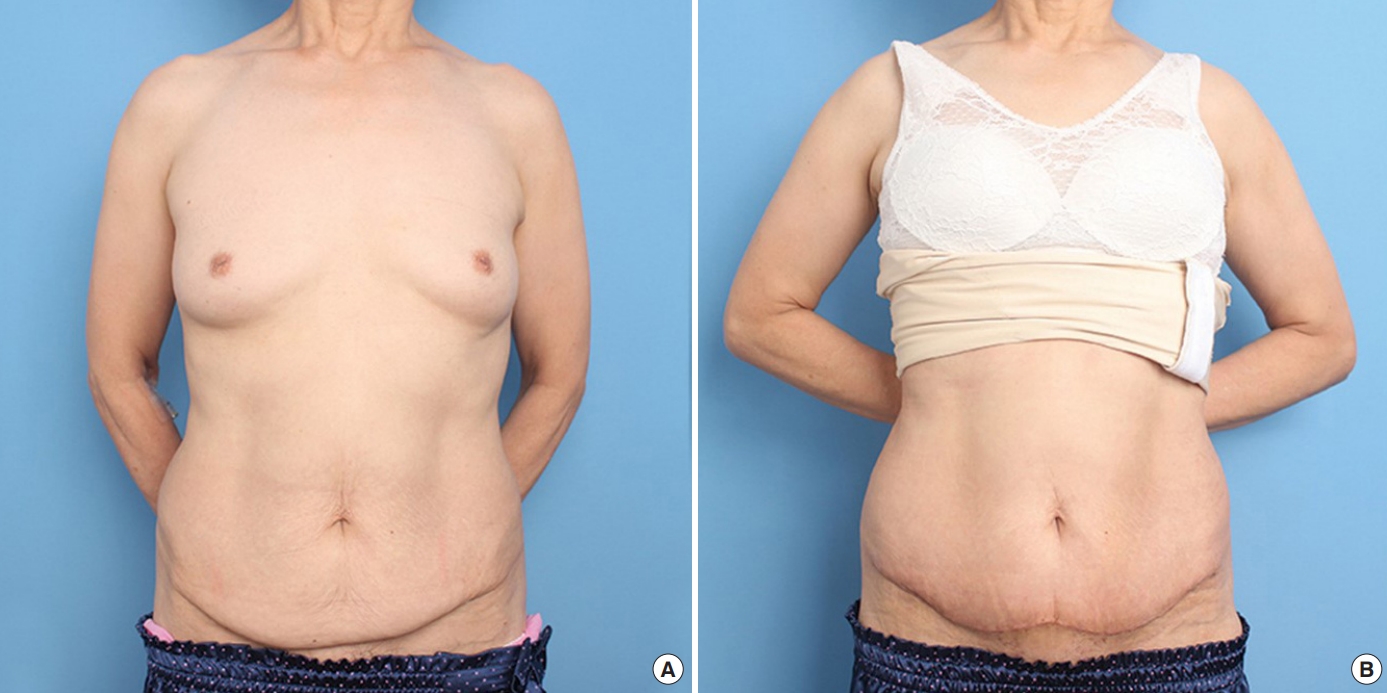
All patients undergoing the procedure were women (average age, 38 years; range, 28–60 years). The follow-up periods ranged from 12 to 24 months. In our clinical cases, the modified procedure with reverse lip design led to no complications requiring further revisions. By contrast, the conventional procedure used in the HLTA group led to two cases of skin necrosis and wound dehiscence. Furthermore, the RLDA resulted in enhanced aesthetic outcomes (Figs. 2, 3). Patients were also generally satisfied with the procedure’s outcomes and aesthetic improvements. Patients were able to return to their routine activities approximately 1-week postoperation while wearing a supporting undergarment.
Conventional abdominoplasty can lead to unwanted tension of the undermined flap in the midline, especially when liposuction is performed simultaneously [4-7]. Matarasso et al. described the suction area as a concept, demonstrating the abdominal wall blood supply superimposed on areas of undermining [8,9]. The suction area indicates the origin of the lateral intercostal blood supply that perfuses the abdominoplasty flap. The undermining area exhibits random patterns in the perfused areas of liposuction. Namely, suction area 3, which is located in the upper umbilicus area, is the “terrible abdominoplasty triangle,” where ischemia is most likely to occur. One patient who suffered from ischemia in this area was a 38-year-old female patient who underwent modified HLTA with SAL. Suprafascial dissection was performed, and the patient seemed to have no problem initially. However, signs of skin necrosis emerged on the midline of the lower abdomen 4 days after the operation. After 25 days of conservative management, the necrotic tissue was removed, and the defect was repaired using a Limberg local flap. This prolonged convalescence and increased scarring necessitate a design modification to address these issues [10-12]. Thus, we proposed a more stable method that preserves the pubic area, which has a more stable blood supply than suction area 3 (used in the HLTA design) and reduces midline tension.
Compared to conventional abdominoplasty, the reverse lip design of abdominoplasty is characterized by a decreased midline vector and greater tension on the lateral side. Generally, since the outcomes of surgery improve as more vectors of excess are addressed [13,14], these oblique vectors in the reverse lip design treat the more horizontal excess in the epigastrium.
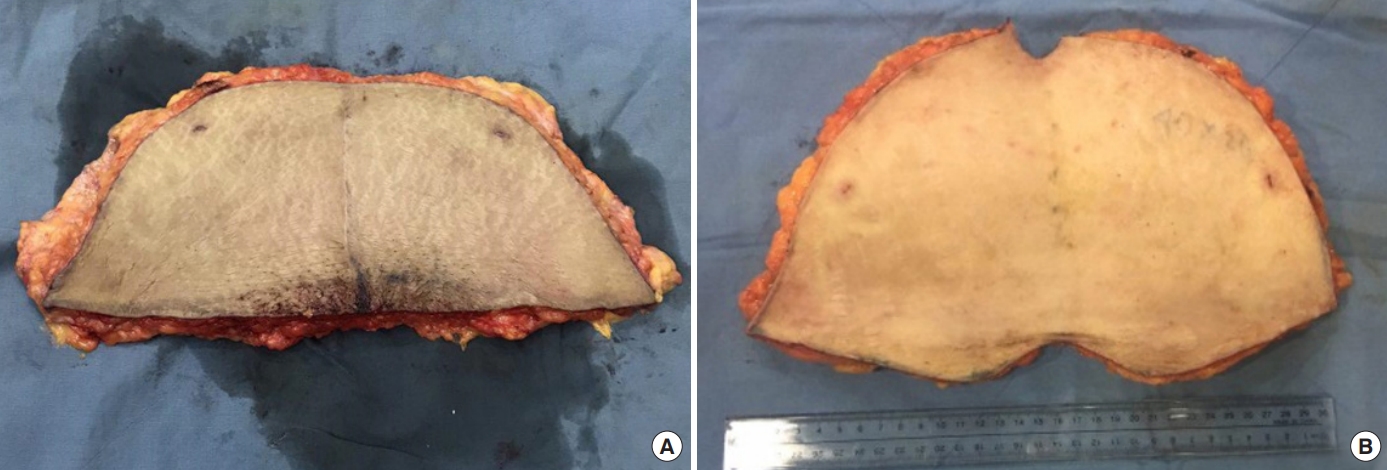
In addition, in HLTA and conventional abdominoplasty, the superior wound edge is always longer than the inferior one. By contrast, as demonstrated in the excised abdominal tissue of RLDA, the superior wound edge is not longer than the inferior edge due to its concave area, as it normally would be in the conventional method (Fig. 4).
In the reverse lip design, preserving more pubic area tissue has many advantages. Preserving more pubic area tissue provides a more stable blood supply than in the undermined epigastric area, which has a random blood supply. Furthermore, wound closure is easier, and it is less likely to lead to the incidence of dog ears, as the superior wound edge is not longer than the inferior one. The design also leads to a more natural pubic area than is achieved using HLTA or other conventional abdominoplasty techniques that directly remove an upper portion of the pubic hair region.
In conclusion, RLDA minimizes ischemic problems by reducing the low midline tension of the undermined abdominal flap that can occur in conventional abdominoplasty. The modified design also involves a scar that can be more effectively concealed in lower regions, without creating a vertical scar, as is often the case in HLTA. Finally, the reverse lip design can be applied to mini-abdominoplasty or any type of comprehensive abdominoplasty using the same principles, demonstrating the procedure’s versatility in multiple surgical settings.
Notes
Ethical approval
The study was approved by the Institutional Review Board of Pusan National University Hospital (IRB No. 2105-035-103).
Patient consent
The patients provided written informed consent for the publication and the use of their images.
Fig. 1.
Abdominoplasty design. (A) Conventional full abdominoplasty. (B) Reverse lip full abdominoplasty. SAL, suction-assisted lipoplasty.
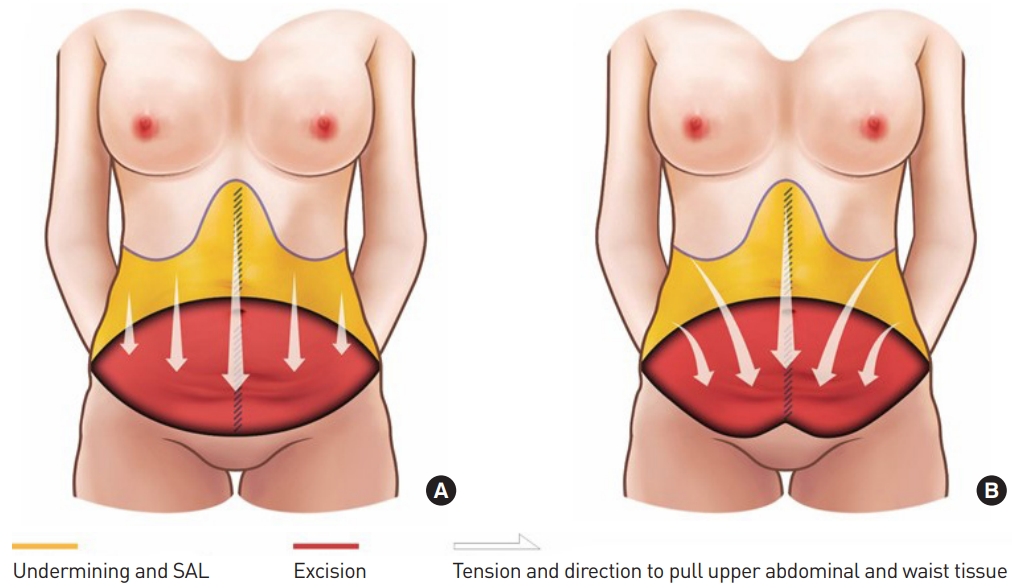
Fig. 2.
A case of reverse lip full abdominoplasty. (A) A 37-year-old female patient underwent reverse lip design lipoabdominoplasty due to stretch marks after delivery. An abdominal excision measuring 27×12 cm was performed, as well as periumbilical tissue excision. (B) A follow-up photograph on postoperative day 17.
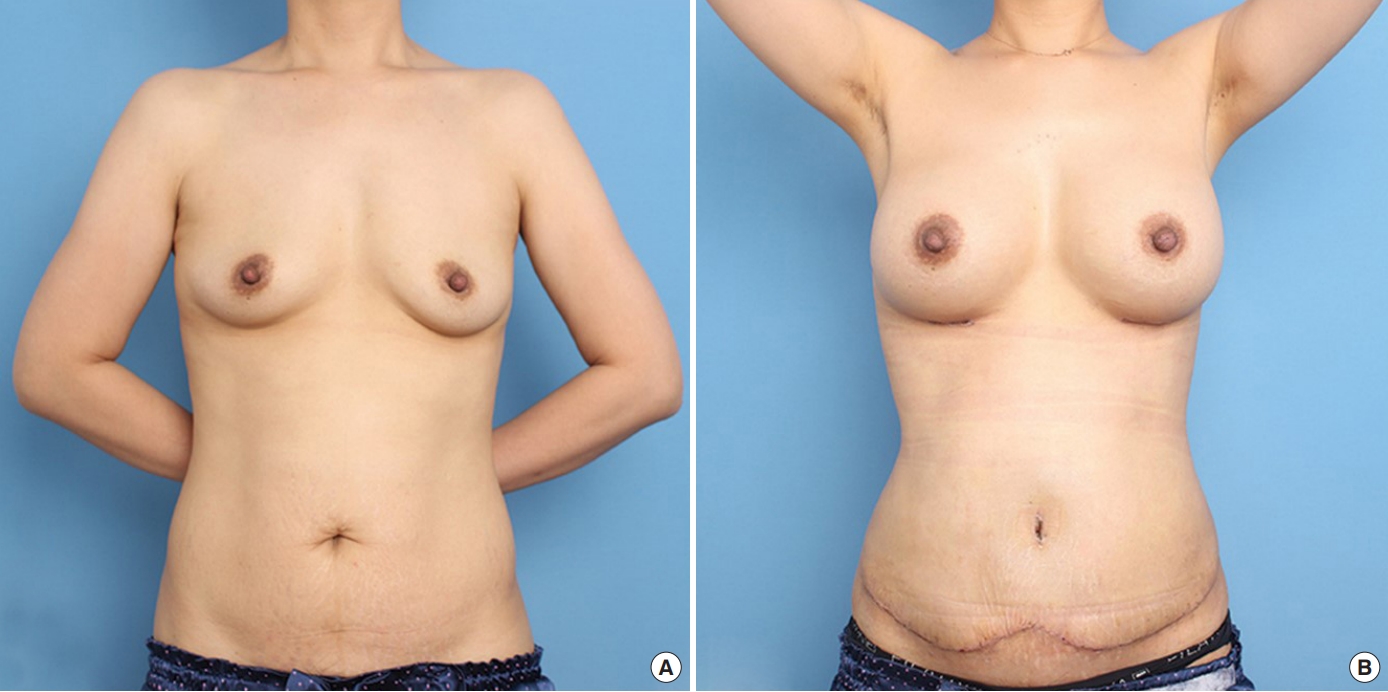
Fig. 3.
A case of a reverse lip mini-abdominoplasty. (A) A 60-year-old woman with a history of a cesarean section and hysterectomy underwent reverse lip design mini-abdominoplasty. A 26×10 cm section of the lower abdomen tissue was removed, including the cesarean section scar. (B) A photograph at follow-up on postoperative day 10.
REFERENCES
1. Pitanguy I. Abdominal lipectomy: an approach to it through an analysis of 300 consecutive cases. Plast Reconstr Surg 1967;40:384-91.

2. Matarasso A. Abdominolipoplasty: a system of classification and treatment for combined abdominoplasty and suction-assisted lipectomy. Aesthetic Plast Surg 1991;15:111-21.

3. Lockwood T. High-lateral-tension abdominoplasty with superficial fascial system suspension. Plast Reconstr Surg 1995;96:603-15.


4. Matarasso A. Liposuction as an adjunct to a full abdominoplasty revisited. Plast Reconstr Surg 2000;106:1197-202.


5. Swanson E. Prospective outcome study of 360 patients treated with liposuction, lipoabdominoplasty, and abdominoplasty. Plast Reconstr Surg 2012;129:965-78.


6. Heller JB, Teng E, Knoll BI, et al. Outcome analysis of combined lipoabdominoplasty versus conventional abdominoplasty. Plast Reconstr Surg 2008;121:1821-9.


7. Buck DW 2nd, Mustoe TA. An evidence-based approach to abdominoplasty. Plast Reconstr Surg 2010;126:2189-95.


8. Matarasso A, Matarasso DM, Matarasso EJ. Abdominoplasty: classic principles and technique. Clin Plast Surg 2014;41:655-72.

10. Manassa EH, Hertl CH, Olbrisch RR. Wound healing problems in smokers and nonsmokers after 132 abdominoplasties. Plast Reconstr Surg 2003;111:2082-7.


11. Lopez Q. Treatment of large skin necrosis following a modified avelar abdominoplasty with the Erchonia EML 635 nm laser and platelet-rich plasma. Am J Cosmet Surg 2019;26:29-34.

12. Flores Gonzalez EA, Perez Chavez F, Ramirez Guerrero OR, et al. A new surgical approach to body contouring. Plast Reconstr Surg Glob Open 2021;9:e3540.