|
 |
- Search
| Arch Aesthetic Plast Surg > Volume 28(4); 2022 > Article |
|
Abstract
Background
Acellular dermal matrix (ADM) is widely used for prosthetic breast reconstruction. Although many studies have investigated the efficacy and complications of ADM in prosthetic breast reconstruction, studies on drainage and seroma formation according to the size of ADM manufactured using the same process are lacking. This study analyzed drainage and seroma formation according to the size of sterile ADM.
Methods
From January 2011 to June 2018, the authors retrospectively reviewed the medical charts of patients who underwent direct-to-implant breast reconstruction using MegaDerm at a single institution. The ADMs used were classified as small or large groups. The two groups were compared in terms of the volume and duration time of two closed-suction drains (supramuscular and submuscular drains). Seroma and infection risk were also analyzed.
Results
Of 344 patients, 69 were included. Among them, 22 patients were in the small-ADM group and 47 patients were in the large-ADM group. The supramuscular drain volume (P=0.295) and time (P=0.365) were not significantly different between the two groups. However, the submuscular (P=0.001) and total drain volume (P=0.004) were higher in the large-ADM group. In addition, seroma occurred significantly more frequently in the large-ADM group (P=0.048), but there was no significant difference in minor infections (P=0.088).
Acellular dermal matrix (ADM) is widely used in direct-to-implant (DTI) breast reconstruction. ADM reduces the burden on the skin by reinforcing the mastectomy skin flap, promoting vascularization, and improving the overall cosmetic outcome by enhancing the position and definition of the inframammary fold. In addition, ADM reduces capsular contracture induced by breast implants. ADM was first used for breast reconstruction in 2005 [1], and it has subsequently become the primary choice for reconstruction. As a result, many manufacturers are producing large ADMs that cover a wider surface than in the past [2].
ADM is derived from human cadavers, with all cellular and antigenic components removed, and it can be classified as ŌĆ£asepticŌĆØ or ŌĆ£sterileŌĆØ according to the processing method. Aseptic ADM minimizes contamination during ADM processing; however, no sterility assurance level (SAL) is associated with aseptic processing. The most well-known aseptic ADM product is AlloDerm (LifeCell Corp., Branchburg, NJ, USA). It undergoes a freeze-drying process under aseptic conditions, and it is currently the most frequently used ADM for breast reconstruction by plastic surgeons. In contrast, sterile ADM undergoes a terminal sterilization process validated to a SAL of 10ŌĆō6. A typical example of a sterile ADM is MegaDerm (L&C BIO, Seongnam, Korea), which has been introduced recently. MegaDerm undergoes electron-beam sterilization to remove viruses, bacteria, and spores [3].
With the increased use of ADMs for implant-based breast reconstruction, many studies have investigated complications related to ADM use [4-6]. Several studies have reported that ADM use increased the risk of infection and seroma formation, but this remains a matter of debate. In addition, ADMs are made by various manufacturing processes, and ADMs of various sizes are used, but studies analyzing the effect of ADM on breast reconstruction that consider this heterogeneity are limited.
The authors hypothesized that the drainage amount might be different depending on the ADM manufacturing process and the size of the area where the ADM contacts the flap, and that the risk of seroma might increase with increasing drainage volume and drain time. Therefore, only sterile ADM was included in the present study, and the amount of drainage according to the size of the ADM was analyzed.
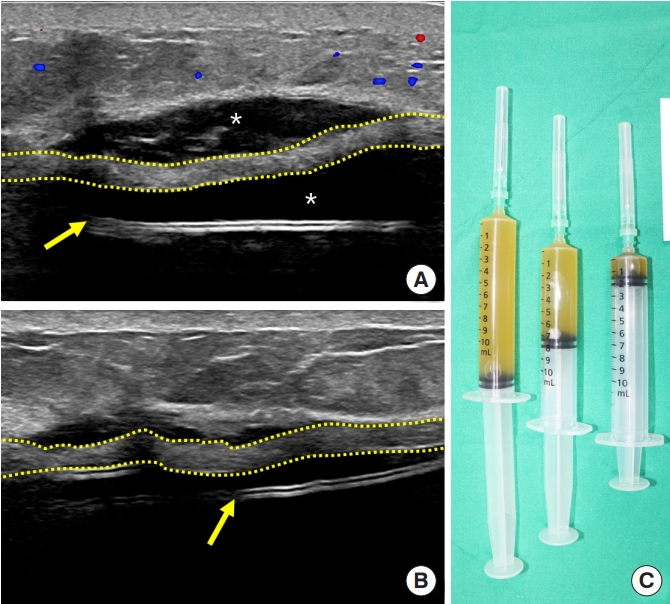
Our study was reviewed and approved by the Institutional Review Board of Yeungnam University Hospital. A retrospective medical chart review from January 2011 to June 2018 of patients who underwent DTI breast reconstruction at a single center was done. Among patients who underwent DTI breast reconstruction, only those who underwent the procedure with the submuscular approach with MegaDerm, a sterile ADM, were included. Only textured silicone gel implants (Allergan Corp., Irvine, CA, USA) were used for breast implants, and tissue expanders were excluded. Patients who received neoadjuvant radiation therapy, those whose follow-up period was less than 6 months, those with severe comorbidities (metastatic cancer, chronic kidney disease, uncontrolled diabetes, and immunocompromised state), and those who used fenestrated ADMs were also excluded. Patients who underwent reoperations were also excluded, as the drain volume could have been affected (Table 1). Only cases of seroma and minor infections were included for analysis to assess postoperative complications. An infection was defined as having erythematous changes in the breast, fever, or increased C-reactive protein levels compared with the previous level. Those whose symptoms could be controlled using oral or intravenous antibiotics were classified as minor infections and were included in the analysis. Infections not controlled by antibiotics were classified as major infections, and reoperation (such as irrigation or implant change) was performed. Major infections were excluded from the analysis because reoperation affected the drainage. Seroma was defined as a condition requiring ultrasound-guided aspiration after removal of both drains (Fig. 1). A suitable dose of second-generation cephalosporin antibiotics was administered intravenously before and after surgery, and the regimen was maintained for 10 days postoperatively.
The ADM size was determined by considering the implant size, breast ptosis, and chest wall size. The trimmed ADM was fixed along the inferior border of the pectoralis major muscle superiorly, the inframammary fold inferiorly, and the serratus anterior fascia laterally. In addition, all trimmed ADM pieces were used, so that no ADM was discarded.
Two closed-suction drains were inserted. One was the supramuscular drain, placed between the pectoralis major muscle and mastectomy skin flap, and the other was the submuscular drain, placed between the implant and pectoralis major muscle. The drains were checked daily and removed if the drainage volume was less than 20 mL/day, for 2 consecutive days. Patients who were discharged with the drains had to visit the hospital twice a week, and the drains were removed based on the above conditions by referring to the self-reported drainage volume.
The patients were divided into two groups according to the size of ADM to investigate the differences in drainage volume and drain duration according to ADM size. ADMs with dimensions of 4├Ś12 cm and 4├Ś16 cm were classified as the small-ADM group, while those with dimensions of 6├Ś16 cm and 7├Ś18 cm were classified as the large-ADM group. The risks of seroma and minor infection in the two groups were compared.
The t-test, Pearson chi-square test, and Fisher exact test were used to compare the results between the groups. Linear regression analysis was performed to evaluate the correlation between each variable and total drain volume by adjusting for variables that could affect drainage. Statistical analyses were conducted using SPSS version 26 (IBM Corp., Armonk, NY, USA), and the statistical significance level was set at P<0.05.
In total, 344 patients underwent DTI breast reconstruction from January 2011 to June 2018. After excluding those who received neoadjuvant radiation therapy, who underwent reoperations, whose follow-up period was less than 6 months, and who had severe comorbidities and received fenestrated ADMs, 248 patients remained. Of those patients, 69 had received MegaDerm, with 22 patients in the small (4├Ś12 cm or 4├Ś16 cm) group and 47 in the large (6├Ś16 cm or 7├Ś18 cm) group.
The two groups showed similar characteristics in terms of age, body mass index, comorbidities, mastectomy volume, implant size, adjuvant chemotherapy, hormone therapy, and nipple-sparing mastectomy (Table 2).
The supramuscular drain volume was larger in the small-ADM group (137.2┬▒52.3 cc) than in the large-ADM group (118.3┬▒75.9 cc). However, the difference was not significant (P=0.295). In contrast, the submuscular drain volume in the large-ADM group (559.7 ┬▒213.2 cc) was significantly larger than that in the small-ADM group (387.8┬▒161.9 cc) (P=0.001). Similarly, the total drain volume, which is the sum of the two drains, was also larger in the large-ADM group (678.0┬▒242.9 cc) than in the small-ADM group (525.0 ┬▒170.5 cc) (P=0.004). The duration of the supramuscular drain was not significantly different between the two groups (P=0.365). However, the duration of the submuscular drain was significantly longer in the large-ADM group (16.7┬▒5.5 days) than in the small-ADM group (13.5┬▒4.0 days) (Table 3).
Seromas and minor infections occurred only in the large-ADM group. Seroma showed a statistically significant difference between the two groups (P=0.048), but minor infections did not (P=0.088).
In univariate linear regression analysis, mastectomy volume (P=0.004), implant size (P<0.001), and ADM size (P=0.010) showed positive correlations with total drainage volume. Multivariate linear regression analysis confirmed that implant size (P=0.043) and ADM size (P=0.017) were positively correlated with total drain volume (Table 4).
ADM is derived from human cadavers, with all the cellular and antigenic components removed. This matrix comprises collagen, fibronectin, elastin, hyaluronan, and proteoglycans. Upon implantation, the structure serves as a scaffold for donor-side cells to facilitate incorporation and revascularization [7]. During revascularization, the implanted ADM becomes recolonized by fibroblasts, myofibroblasts, and other cells such as lymphocytes, macrophages, granulocytes, and mast cells of the connective tissue and is then activated by the immune response. It is considered that the growth factors produced at this stage induce progressive ADM angiogenesis to promote its local incorporation [8].
Although ADM is a nonantigenic and biocompatible material, it can trigger a physiologic foreign body reaction characterized by lymphocyte infiltration and macrophage activation. The interstitial fluid generated during this process is exuded to form a serous fluid, and the volume produced depends on the area of the ADM.
There are three main explanations for the formation of seroma following prosthetic breast reconstruction: (1) fluid accumulation due to exudation into the dead space induced by movement of the chest wall; (2) lymphatic disruption; and (3) ongoing inflammation [9]. To prevent seroma formation, a closed-suction drain is placed within the reconstruction site. The drain is removed when the drain volume decreases below a certain level as the dead space and inflammation decline due to adhesion. The criteria of drain removal differ slightly for different hospitals; however, the drain is usually removed when the volume is below 30 cc for 2 consecutive days. In this study, a stricter approach was adopted, and the drain was removed when the volume was below 20 cc for 2 consecutive days. Fluid accumulation may still occur even after the drain is removed following stricter control. However, small amounts of fluid can be absorbed due to the pressure gradient. Seroma can still form if fluid accumulates due to ongoing inflammation of the ADM. If the drain volume is too large or the drain duration is too long, excessive fluid formation due to ongoing inflammation of the ADM may be suspected, increasing the risk of seroma formation after the drain is removed.
The patients were divided into two groups (small and large) based on the size of ADM to determine the difference in the drainage for different ADM sizes. The dimensions of ADMs in the small-ADM group were 4├Ś12 cm and 4├Ś16 cm, while the size of ADMs in the large-ADM group were 6├Ś16 cm and 7├Ś18 cm. Since the comparison of the amount of drainage by ADM size is relative, the criteria for dividing the groups were based on the median of the largest and smallest ADMs. In this study, the large-ADM group showed a larger drain volume and longer drain duration than the small-ADM group. Seroma formation was also significantly more common in the large-ADM group. It is thought that fluid formation due to ongoing inflammation in large ADMs persisted for a long time even after the drain was removed, resulting in seroma.
The process of the ADM becoming integrated into the host tissue differs depending on the method of ADM preparation and type of ADM [10,11]. Furthermore, while ADMs are supposed to be devoid of cellular and antigenic components, it is challenging to eliminate them entirely during the manufacturing process in practice. Because there are differences in the ADM structure and cellular and antigenic components depending on the ADM preparation method, it is considered appropriate to analyze only ADMs manufactured using the same processes to accurately determine whether complications were associated with the ADM itself. Sterile ADMs undergo terminal sterilization to achieve a SAL of <10ŌĆō6. The SAL refers to the probability of a viable microorganism being present in the product after sterilization. A SAL of <10ŌĆō6 means that the probability of finding a non-sterile unit is 1 in 1,000,000; therefore, it could be used as a surgically implanted device. Among the sterile ADMs, we analyzed only MegaDerm that underwent electron-beam sterilization to eliminate viruses, bacteria, and spores without destroying the collagen tissue structure [12]. This study could not confirm whether MegaDerm is safer than other types of ADMs, but it did confirm that the drain volume and seroma incidence could increase if the MegaDerm implantation area increases.
Obesity, implant size, mastectomy volume, and preoperative irradiation are known to increase the risk of seroma formation during prosthetic breast reconstruction [13,14]. All these factors are supported by some clinical evidence, although none are considered conclusive. This study assumed that these factors might affect seroma formation and drainage. Therefore, patients who underwent radiation therapy were excluded from the analysis. Furthermore, since the two groups had statistically similar characteristics, it is unlikely that these variables affected the drain. Additionally, the authors performed multivariate linear regression analysis for a more precise analysis. Adjusting the variables that may affect the total drain volume showed that larger ADMs were associated with greater total drain volume. A positive correlation was also found between implant size and total drain volume. The wider area of contact of large implants with soft tissues is thought to exacerbate inflammation and thus increase fluid formation.
A large ADM is typically used when the mastectomy volume or implant size is large. However, there were no statistically significant differences in mastectomy volume or implant size between the two groups in our data This is thought to be because we considered the implant size, breast ptosis, and chest wall size in determining the ADM size.
Some limitations should be considered when interpreting the findings of this study. First, the width of the mastectomy skin flap has been found to be a significant factor in the wound healing process. However, this variable was not considered in this study as it could not be quantified. Second, the immune and inflammatory responses that occur with ADM were not pathologically analyzed. Performing biopsies on human patients would be challenging; therefore, laboratory animal testing would be required for a future analysis.
Nevertheless, the findings of this study are significant in that for patients who underwent immediate breast reconstruction through a subpectoral approach using only sterile ADMs, the drainage volume and drain duration for different ADM sizes were analyzed to investigate the effect of ADM size on seroma formation and the occurrence of infections.
The benefits of using ADMs in prosthetic breast reconstruction have been reported, and with the increasing popularity of prepectoral approaches, the size of ADMs used by plastic surgeons is steadily increasing [15]. Considering this trend, our study could provide a clinical basis to promote the safe use of large ADMs. Keeping in mind that large ADMs could increase seroma formation or drain volume, it is better to keep the closed-suction drain less than 20 cc for a longer time, or to use prophylactic antibiotics for a sufficient duration.
Notes
Ethical approval
The study was approved by the Institutional Review Board of Yeungnam University Hospital (IRB No. 2020-12-047-002) and performed in accordance with the principles of the Declaration of Helsinki.
Patient consent
This study is a retrospective study using medical record review and so informed consent was waived.
Fig.┬Ā1.
Ultrasound-guided aspiration was conducted for a seroma that formed during the fourth week after direct-to-implant breast reconstruction. (A) Acellular dermal matrix (yellow dotted line) is separated from the mastectomy skin flap and breast implant shell (yellow arrow), and seroma (asterisks) formation can be seen. (B) Ultrasound image after aspiration. (C) The total aspiration volume was 23 cc.
Table┬Ā1.
Exclusion criteria for the study population
Table┬Ā2.
Patient demographics and operative characteristics stratified by acellular dermal matrix size
Table┬Ā3.
Drain volume and duration by acellular dermal matrix size
Table┬Ā4.
Linear regression analysis between the total drain volume and variables
REFERENCES
1. Breuing KH, Warren SM. Immediate bilateral breast reconstruction with implants and inferolateral AlloDerm slings. Ann Plast Surg 2005;55:232-9.


2. Neamonitou F, Mylvaganam S, Salem F, et al. Outcome of complete acellular dermal matrix wrap with polyurethane implant in immediate prepectoral breast reconstruction. Arch Plast Surg 2020;47:567-73.




3. Lee JH, Park Y, Choi KW, et al. The effect of sterile acellular dermal matrix use on complication rates in implant-based immediate breast reconstructions. Arch Plast Surg 2016;43:523-8.




4. Tierney BP, De La Garza M, Jennings GR, et al. Clinical outcomes of acellular dermal matrix (SimpliDerm and AlloDerm Ready-to-Use) in immediate breast reconstruction. Cureus 2022;14:e22371.



5. Chun YS, Verma K, Rosen H, et al. Implant-based breast reconstruction using acellular dermal matrix and the risk of postoperative complications. Plast Reconstr Surg 2010;125:429-36.


6. Cayci C, Santner F, Jacobson SR. Impact and outcome of human acellular dermal matrix size for immediate and two-stage breast reconstruction. Plast Reconstr Surg 2013;132:11-8.


7. Bohac M, Danisovic L, Koller J, et al. What happens to an acellular dermal matrix after implantation in the human body? A histological and electron microscopic study. Eur J Histochem 2018;62:2873.


8. Garcia O Jr, Scott JR. Analysis of acellular dermal matrix integration and revascularization following tissue expander breast reconstruction in a clinically relevant large-animal model. Plast Reconstr Surg 2013;131:741e-751e.


9. Jordan SW, Khavanin N, Kim JY. Seroma in prosthetic breast reconstruction. Plast Reconstr Surg 2016;137:1104-16.


10. Capito AE, Tholpady SS, Agrawal H, et al. Evaluation of host tissue integration, revascularization, and cellular infiltration within various dermal substrates. Ann Plast Surg 2012;68:495-500.


11. Michelotti BF, Brooke S, Mesa J, et al. Analysis of clinically significant seroma formation in breast reconstruction using acellular dermal grafts. Ann Plast Surg 2013;71:274-7.


12. Lee JH, Kim HG, Lee WJ. Characterization and tissue incorporation of cross-linked human acellular dermal matrix. Biomaterials 2015;44:195-205.


13. Lim YM, Lew DH, Roh TS, et al. Analysis of factors that affect drainage volume after expander-based breast reconstruction. Arch Plast Surg 2020;47:33-41.




-
METRICS

-
- 0 Crossref
- 2,522 View
- 60 Download
- Related articles in AAPS
-
Usefulness of meshed SurgiMend in direct-to-implant breast reconstruction2021 April;27(2)