 |
 |
- Search
| Arch Aesthetic Plast Surg > Volume 28(4); 2022 > Article |
|
This article has been corrected. See Arch Aesthetic Plast Surg. 2023 Jan 30; 29(1): 59.
Abstract
Postmastectomy nipple necrosis is a factor that leads to a poor aesthetic outcome in breast reconstruction because of the unique projective structure of the nipple. We present a case of successful nipple reconstruction using a de-epithelialized rectangular flap. A 45-year-old woman was diagnosed with left breast cancer. She had a vertical scar below the nipple-areolar complex due to previous reduction mammoplasty. She underwent nipple-sparing mastectomy, breast reconstruction with a deep inferior epigastric artery perforator (DIEP) flap, and contralateral reduction. After the operation, the nipple gradually necrotized, and full-thickness nipple necrosis was observed on postoperative day 12. For nipple reconstruction, we designed a 38├Ś23 mm rectangular flap from the DIEP flap considering the contralateral nipple diameter (12 mm), protrusion (2 mm), and ipsilateral mastectomy skin flap thickness (15 mm). The area in contact with the mastectomy skin flap was placed in the defect area after de-epithelialization. The reconstruction was successful and the nipple survived with a slight loss of projection. When unexpected nipple necrosis occurs after DIEP-based breast reconstruction, designing a de-epithelialized rectangular flap using the DIEP flap tissue is a feasible reconstructive method to consider.
The pedicled or free rectus abdominis myocutaneous flap and the deep inferior epigastric artery perforator (DIEP) flap are commonly used in breast reconstruction with silicone implants. However, previous studies have reported a 5% to 30% rate of necrosis in mastectomy skin and in the nipple-areolar complex following breast reconstruction [1-3]. This complication worsens the aesthetic outcome of breast reconstruction. Because of the nippleŌĆÖs protruding shape, tip or full-thickness necrosis often occurs, making it difficult to reconstruct the original shape [4,5].
In addition to necrosis, there are cases where the nipple must be removed when a subareolar resection biopsy is done to diagnose breast cancer, and reconstruction must be performed. We present a case of successful nipple reconstruction for nipple necrosis that occurred after breast reconstruction using a DIEP flap.
A 45-year-old woman was seen in our clinic for left breast cancer. She had undergone reduction mammoplasty 10 years ago, and a vertical reduction scar was observed. A nipple-sparing mastectomy was performed using the previous lower pole incision line and a subsequent DIEP flap reconstruction was performed. Considering the patientŌĆÖs history of reduction mammoplasty, part of the abdominal skin was preserved during surgery without de-epithelialization, in preparation for possible mastectomy skin-flap necrosis.
Although there were no immediately identifiable changes in the nipples, the nipple and areolar complex gradually changed color. Twelve days after the surgery, full-thickness nipple necrosis with a conversion to dry gangrene was observed. On postoperative day 15, the necrotized nipple was excised, leaving a soft tissue defect 12 mm in diameter and 15 mm deep (Fig. 1).
A 38├Ś23 mm rectangular flap was designed from the DIEP flap to cover the defect (Fig. 2). The cylindrical flap was designed with a diameter of 12 mm (12 mm├ŚŽĆŌēł38 mm), and the height of the cylinder was calculated as 23 mm, which was the sum of the mastectomy skin flap thickness (15 mm), nipple projection (2 mm), and half the length of the rectangle (12 mm/2=6 mm) used to make a nipple cap (Fig. 3).
After elevation of the full thickness of the skin and part of the subcutaneous fat, the unexcised middle inferior portion of the rectangular flap measuring 4 mm became a circulation pedicle. After rolling the elevated flap into a cylindrical shape, it was sutured with 4-0 Monosyn (B. Braun, Melsungen, Germany), and the bottom of the cylindrical flap was also approximated between the dermis of the DIEP flap using 4-0 Monosyn; hence, the flap was not depressed (Fig. 4).
After inserting the cylindrical flap into the defect site, the remnant DIEP flap tissue around the nipple-areolar complex was de-epithelialized (Fig. 5). Next, the area between the de-epithelialized site and the mastectomy skin flap and nipple cap was sutured with 4-0 Monosyn. Subsequently, the skin layer was repaired with 5-0 Ethicon (Johnson & Johnson, New Brunswick, NJ, USA) (Fig. 6). The dressing, comprising Terramycin ointment (Pfizer Inc., New York, NY, USA) and non-adhesive foam, was changed daily.
On postoperative day 19, partial skin necrosis was observed on the lateral side of the areola. However, no complications were found on the reconstructed nipple and the projection was maintained (Fig. 7). Although the nipple projection had lost 3 mm by 6 months postoperatively, the patient was satisfied with the result (Fig. 8).
Several methods have been introduced to cover postmastectomy nipple necrosis or defects [6-9]. Shestak et al. [10] compared bell flaps, modified star flaps, and skate flaps and reported that the modified flaps yielded the least projection loss. Losken et al. [9] first reported a C-V flap for nipple reconstruction and introduced several modified techniques [6,11,12].
In our case, the thickness of the patientŌĆÖs mastectomy skin flap was 15 mm; thus, there was sufficient tissue from the DIEP flap for nipple reconstruction that reproduced nipple projection. Since the techniques used thus far had resulted in projection loss, a design to minimize the loss was required. Therefore, we formed the rectangular flap into a tall nipple column to avoid depression of the nipple. Although the reconstructed nipple had depressed 3 mm at 6 months, the nipple maintained more than 80% of its initial height (final nipple height from the base: 17 mmŌĆō3 mm=14 mm; initial nipple height from the base: 17 mm; 14/17=82.35%) This degree of projection preservation was significant considering that the previous method only preserved 10.1% to 68.4% of the initial nipple height [13,14]. However, further studies are needed to determine whether these results can be consistently achieved.
Unlike the subcutaneous tissue of the C-V flap, the base of our reconstructed rectangular flap was dermis tissue, which helped avoid projection loss. In addition, the rectangular flap had sufficient vertical length for construction of the nipple cap, which makes the rectangular flap higher than the C-V flap, possibly leading to scar widening at the harvest site or a changed flap shape. However, the abdominal flap tissue, apart from the nipple itself, was placed below the mastectomy skin flap layer, maximizing nipple projection, and thereby avoiding the limitations described above. We believe that the major benefit of our cylindrical design was better flap circulation by providing wider contact of the de-epithelialized area with the mastectomy tissue. This design also resulted in a more natural shape.
Although the abdominal skin was used to reconstruct the nipple and not saved for other possible mastectomy skin-flap necrosis, the small dermal layer that would be needed (i.e., 6├Ś6├ŚŽĆŌēł113.04 mm2 of skin for a nipple cap 12 mm in diameter or 12├Ś9├ŚŽĆŌēł339.12 mm2 of skin for a 9-mm projected nipple column) could heal sufficiently by secondary intention or by a future skin graft using the remnant breast skin.
In conclusion, we suggest that a de-epithelialized rectangular flap would be a good choice for the repair of nipple loss after autologous tissue-based breast reconstruction to maintain the projection of the reconstructed nipple and achieve a better aesthetic outcome.
Notes
Patient consent
The patient provided written informed consent for the publication and the use of her images.
Fig.┬Ā1.
On postoperative day 12, full-thickness nipple necrosis occurred, and on postoperative day 15 debridement was performed in this area. After removal of the necrotic tissue, a defect 12 mm in diameter and 15 mm deep was observed.

Fig.┬Ā2.
Diagram for rectangular flap-based nipple reconstruction. In this case, the cylindrical flap was designed with a diameter of 12 mm (12 mm├ŚŽĆŌēł38 mm). The height of the cylinder was calculated as 23 mm, which was the sum of the mastectomy skin flap thickness (15 mm), nipple projection (2 mm), and half the length of the rectangle (12 mm/2=6 mm) to make a nipple cap.
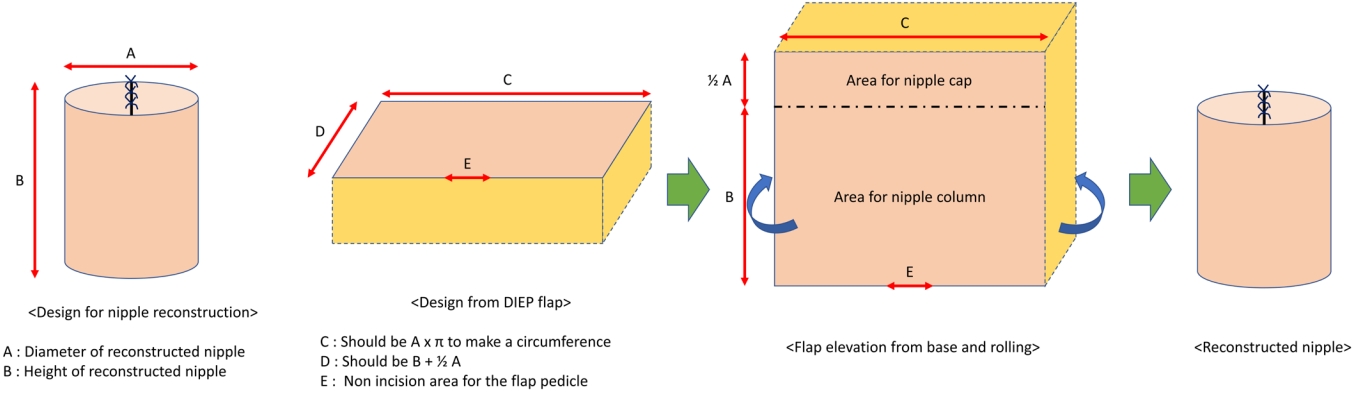
Fig.┬Ā3.
A rectangular flap was designed using a deep inferior epigastric artery perforator (DEIP) flap measuring 38├Ś25 mm. The DEIP flap was elevated including the full thickness of the skin and part of the subcutaneous fat. The middle inferior border of the flap was not incised.
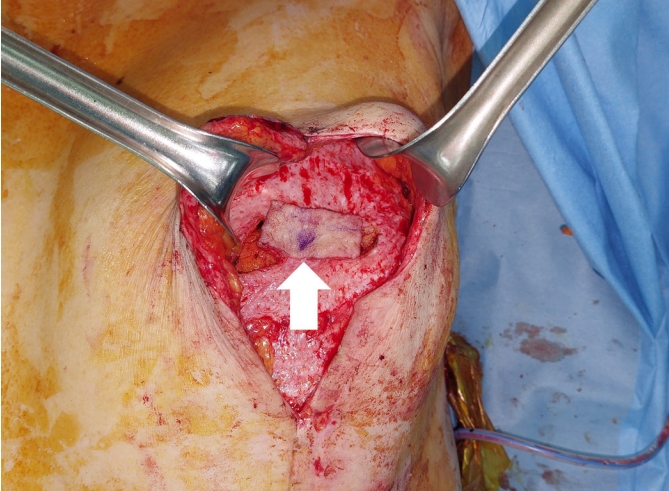
Fig.┬Ā4.
After rolling the elevated flap into a cylindrical shape, the bottom of the flap was sutured.
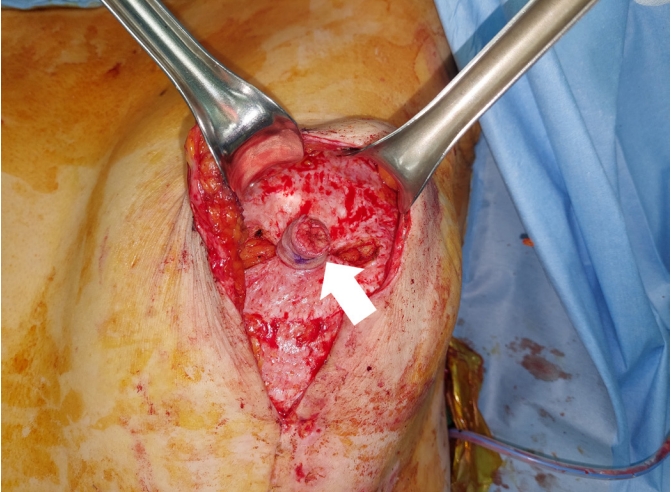
Fig.┬Ā5.
After inserting the cylindrical flap into the defect, the point where the flap and mastectomy skin flap met was marked and de-epithelization was performed on the lower segment.
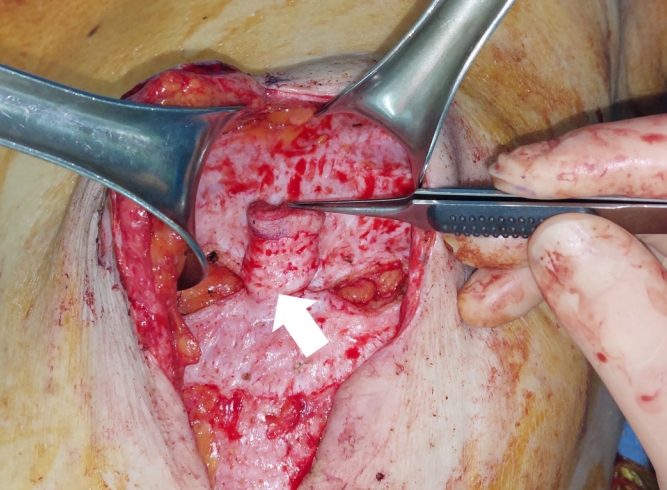
Fig.┬Ā6.
The area between the de-epithelialized site and the mastectomy skin flap was sutured with 4-0 Monosyn and 5-0 Ethicon, and the cap of the nipple was sutured in the same manner.

REFERENCES
1. Robertson SA, Jeevaratnam JA, Agrawal A, et al. Mastectomy skin flap necrosis: challenges and solutions. Breast Cancer (Dove Med Press) 2017;9:141-52.




2. Lee KT, Mun GH. Necrotic complications in nipple-sparing mastectomy followed by immediate breast reconstruction: systematic review with pooled analysis. Arch Hand Microsurg 2014;23:51-64.

3. Rao R, Saint-Cyr M, Ma AM, et al. Prediction of post-operative necrosis after mastectomy: a pilot study utilizing optical diffusion imaging spectroscopy. World J Surg Oncol 2009;7:91.




4. Cho JW, Yoon ES, You HJ, et al. Nipple-areola complex necrosis after nipple-sparing mastectomy with immediate autologous breast reconstruction. Arch Plast Surg 2015;42:601-7.



5. Gould DJ, Hunt KK, Liu J, et al. Impact of surgical techniques, biomaterials, and patient variables on rate of nipple necrosis after nipple-sparing mastectomy. Plast Reconstr Surg 2013;132:330e-338e.



6. Yoon JS, Chang JW, Ahn HC, et al. Modified C-H flap for simultaneous nipple reconstruction during autologous breast reconstruction: surgical tips for safety and cosmesis. Medicine (Baltimore) 2018;97:e12460.


7. Anton MA, Eskenazi LB, Hartrampf CR Jr. Nipple reconstruction with local flaps: star and wrap flaps. Semin Plast Surg 1991;5:67-78.

8. Guerra AB, Khoobehi K, Metzinger SE, et al. New technique for nipple areola reconstruction: arrow flap and rib cartilage graft for long-lasting nipple projection. Ann Plast Surg 2003;50:31-7.


9. Losken A, Mackay GJ, Bostwick J 3rd. Nipple reconstruction using the C-V flap technique: a long-term evaluation. Plast Reconstr Surg 2001;108:361-9.


10. Shestak KC, Gabriel A, Landecker A, et al. Assessment of long-term nipple projection: a comparison of three techniques. Plast Reconstr Surg 2002;110:780-6.


11. Eo S, Kim SS, Da Lio AL. Nipple reconstruction with C-V flap using dermofat graft. Ann Plast Surg 2007;58:137-40.


12. Mori H, Hata Y. Modified C-V flap in nipple reconstruction. J Plast Reconstr Aesthet Surg 2008;61:1109-10.











