Nipple Reduction Using an S-Shaped Excision Technique
Article information
Abstract
Many people experience psychological distress because of large nipples. In this article, the authors would like to introduce our simple nipple reduction method that addresses the drawbacks of previous methods. This technique for nipple reduction using an S-shaped excision is simple, safe, and predictable. It is also a suitable method for nipple reduction in men and in women who have completed breastfeeding.
INTRODUCTION
Men or women with large nipples may have problems with sexual relations, be afraid of taking off their clothes in public changing room, and/or feel uncomfortable when wearing tight clothing; these issues cause many people to experience emotional distress.
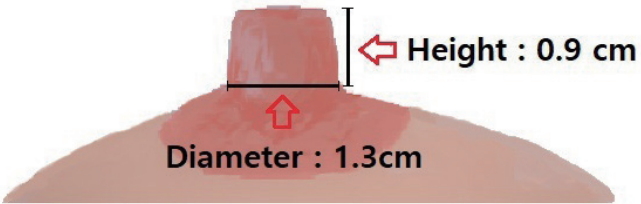
Although the ideal female nipple size has not been established, the reported average areolar diameter for Asian women is 4.0 cm, the average nipple diameter is 1.3 cm, and the average height is 0.9 cm [1]. Thus, the areolar diameter of Asian women is relatively small, but the nipple diameter is comparatively large, and for this reason, nipple reduction is more important in Asians than in other races [2]. However, many surgeons do not regard nipple reshaping to be as important as mammoplasty.
Many nipple reduction methods have been previously described, but complications such as sensory changes and delayed healing have been reported, the methods are complicated, and the outcomes are unpredictable [2-9]. In this article, the authors introduce an effective, safe, and straightforward nipple reduction method that addresses the above-mentioned drawbacks of previously described methods.
IDEA
Surgical procedure
To determine the amount of nipple tissue to remove, we agreed on an ideal nipple size and made the appropriate measurements preoperatively. Assuming that the ideal nipple size and mean size are the same, the ideal nipple shape was taken to be that of a gentle hemisphere on a cylinder with a diameter of 1.3 cm and height of 0.9 cm (Fig. 1).
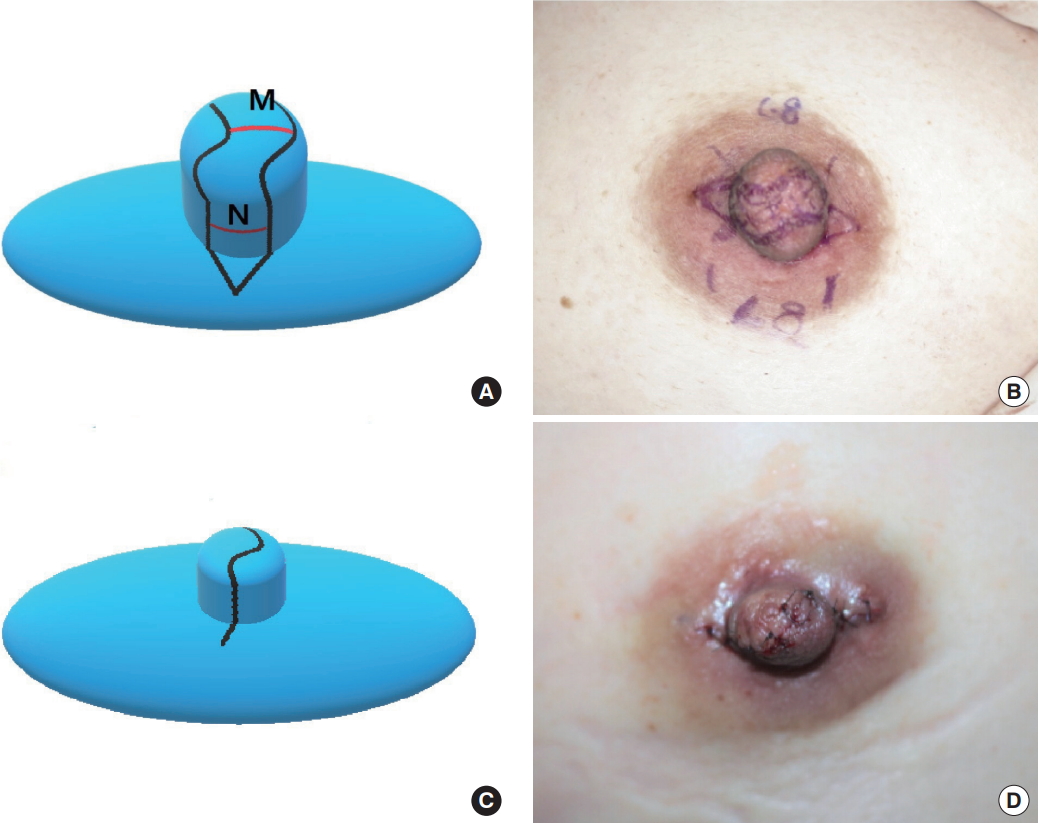
In this case, the circumference of the ideal nipple cylinder was calculated as 1.3×3.14 cm, or almost 4 cm. To create a nipple of this size, we designed two apposed flaps with an outer circumference of 2.0 cm. Briefly, given a required nipple height of 0.9 cm, 2 pairs of lines were drawn approximately 0.9 cm from the nipple-areolar junction and then 2 matching S-shaped lines were drawn across the top of the nipple from the ends of these lines (Fig. 2). The 2 dog ears at the nipple-areolar junction were corrected by excising small triangular pieces of tissue.
The variable M was defined as the width of tissue removed from the top of the nipple, and N as the width of tissue removed from the side of the nipple. When the circumference of a nipple before surgery is X, 2N=X−4.0. As shown in Fig. 2, the nipple diameter was designed to be 1.3 cm, the height to be 0.9 cm, and the circumference to be about 4.0 cm after surgery. The length of M and N may vary depending on the patient’s preference.
After M and N were determined, sufficient tissue excision was performed to minimize tension after closure. Temporary sutures were placed at the highest points on both sides of the nipple to achieve the desired height, and irregular margins were trimmed according to the height and shape desired by the patient. Suturing was then performed using 6-0 Vicryl and 6-0 nylon sutures.
DISCUSSION
Several complex techniques have been devised for nipple reduction, but if multiple flaps are elevated or excessive excision is applied to the nipple base, subsequent sensory changes may occur [3]. In addition, because nipple blood supply is provided by the subdermal plexus, complex procedures can jeopardize blood supply and cause delayed wound healing or necrosis [5,6,8,10]. From this point of view, we consider our method to be safer than previous methods, mainly because of its simplicity.
In addition, several procedures have been described that preserve lactation, but they provide ineffective nipple diameter reduction because the circumcision methods were designed to avoid the central area [4-6]. However, in previous studies the majority of patients who requested nipple reduction were either women with no intention of becoming pregnant or men, and the preservation of lactiferous ducts was therefore not an essential requirement. By using the described procedure, sufficient central parenchyma can be removed and the tension can be reduced by approximation, and the expected results satisfy patients’ long-term expectation for nipple size. Additionally, other simple methods to remove other central areas of parenchyma are effective for height removal, but they do not reduce the diameter effectively. However, our method can also effectively reduce the diameter [4,9].
An important advantage of our method is that it enables the height and circumference of the final product to be predicted, and based on our experiences, it produces results in accord with the preoperative calculations, allowing symmetrical nipples to be obtained by calculation even in the presence of asymmetry (Fig. 3). However, the primary disadvantage of our method is that short scars at the nipple-areolar junction can occur in the areolar direction, but they are adequately disguised by Montgomery tubercles. In addition, to disperse the direction of scarring, we used an S-shaped incision. No patient has yet complained about scarring because the scars became invisible at around 6 months postoperatively (Fig. 4).
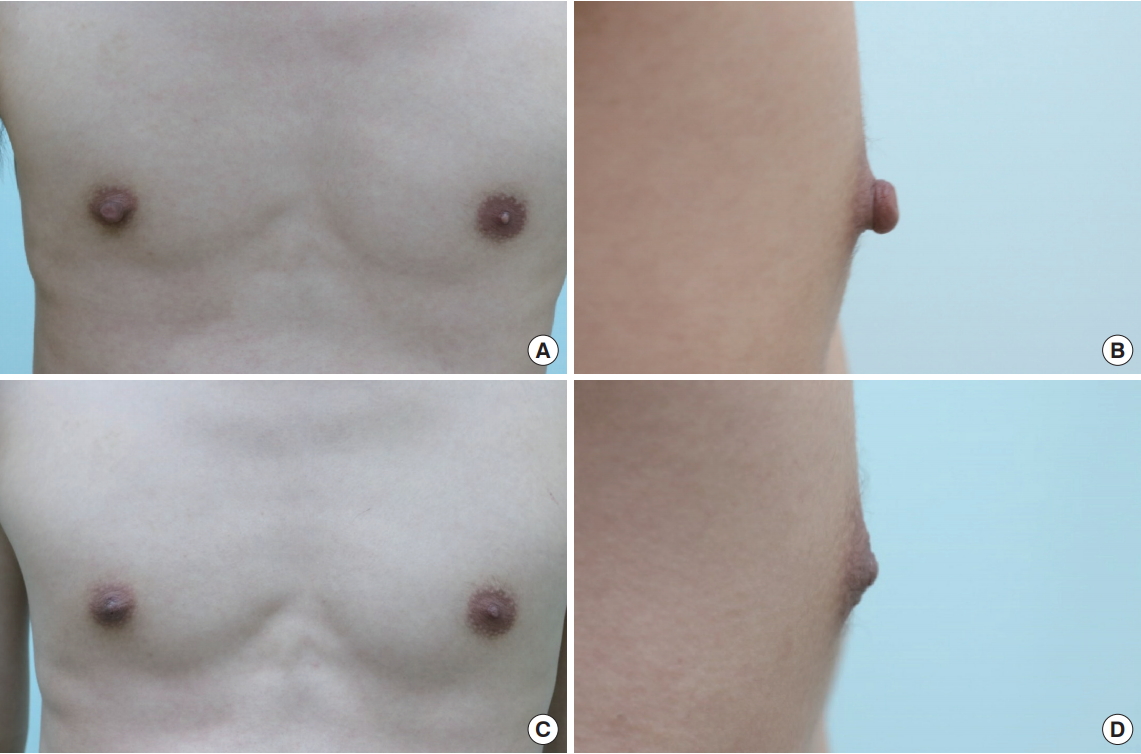
Preoperative and postoperative views of a 21-year-old man with right-side nipple hypertrophy and asymmetry. Right-side nipple reduction was performed. (A, B) Preoperative views. (C, D) Views at 6 months postoperatively showing a natural appearance.
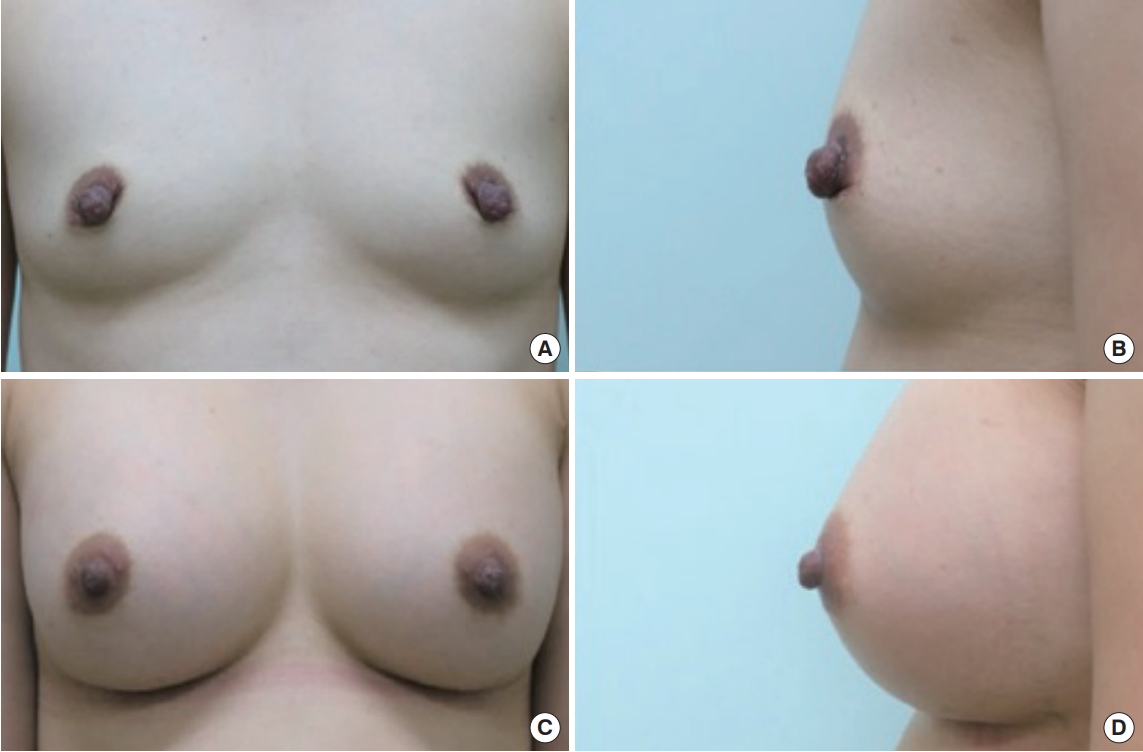
Preoperative and postoperative views of a 36-year-old woman no longer seeking pregnancy. Augmentation mammoplasty and nipple reduction were performed. (A, B) Preoperative views. (C, D) Views at 6 months.
We conclude that the described S-shaped excision technique is both safe and straightforward and produces predictable results, and that it is suitable for nipple reduction in men and in women who have completed breastfeeding.
Notes
No potential conflict of interest relevant to this article was reported.
PATIENT CONSENT
Patients provided written consent for the use of their images.