INTRODUCTION
In Asian countries, a square-shaped lower face is considered unattractive and masculine. Many women with a square-shaped lower face in South Korea and other eastern Asian countries prefer an oval and slender lower face. A square-shaped lower face is caused by a prominent mandibular angle and masseter hypertrophy; therefore, facial contouring surgery and botulinum toxin injection are performed frequently [1]. Many operative techniques of facial contouring surgery have been developed to improve the prominent mandibular angle. In 1949, Adams [2] introduced ostectomy for a prominent mandibular angle and simultaneous resection of the masseter muscle using an external approach. Converse [3] used the same surgical technique as Adams but used an intraoral approach. McCarthy et al. [4] also used an intraoral approach to resect both the mandibular angle and masseter muscle. However, these surgical techniques have limited applications for Asian patients, because these techniques usually bring the angular process toward the middle of the mandibular body, termed the second mandibular angle [1]. In 1989, Baek et al. [5] reported a multiple osteotomy procedure for a prominent mandibular angle. Many modified techniques have been subsequently reported, including ostectomy of the lateral cortex around the mandibular angle [6], angle-splitting ostectomy [7,8], sagittal split ramus ostectomy [9], and 1-stage or multistage osteotomy of the mandibular angle [1, 10]. Recently, mandibular angle ostectomy using an oscillating saw and an intraoral approach has become the primary procedure for a prominent mandibular angle.
Currently, patients with a square-shaped lower face want a narrow chin as well as improvements in the mandibular angle contour, which is called a ŌĆ£V-line shape.ŌĆØ Mandibular angle ostectomy may improve the lateral contour of the mandibular angle, but the width of the mandible is not decreased effectively [11]. Mandibular angle-splitting ostectomy may improve the frontal shape effect, [7,8] but cannot increase the mandibular plane angle or the mandibular angle [11]. To improve the frontal shape (decrease the width of the mandible to form a narrow chin) and lateral contour (mandibular angle contour) simultaneously, we modified and combined conventional surgical techniques: extended, long, curved (angle to chin) ostectomy with outer cortex grinding. We therefore conducted the present study to analyze the effectiveness of our new surgical technique.
METHODS
From May 2012 to January 2014, a total of 243 patients who elected to undergo our surgical technique for purely aesthetic reasonsa V-line shape of the lower face-were investigated. The patientsŌĆÖ ages ranged from 18 to 42 years (mean, 26.4 years). All the patients who had a prominent mandibular angle and broad chin underwent ŌĆ£extended, long, curved ostectomy with outer cortex grinding.ŌĆØ The mean follow-up period was 12.3 months (range, 4.3 to 24.3 months).
Surgical Procedure
We designed the ostectomy line preoperatively with 3D CT scans and dental panoramic X-rays. The osteotomy line was drawn along the occlusal plane of the ramus to the chin below the lateral incisor. Precautions were taken to avoid mental nerve and retromandibular vein damage with these preoperative designs.
Under general anesthesia, 0.5% lidocaine plus 1:200,000 epinephrine was injected into the inferior mandibular border, angle, and masseter muscle transcutaneously without damaging the facial artery along the mucosal incision line. An intraoral incision line was designed on the labial side of the buccal sulcus, which ran from canine to canine (anterior incision), and from the first molar to the anterior edge of the ascending ramus on each side (lateral incision). Subsequently, subperiosteal dissection was performed, the mandible was fully exposed, and the mucous membrane below the first and second premolars remained intact. The periosteum in the lower margin of the body, the posterior margin of the ramus, and the mandibular angle were raised using a U-shape periosteal elevator without damaging the integrity of the periosteum. A stylomandibular ligament on the mandibular angle was dissected completely. Osteotomy through the bone using a reciprocating saw was performed below the lateral incisor (via an anterior incision). We then carried out the osteotomy from the end of the previous osteomized line to the mandibular angle with an oscillating saw via a lateral incision. With the oscillating saw, we osteomized the outer cortex vertically then tilted the saw downward slightly to osteomize the cancellous bone and inner cortex obliquely for a natural, frontal-shape effect. We termed our surgical technique ŌĆ£extended, long, curved ostectomy,ŌĆØ because the osteotomy design was extended anteriorly below the lateral incision compared to conventional ostectomy (Fig. 1).
The grinding of the outer cortex with a small round bur was performed on the ramus and moved forward to the lateral incision and chin. A reciprocating rasp was also applied along the ostectomy line. Grinding is helpful for natural contouring on palpation and maximum frontal shape effectiveness.
The incision is closed using a double-layer absorbable 4-0 Vicryl suture for both the submucosal layer and mucosa. A drain was inserted through the incision and applied for 24 hours. Bulky compressive cotton dressing with an elastic bandage was maintained for 3 days. Elastic mask dressings were then applied.
Outcome analysis
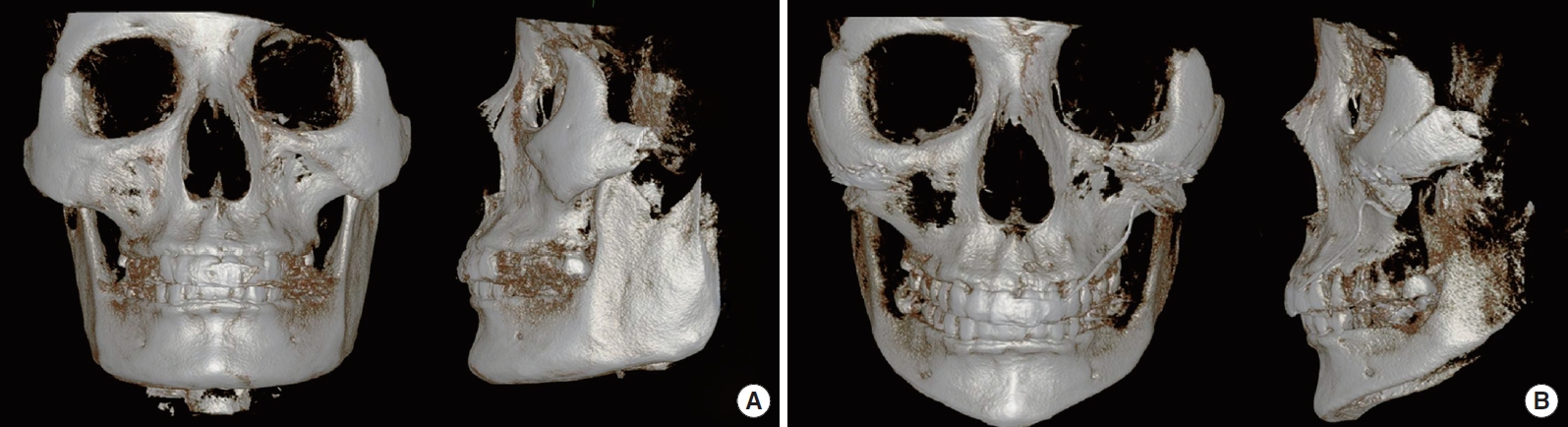
For the outcome analysis of this procedure, we used a three-dimensional (3D) computed tomography (CT) scans of each patient were done preoperatively and postoperatively (mean 10.7 months, range, 2.7 to 22.6 months) We compared mandibular angle degree and G-G (gonial-gonial) distances on preoperative 3D CT scans with the postoperative 3D CT (Fig. 2).
For statistical analyses, the paired t-test was used to compare the preoperative and postoperative data. Statistical significance was set at P<0.05. The software used for analysis was PASW Statistics 18.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
A total of 243 patients underwent the same surgical procedure-extended long curved ostectomy with outer cortex grinding-with a 12.3 month mean postoperative follow-up time (range, 4.3ŌĆō24.3 months).
Mandibular measurements demonstrated significant increments of angle degrees on the right (115.2┬░┬▒11.1 vs 129.3┬░┬▒11.5, P<0.05) and left sides (112.2┬░┬▒10.2 vs 130.4┬░┬▒11.3, P<0.05). The discrepancies of angle degrees and G-G distances both decreased postoperatively (3.1┬░┬▒1.9 vs 1.0┬░┬▒1.2, P<0.05; 123.7 mm┬▒7.9 to 110.0 mm┬▒3.5, P<0.05, respectively).
With these results, lower facial contours of all patients showed significant improvement in terms of lateral contour (increments of mandibular angle degrees on both sides and decrements of discrepancies) and frontal shape (decrement of G-G distances and chin widths) (Table 1, Fig. 3).
There were no major complications, such as temporomandibular joint malfunction or permanent mental nerve injury. Restricted mouth opening was immediately present in eight patients (3.3%) but resolved spontaneously within 3 weeks. We found evidence of hematoma (n =6, 2.7%) 4-7 days postoperatively, but evacuation procedures were not performed, since these resolved spontaneously 10-20 days postoperatively. Postoperative numbness of the lower lip and chin (n=15, 6.2%) were noted immediately, but no particular treatments were needed for these problems. The numbness resolved spontaneously within 3-6 months postoperatively with no particular treatment. A sagging face due to decreased volume and periosteal detachment of the mandible was noted in 11 patients (4.5%) but was resolved using subcutaneous liposuction 6-15 months postoperatively.
DISCUSSION
Lower face contouring surgery prevails in eastern Asian countries, [12] because a square-shaped face is regarded as an unattractive feature. There are several surgical techniques for mandibuloplasty. The conventional mandibular angle curved ostectomy often leads to a comparatively short ostectomy line and rough contour. Moreover, this procedure cannot resolve a broad chin [13].
Therefore, several newly developed surgical techniques have been developed to overcome these limitations. In 2011, Shao et al. [11] used full-thickness, long, curved ostectomy from the mandibular border of the mandible below the mental foramen to correct the lateral profile, and mandible corticectomy to improve the frontal appearance. This surgical technique is not limited to the angle but extends to the mandible body and ramus. Moreover, the lower face width (including the chin width) is reduced maximally with splitting corticectomy. However, this technique is more difficult than our technique and takes a longer time (average, 130 min compared with 60 min).
In 2014, Zhang et al. [13] reported that a single stage, en-bloc mandibular angle-body-chin curved ostectomy (MABCCO) technique via an intraoral approach coupled with outer cortex grinding (OCG) is the surgical treatment of choice for a prominent mandibular angle with a broad chin. This technique is similar to our technique, but there are several differences. A mucosal incision was made from the occlusal plane to the lateral incisor in their technique, but we designed three separate incisions: from canine to canine (anterior incision) and from first molar to the anterior edge of the ascending ramus on each side (lateral incision). We use a small, round bur on the anterior chin, which can maximize the frontal shape effect. We perform extended, long, curved ostectomy despite an intact mucosal membrane between the anterior incision and the lateral incision, because we use a reciprocating saw that can pass along the inferior mandibular margin below the intact mucosa. We can thus protect the mental nerve from transection and stretching.
In this study, we demonstrate good results with our technique, such as significant increments in degrees and symmetry of the mandibular angle, and decrements in G-G distances and chin widths. To clarify the appropriate application of our technique, long term, large-scale prospective studies and analysis of patient satisfaction are necessary for more meaningful conclusions.