INTRODUCTION
It becomes obvious that fat tissue is not just storage of excess carbohydrate. It is a regenerative complex supporting from the skin surface to deeper organs comprising adult stem cells as well as high energy resource related with tissue repair and regeneration.
Fat grafting technique, which has been performed for more than hundred years, is utilized to improve defects of facial contour, fat atrophy as an aging process and lipodystrophy due comorbid diseases. Nevertheless, the availability had been limited because of variable survival rate in accordance with operators and side effects such as fat necrosis. As Coleman technique was introduced in 1997, however, consistent operative results were obtained and autologous fat grafting has been settled as a reliable natural filler [1]. Although specific statistical report is deficient, autologous fat grafting is one of the most commonly conducted procedures in aesthetic and reconstructive surgery.
Adipose stem cell (ASC), a kind of adult stem cell, was discovered around 2000 and have been studied for more than ten years by scientists and medical doctors. The outcome of scientific research has been accumulated and led ASC to be the core element of regenerative medicine [2,3]. Furthermore, ASC has been clinically applied to fat grafting and a new method of ‘cell-assisted lipotransfer’ was introduced [4,5]. Platelet-rich plasma (PRP) can also be employed to improve survival rate of the grafted fat. PRP is known to have synergy effect with ASC in fat graft survival [6-11].
As the improvement of surgical techniques in fat surgery, survival rate of the grafted fat increased and side effects such as fat necrosis decreased. As a result, a new surgical trend of large volume fat grafting for breast and buttock augmentation showed consistent operative results, moreover, enabled augmentation mammoplasty without silicone implant [12,13]. Nowadays, fat grafting began to be applied for burn and wound management [14,15], moreover utilized to improve severe scar due to trauma and burn [16,17].
There have been several important advancements in fat grafting procedure during last ten years. Fat grafting is not a simple procedure transferring fat tissue. With the discovery of ASCs, fat grafting becomes a major tool of regenerative medicine. This article reviews recent advancements in fat grafting techniques helping plastic surgeons to understand and utilize fat transfer scientifically, furthermore intends to suggest the orientation of development in the future.
Fat harvesting, preparation and reinjection
Rohrich et al. reported that the cell viability of grafted fat is not influenced by donor site [18]. Lidocaine and epinephrine, components of tumescent solution, were proved not to give effects on fat tissues [19,20]. Harvesting fat with large cannula and gentle negative pressure helps fat survival. Shiffman et al. reported that negative pressure under 700 mmHg can cause cellular loss up to 10 percent [21]. Ozsoy et al. noted that using 4 mm cannula rather than 2-3 mm cannula increases survival rate of fat tissue [22].
The Coleman technique reported in 1997 recommends suction with 10 mL syringe to reduce damage applied to fat cell in fat harvesting, and in preparation, removes impurities and oil through 300 rpm (800 g) of proper centrifugal filtration, so raises density of the fat cell in same volume, and in reinjection, uses a thin cannula, 1 mL or 3 mL syringe, so raises possibility of revascularization from surrounding tissue with a method doing distributed arrangement of small aliquots less than 0.1 mL equally in recipient bed. The Coleman technique extended around the globe in a short time and fat grafting began to show improved engraftment rate and stable result, so settleed as a new standard of transplantation of fat [1].
Afterward, various attempts continued, and it was introduced that a method omitting centrifugation and using washing and straining technique [23] and a method putting aspirated fat on sterile towel so removing fluid and debris [24], but announcement about such new attempts were not the results by controlled comparative study so whether better results can be obtained actually with these methods is not sure. Based on several related study results in the meantime, various gears were commercialized to reduce damage of fat and progress fat harvesting and preparation, so LipVage (Genesis Biosystems, Lewisville, TX), PureGraft (Cytori Therapeutics, San Diego, CA), and Viafill (Lipose Corp, Maitland, FL) are merchandised on the market [25-27].
Ozsoy reported that in fat reinjection, adipocyte viability on use of 2.5 mm in diameter of a heavy cannula is much higher than adipocyte viability on use of 1.6 mm or 2.0 mm of cannula [22], but Erdim reported that there is no difference of cell viability according to needle gauge in fat reinjection experiment using 14, 16, and 20 gauge of needle [28].
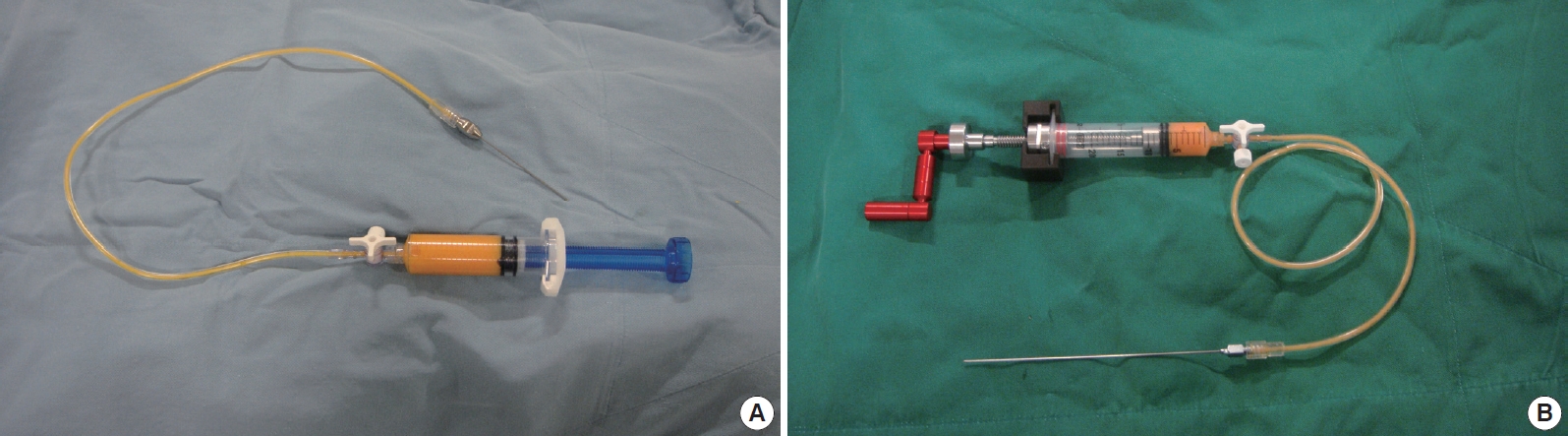
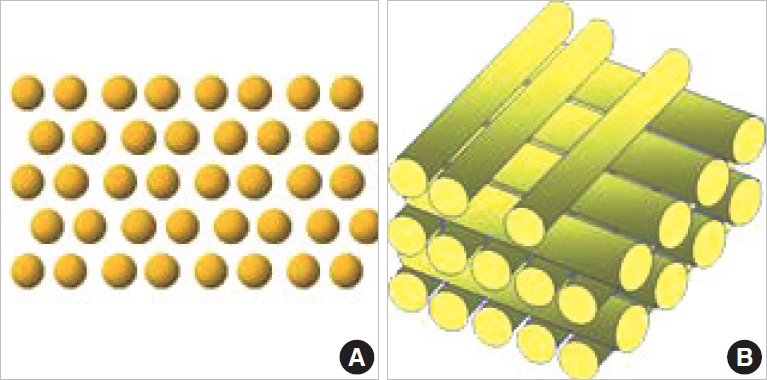
While large volume fat injection for Breast and gluteal augmentation was conducted, there is a problem that Coleman technique holding 1 mL or 3 mL syringe with a hand and injecting gradually is a time-consuming to finish hundreds mL of fat and is difficult to operate for accuracy. A solution for this problem is a screw type syringe (AP Medical, Seoul, Korea) with rotating syringe handle (Fig. 1). When an assistant holds a syringe handle and turns it one round, regular amount of o.5 mL of fat is injected. Amount of fat transplantation per the unit area is decided in inverse proportion to velocity of operator moves cannula. This is new method injecting fat as the shape like thin and long noodle in contrast with Coleman technique transplanting fat as small aliquots. In this new technique, to transplant much fat efficiently in limited recipient area, possibility of revascularization should be raised by arrangement like several logs are laid on top of another in the other direction (Fig. 2).
Adipose stem cells and fat graft update
In the middle of 1990 having 21st Century called the era of regenerative medicine ahead, plastic surgeons started to study adipose tissue dumped after body contouring surgery as liposuction in Pittsburgh University in United States. They dissociated adipose tissue with collagenase, a histolysis enzyme, and then analyzed stromal vascular fraction obtained by centrifugal filtration of cell suspension. A new type of stromal cells similar to fibroblast were identified showing multipotent differentiation potential, and these new cells are proved to be a kind of adult stem cells through various scientific experiments [2,3]. This adult stem cell extracted from adipose tissue is called with various names such as adipose tissue-derived stem cells, adipose-derived stromal cells (ADSC), adipose tissue-derived mesenchymal stromal cells, or adipose stromal cells, but recently, it is arranged as ADSC or ASC.
ASC can not only be obtained easily and plentifully from lipoaspirate but also be differentiated into various tissues such as adipocytes, cardiomyocytes, chondrocytes, endothelial cells, myocytes, neuron-like cells, and osteoblasts. So, it is acknowledged that utility of ASCs in regenerative medicine is very high.
If many cultured ASCs are used fully, remedial value of ASCs can be experienced clearly, but many mandatory controls and investment of occupancy expense are necessary to apply cultured ASC to clinics, so full-scale clinical application is not realized yet and ASC is still in the state of clinical trial for several major disease conditions in Korea. Fortunately, even with 20-30 mL of a small adipose tissue is dissociation, quite a number of cells can be obtained, and effectively used in clinics without cultured process. Especially, in ischemic condition, ASC uniformly differentiate into neoangiogenesis, which can be helpful treating postoperative wound problem, radiation necrosis, or ischemic flap of filler-induced skin necrosis [29]. A new type of fat grafting called cell-assisted lipotransfer introduced after discovery of ASC is known as a good method increasing survival rate of fat and reducing side effects in comparison with existing methods [4,5] but it is a stage of imperfection that is not easy to apply to Asian women who devoid of sufficient fat that is essential to this operation. When more than enough number of cultured ASCs are mixed with fat to be transplanted and then cell-assisted lipotransfer is will be completed as the method increasing survival rate of fat transplantation innovatively.
Another method to increase survival rate of fat grafting is the use of platelet-rich plasma (PRP). It is known that various cytokines released from platelets promote healing process and improve fat graft survival [6-11]. However, there are a report that PRP is ineffective in animal experiment [30], and there are criticism about whether the results of small animal experiment still have the reliable value in the clinical surgical procedure on real human body.
Fate of graft fat
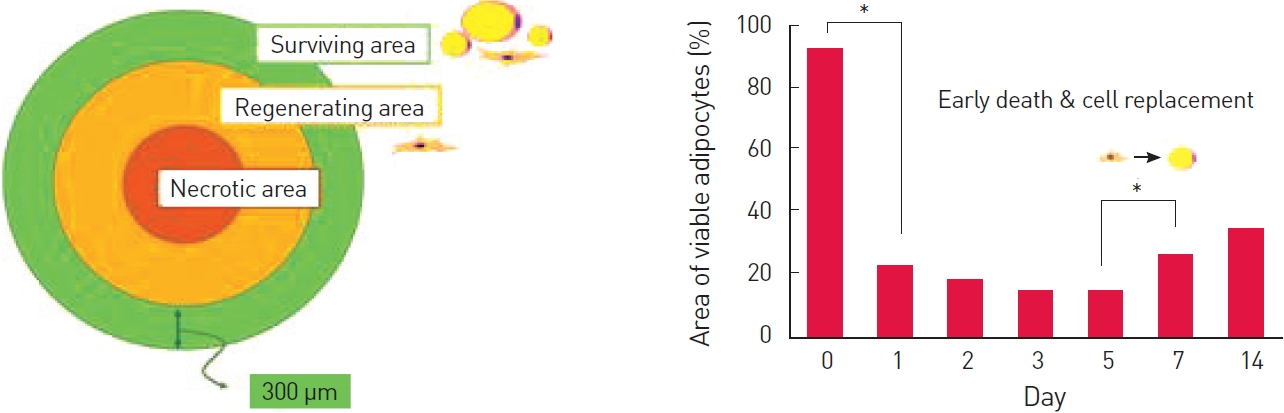
More than 100 years passed from first report of fat harvesting [31], but engraftment process of fat is uncertain yet. Long-standing hypothesis such as cell survivor theory and host replacement theory about engraftment of fat was printed in textbook until recently without clear qualification process. With increased understandings on fat biology and accumulation of clinical experience, it becomes obvious that survival of transplanted fat is influenced by various factors such as characteristic of patients, methods of fat processing, and condition of recipient bed, however logical and scientific understanding about engraftment process is still insufficient. Lately, Eto et al. published the groundbreaking result of research work about engraftment of fat and I believe it is a great advancement in fat grafting [32]. According to this result, adipocyte existing within 300 μm from the surface of transplanted adipose tissue survives, but most adipocytes located deeper in transplanted fat die within 24 hours. At this moment, some ASCs survive in the deeper part of the transplant and play an important role to regenerate adipose tissue in transplanted fat. Finally, it is important to transplant fat as a small lump so increase surface area contacting surrounding tissue on fat grafting. Henceforward, the process of fat regeneration is progressed by ASC between 3 and 7 days, so the role of ASC is important in fat grafting (Fig. 3).
Clinical application of fat grafting
According to important scientific advances such as refinement of fat grafting, discovery of adipocyte stem cells, and understanding an engraftment process of fat, interest about fat grafting cannot be higher than ever before and it is expanding the limit to new fields such as large volume fat grafting, fat transfer for burn and difficult wounds, and also for scar treatment.
Fat grafting for breast augmentation has been already attempted since several decades ago, but complications of fat necrosis, cyst formation, and infections have long been big issues. However, in these latter days, breast augmentation surgery using cell-assisted lipotransfer increases greatly [4,5], and the fat grafting procedure in patients with partial mastectomy or lumpectomy to improve breast shape is already established as a stable treatment [33-35]. Lately, many patients after breast reconstruction with flap operation or breast prostheses wants fat grafting to improve breast shape or to substitute breast prostheses for autologous fat [36]. Also, there is new method using BRAVA, external pre-expansion device, so enlarging skin pocket before fat grafting on breast to increase survival rate of fat [37,38].
Lately, it is reported that application of the fat tissue to burn wound or extensive wound not only reduces therapy period but also reduces deformity after the end of healing process [15,16]. Also, fat grafting is conducted to improve scar and scar contracture by injury or burn [17,18].
These new trials are very simple and primitive way of utilizing regenerative potential of fat and ASCs for clinical purposes at this age of government regulation. Near future, the ultimate form of stem cell therapy using cultured pure ASCs can be put into use effectively and efficiently.
Future of fat grafting and stem cell therapy
Future fat grafting may not be simple fat tissue grafting. It may be more like fat cell grafting or fat tissue engineering incorporating adipocytes, ASCs and adequate scaffold materials. Cell-assisted lipotransfer could be upgraded by enrichment with adequate number of cultured ASCs which significantly affect the engraftment of graft fat.
Full-scale clinical application of stem cell therapy is delayed by legal control to ensure patients’ safety, but the effect of stem cell therapy have been already proved through scientific verification during the past decade. Only if enough number of cultured ASC can be used in clinics as needed, era of regenerative medicine with stem cell therapy can fully open for the first time.
The business of stem cell bank have already started by ambitious investors, but it is early to create a profit yet. It may not be easy for ordinary people to spend large amount of money to preserve their own stem cells in advance for unrealized further medical techniques. However, to benefit from stem cell therapy that will be developed newly and continuously in the future, cryopreservation of own stem cells early in life will be an important medical option before long.
CONCLUSION
Scientific knowledge about fat and fat tissue transfer are accumulating rapidly. Fat is a unique regenerative complex comprising adult stem cells as well as high energy resource related with tissue repair and regeneration. The regenerative potential of fat tissue led us to expand the limit of application day by day. Fat tissue is expected to be an essential component of regenerative medicine in the twenty first century and it is essential for plastic surgeons to understand new knowledge on fat biology to perform better and reasonable clinical practice.