Initial experiences and usefulness of porcine acellular dermal matrix-assisted prepectoral breast implant surgery: a case series and systematic review
Article information
Abstract
Background
We report our experiences with prepectoral placement breast implant surgery using Supporix (HansBioMed), a porcine acellular dermal matrix (PADM), for cosmetic and reconstructive indications. The clinical efficiency, safety, and cost-effectiveness of PADM were also discussed.
Methods
A single-center, retrospective study was designed from December 2017 to December 2019. The participants were Korean women who underwent PADM-assisted prepectoral breast implant surgery performed by two surgeons. All complications were registered and analyzed. A systematic review and meta-analysis of complication rates after PADM-assisted prepectoral breast implant surgery were conducted for comparison with other studies. A subgroup analysis was performed according to the operation type: the cosmetic breast surgery (CBS) group, the immediate implant-based breast reconstruction (IIBR) group, and the delayed implant-based breast reconstruction (DIBR) group.
Results
Twenty breasts in 16 patients were included in our study (median follow-up period, 8.25 months). In a systematic review, 20 publications with a total of 2,504 breasts in 1,921 women were quantitively analyzed. The overall complication rates in our study and other studies were 14% and 24% in the total group analysis, 0% and 12% in the CBS group, 62% and 26% in the IIBR group, and 0% and 28% in the DIBR group, respectively.
Conclusions
Our data support the effectiveness of PADM-assisted prepectoral breast implant surgery, which was comparable to other studies. PADM was effective for reducing seroma and hematoma in the revision CBS group and the DIBR group. In the IIBR group, it was helpful in preventing implant loss and explantation.
INTRODUCTION
In recent years, prepectoral implant-based breast reconstruction using an acellular dermal matrix (ADM) has become increasingly common. Because of concerns regarding complications from a subpectoral approach, including animation deformity, arm-shoulder morbidity restriction, pain, chest tightness, muscle spasm, and increased recovery time, the implant site has been changed to a prepectoral site with the application of ADM. In the prepectoral approach, the proper use of ADM is important because it can reduce the risk of implant-related complications such as capsular contracture, rippling, palpability, and visibility that can occur when preChan pectoral implant placement is performed alone [1]. Currently, half of all implant-based reconstructions are performed with the use of an ADM because it improves the aesthetic outcomes by enabling better inframammary fold control, creating a larger new implant pocket in immediate breast reconstruction, and masking the surface irregularities in implant coverage [2]. However, prepectoral implant placement using ADM for full coverage of the implant requires a much larger amount of ADM than subpectoral implant placement, which uses ADM for covering the inferior pole. However, the access and use of human ADM (HADM) in prepectoral implant placement remain limited due to the more expensive cost than subpectoral implant placement. Instead of using HADM, porcine ADM (PADM) has been used in a variety of surgical fields, including breast implant surgery, after the publication of an experimental study evaluating the use of PADM for dura replacement (XenoDerm; Acelity) in 1999 [3]. One study reported strong histologic similarity and biocompatibility of PADM equivalent to that of HADM, without showing inferiority in function [4]. Although PADM is more cost-effective than HADM, data on the use of PADM are limited, and it has not been used extensively in the field of cosmetic breast implant surgery.
We present a comparative study on the safety of PADM, in which we analyzed our experiences and outcomes of PADM-assisted prepectoral breast implant surgery for reconstructive and cosmetic indications. The clinical efficiency was also discussed based on a systematic review and meta-analysis of the complication rates and safety of PADM.
METHODS
Participant selection for the case series
Institutional review board approval and informed consent were obtained for the retrospective chart review of consecutive, PADM-assisted prepectoral breast implant surgery cases performed at a single academic medical center (IRB file No. SCHUH 2019-06-006-
002). After a retrospective chart review of PADM-assisted prepectoral breast implant surgery using PADM (Supporix; HansBioMed) between December 2017 and December 2019, an analysis was performed. The candidates for our study were revisionary cosmetic breast surgery (CBS) patients with severe capsular contracture or foreign body injection, immediate implant-based breast reconstruction (IIBR), and delayed implant-based breast reconstruction (DIBR). The following clinical characteristics were recorded: age, body mass index (BMI), preoperative diagnosis, operation type, implant volume, laterality, operation time, follow-up period, and complications. Complications such as animation deformity, bottoming out, palpability, visibility, infection, seroma, flap necrosis, and capsular contracture were investigated. In addition, surgical costs according to the operation time and cost of the ADM were evaluated.
Surgical procedures and material
Before inserting the implant, we determined the implant volume and prepared the prepectoral pocket. The implant volume was determined by the volume of the excised mastectomy specimen (for reconstructive indications) or the patient’s preference and contralateral volume (for cosmetic indications). If the pocket was much wider than the implant, the lateral part including the serratus anterior muscle was sewn to narrow the width for preventing implant migration. PADM measuring 30×20 cm (Supporix, HansBioMed) and a cohesive round silicone gel-filled implant (Bellagel, SmoothFine; HansBioMed) were used for prepectoral implant placement with the ravioli technique. Supporix is a collagen tissue matrix used to support soft tissue regeneration that is derived from freeze-dried porcine skin, which was approved for use in February 2016. Before implant insertion, the PADM was emulsified for 20 minutes. After making a stab incision on the PADM, the implant was completely wrapped with half-folded PADM. The surrounding area was sewn with interrupted Vicryl 3/0 sutures. The remnant area was removed (Fig. 1). After confirming that the pectoralis major muscle (PMM) was intact, the implant was inserted above the PMM. ADM-fixation suturing was not performed (Supplementary Video 1). One silicone suction drain was inserted between the ADM cover and the skin. Double-layer wound closure was performed with Monosyn 4/0 interrupted sutures and Nylon 5/0 interrupted sutures for skin closure. The drains were left in place in all cases until the drainage was less than 20 mL in a 24-hour period. All patients received an individualized, treated postoperative dressing to prevent complications.

Total porcine acellular dermal matrix (PADM) coverage of the implant. (A) After making a stab incision on the PADM, (B) the surrounding area was sewn by interrupted Vicryl 3/0 sutures, and the remnant pieces were removed. (C) PADM was wrapped around the implant before insertion of the PADM/implant construct.
Study selection and data extraction
A systematic review of available literature was carried out in May 2020 using PubMed. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were thoroughly followed for the literature search, selection, and reporting of the available evidence. A standardized data abstraction form was developed and utilized by the authors (Fig. 2). We included references that described the use of PADM in cosmetic and reconstructive breast surgery. A literature search was performed in PubMed using the search string “porcine” AND “acellular dermal matrix” AND “breast.” The search was limited to articles in the English language and publication years from 2010 to 2020. Initially, only case reports were excluded. The titles and abstracts were screened to meet the following inclusion criteria: human studies, biologic material, prepectoral breast reconstruction, prepectoral CBS, histological data, and complications. Brief communications, correspondences, discussions, letters, and conference abstracts were excluded. The articles deemed relevant were subsequently read and examined in full to assess their eligibility. The reference lists of the included articles were also examined to identify additional relevant papers. All publications that met the inclusion criteria were deemed potentially eligible with respect to complication rates and the effectiveness of PADM in breast surgery. A search for unpublished literature was not performed. Two authors (WJS and SGK) abstracted the data independently and resolved any differences by discussion.
Data analysis
All statistical analyses were performed using Rex, an Excel-based statistical analysis software version 3.5.0.1 (RexSoft Inc.). To determine the 95% confidence intervals (CIs) of PADM complications by the meta-analysis of single proportions, the Freeman-Tukey double arcsine transformation was used for the summary statistics. The study-specific prevalence estimates were then weighted by the inverse of their variance to compute the pooled prevalence and its 95% CI. Random-effects pooled estimates were calculated. To check for between-study variance, a version of the DerSimonian-Laird method was used [5]. To compare the complication rates between our study and the other studies, we performed an exact test of the probability of success of the Bernoulli experiment. To compare the effect of PADM between our study and the other studies through the meta-analysis of complications, a target group was set up as the total group of patients who underwent breast surgery using PADM. Subgroup analysis was performed for the three groups according to operation type: the CBS group, the IIBR group, and the DIBR group. All complications requiring intervention were registered and analyzed by dividing them into eight categories (overall complications, infections, skin necrosis, seroma/hematoma, implant loss/explantation, implant exposure, capsular contracture, and minor complications) according to their frequency and probability. The minor complications included partial nipple necrosis, red breast syndrome, contour deformity, delayed wound healing, and others. Publication bias was assessed using funnel plots and Rucker’s arcsine-Thompson’s (AS-Thompson’s) test. A sensitivity analysis was also conducted to assess the influence of publication bias, as estimated by fitting a Copas selection model.
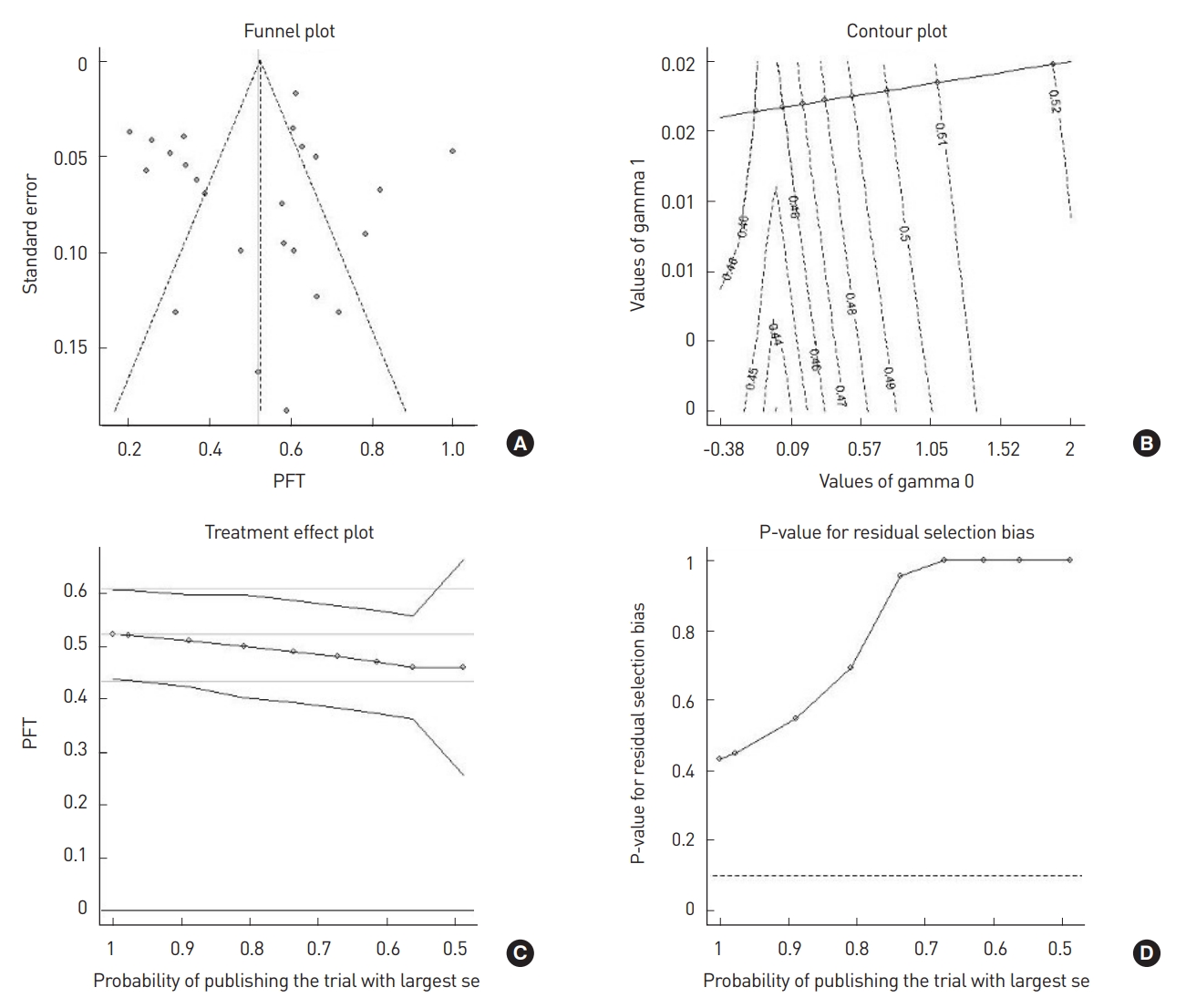
RESULTS
Efficacy of PADM for prepectoral breast implant surgery
A literature search was performed following the PRISMA guidelines. Our search yielded 78 original articles (33 articles in PubMed and 45 articles in the Web of Science). From those, a total of 26 articles were included in this paper for qualitative analysis. Studies (n=20) that clearly specified the numbers of breasts undergoing unilateral and bilateral procedures, the operation type, and complication rates were included in the meta-analysis (Fig. 3). In the systematic review, a total of 2,504 breasts in 1,921 female patients were analyzed for complication rates after PADM-assisted prepectoral implant placement. The pooled incidence of overall complications was 24% (95% CI, 17%–32%). Substantial heterogeneity (I2=93.97%; P<0.01) was detected. Therefore, a subgroup analysis by operation type was conducted. The overall complication rate was 12% in the CBS group, 28% in the DIBR group, and 26% in the IIBR group. A detailed analysis of complications showed that seroma and hematoma had the highest incidence in the CBS group (4%) and the IIBR group (10%). However, skin necrosis was the most common complication in the DIBR group (8%). The results of our systematic literature review are presented in Table 1 and Fig. 4 [6-25]. Publication bias analysis conducted with AS-Thompson’s test showed asymmetry in the funnel plot, with a statistic of 0.70 (P>0.05). This result means that significant asymmetry was found, and the results derived from this meta-analysis should be considered cautiously. Fourteen of the twenty-four studies fell outside the 95% CIs denoted by the diagonal dashed lines shown in the funnel plot (Fig. 5A), which suggests possible heterogeneity and publication bias. The logarithm of the PFT (Freeman-Tukey double arcsine transformation) from the meta-analysis may be sensitive to the range of (γ0, γ1) values. As the probability of publishing the study with the largest standard error decreased from 100% to 48%, the estimated PFT decreased from 0.43 to 0.52 (Fig. 5C). The model indicates statistically non-significant residual publication bias (i.e., P>0.10) for the diminishing probability of publication (Fig. 5D). Overall, adjusting for selection bias, the Copas selection model yielded an estimate of 0.25 (95% CI, 0.18–0.32), as did the random-effects model estimate of 0.25 (95% CI, 0.18–0.33).
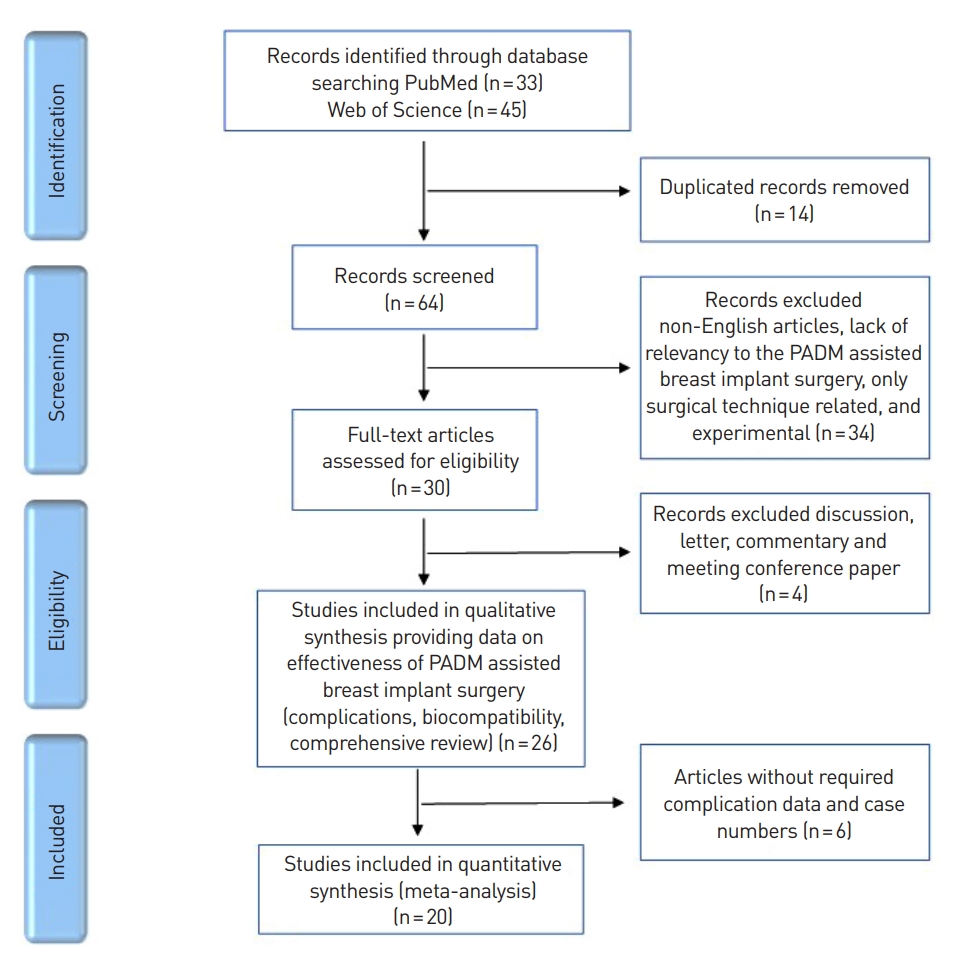
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) diagram of study selection. PADM, porcine acellular dermal matrix.
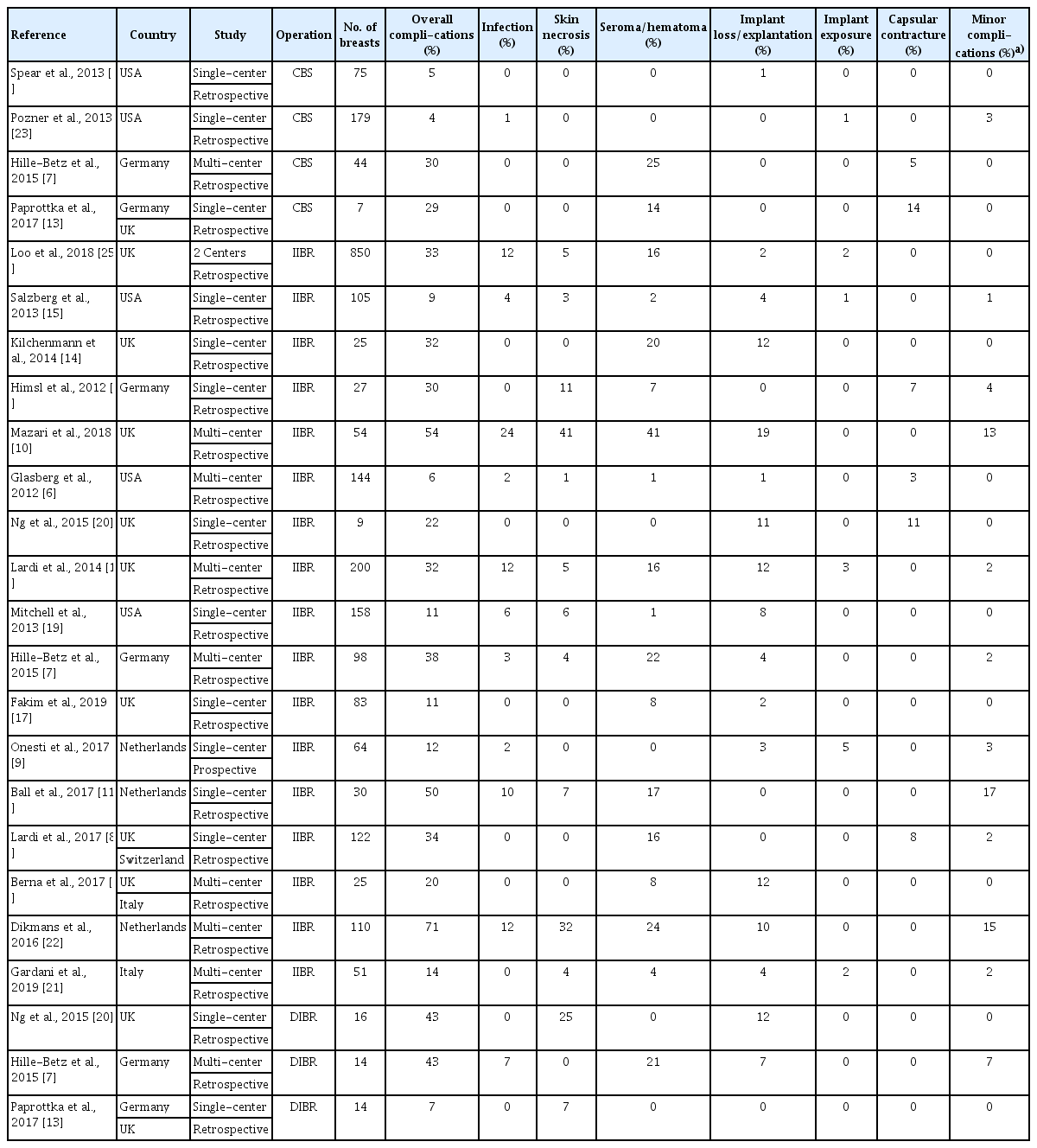
Characteristics of the studies included in the systematic review of PADM-assisted breast implant surgery with information on complication rates in a total of 2,504 breasts of 1,921 patients
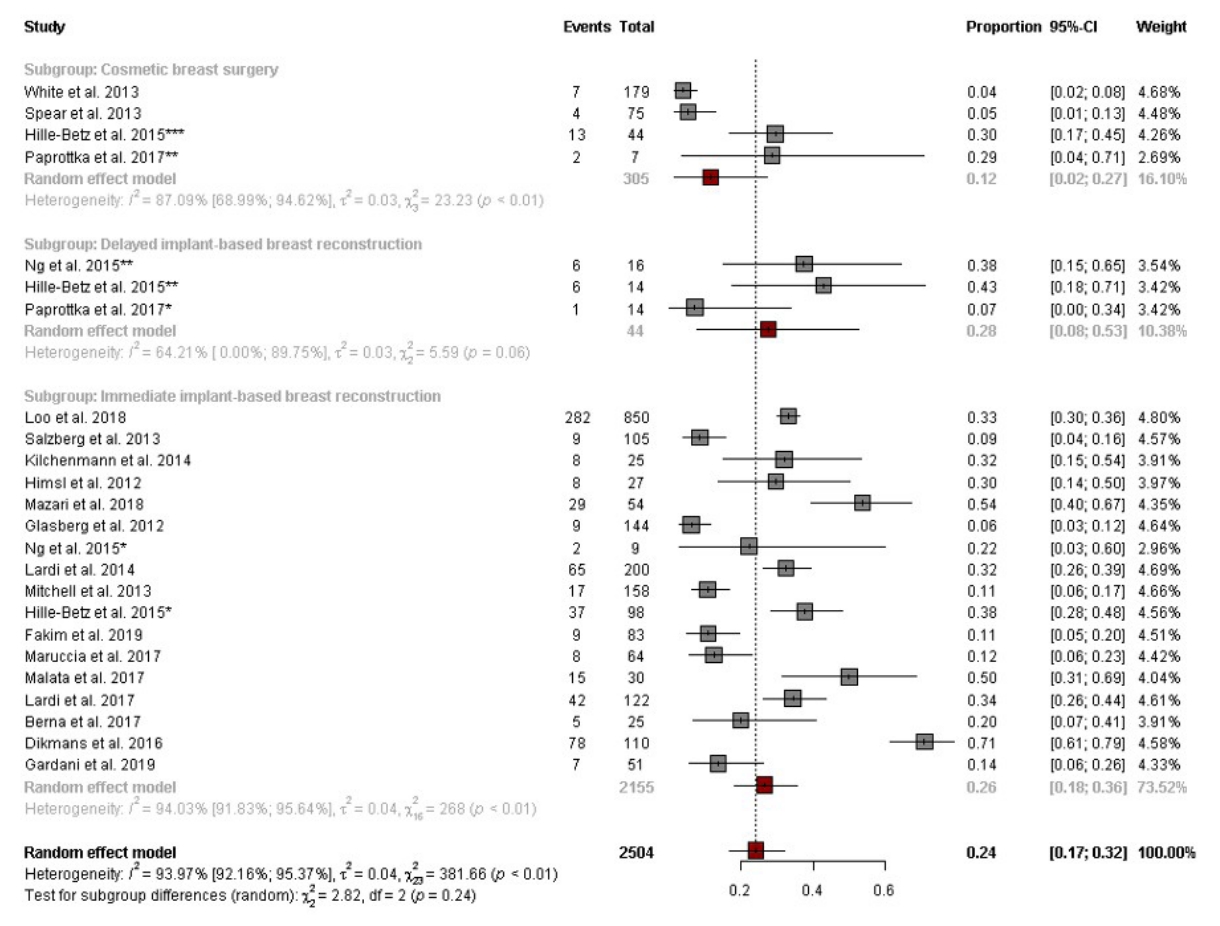
Forest plot of the incidence of overall complications after porcine acellular dermal matrix (PADM)-assisted prepectoral breast implant surgery according to operation type. CI, confidence interval. The marks *, **, and *** are used to distinguish subgroups within one journal.
Patient outcomes
PADM-assisted prepectoral implant placement was performed for a total of 20 breasts in 16 female patients (four bilateral: all cosmetic indications; 12 unilateral: 11 reconstructive, one cosmetic indication). The mean age of the patients was 50.2 years, and the mean BMI was 23.2 kg/m2. All patients asked for an intact PMM and preferred prepectoral implant placement with complete PADM coverage (the ravioli technique). For those with cosmetic indications, two had bilateral capsular contracture, two had foreign body injection, and one had implant rupture. For those with reconstructive indications, eight patients underwent immediate reconstruction followed by unilateral nipple-sparing mastectomy and three patients underwent delayed reconstruction following a lumpectomy, skin-sparing mastectomy, and contralateral augmentation mammoplasty for breast symmetry. All patients underwent direct-to-implant (DTI) breast reconstruction. In patients undergoing delayed reconstruction, skin volume and expansion were sufficiently feasible; therefore, DTI reconstruction was used rather than a tissue expander. The median follow-up period was 8.25 months (range, 3–24 months). Arm and shoulder mobility showed no restrictions. No patients complained of postoperative pain. No animation deformity was reported. The cosmetic results and the patients’ satisfaction were excellent. The implant rims were not visible or palpable. The breasts were smooth except for one case of capsular contracture (grade I). Preoperative and postoperative images of patients undergoing immediate reconstruction, delayed reconstruction, and surgery for cosmetic indications are shown in Figs. 6-8. Five complications (two cases of seroma, one case of mild infection, one case of contour deformity, and one case of partial nipple necrosis) occurred only in three patients with immediate reconstruction. No major complications such as total skin necrosis or severe infection occurred during the mean follow-up period of 8 months. A 57-year-old patient (patient No. 6) showed contour deformity of the left breast at a 1-year postoperative follow-up. The patient was suspected of having an implant rupture and seroma formation based on the computed tomography and magnetic resonance imaging findings. There was no rupture of the implant in the reoperation findings. However, the patient requested implant removal due to there were no abnormal findings, a biopsy was not performed. A 48-year-old patient (patient No. 8) showed seroma and partial nipple necrosis, which was healed by conservative treatment. A 56-year-old patient (patient No. 11) showed seroma and mild infection with fever at 1 month postoperatively. A salvage procedure was performed without implant removal. She showed a good recovery. All seromas were managed by clinic-based aspiration. All case summaries are shown in Table 2.
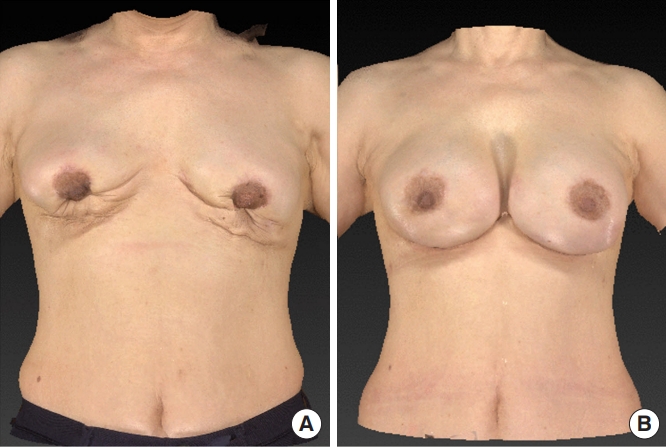
Cosmetic indication (grade IV capsular contracture). (A) Preoperative and (B) 6-month postoperative images of a patient with grade IV capsular contracture. After total capsulectomy and release of the contracture from the scoring envelope, prepectoral breast implant placement with porcine acellular dermal matrix was performed.
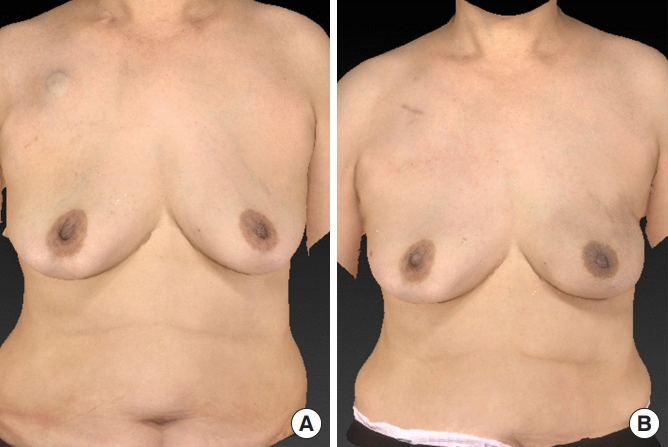
Immediate breast reconstruction. (A) Preoperative and (B) 6-month postoperative images of a patient who underwent immediate prepectoral breast reconstruction with porcine acellular dermal matrix.
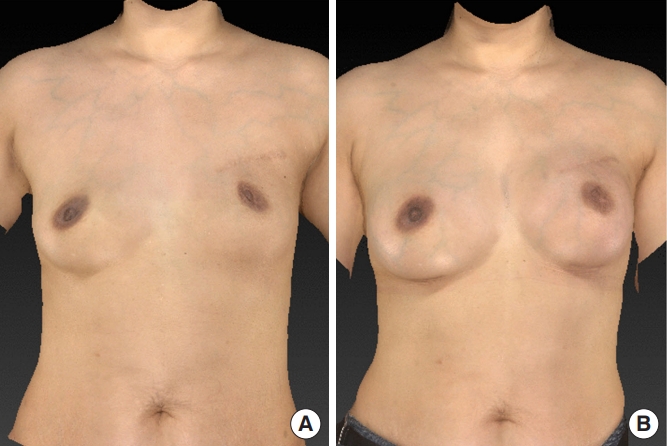
Delayed breast reconstruction. Preoperative (A) and 6-month postoperative images (B) of a patient who underwent delayed prepectoral breast reconstruction with porcine acellular dermal matrix.
Cases
Case 1 (CBS)
A 68-year-old patient (patient No. 1) with capsular contracture (grade IV) in both breasts had a history of a third revisional augmentation mammaplasty performed at another institution (Fig. 6). Although implant removal was performed during the third revision, severe lower pole scarring with capsular contracture was observed. Surgery was approached through an inframammary fold incision. The intraoperative findings showed severe scar formation throughout the pectoralis muscle and breast parenchyma. After total capsulectomy including scar tissue excision, scoring was performed in the portion where the capsular contracture was sufficiently released. The fourth revisional augmentation mammoplasty was performed by inserting a PADM/implant construct (Supporix; 250 cc Bellagel SmoothFine on both breasts) into the prepectoral space without fixation sutures. The operation time was 140 minutes. No complications occurred during the follow-up period.
Case 2 (IIBR)
A 53-year-old patient (patient No. 7) was diagnosed with breast cancer in the upper-outer quadrant of the left breast, and nipple-sparing mastectomy was performed (Fig. 7). The mastectomy specimen weighed 285 g. Immediate breast reconstruction for the left breast was planned. Surgery was approached through a 7-cm-long inframammary fold incision. Immediate breast reconstruction was performed by inserting a PADM/implant construct (Supporix; 275 cc Bellagel SmoothFine) into the prepectoral space without fixation sutures. The operation time was 85 minutes. No complications occurred during the follow-up period.
Case 3 (DIBR)
A 45-year-old patient (patient No. 14) was previously diagnosed with breast cancer in the left breast and treated by lumpectomy in 2008 (Fig. 8). The left breast was slightly flat compared to the right. Upper pole skin thinning was observed due to radiation therapy. Depressed scars were seen in the previous incision. The right breast was also small. Thus, augmentation mammaplasty for the right breast and delayed breast reconstruction for the left breast were planned. Surgery was approached through a 3.5-cm-long inframammary fold incision. Delayed breast reconstruction was performed by inserting a PADM/implant construct (Supporix; 200 cc Bellagel SmoothFine) into the prepectoral space of the left breast. Augmentation mammaplasty was also performed by inserting a PADM/implant construct (Supporix; 150 cc Bellagel SmoothFine) into the prepectoral space of the right breast. Fat injection (35 cc) was performed to correct the depressed scar on the upper pole of the left breast. The operation time was 257 minutes. No complications occurred during the follow-up period.
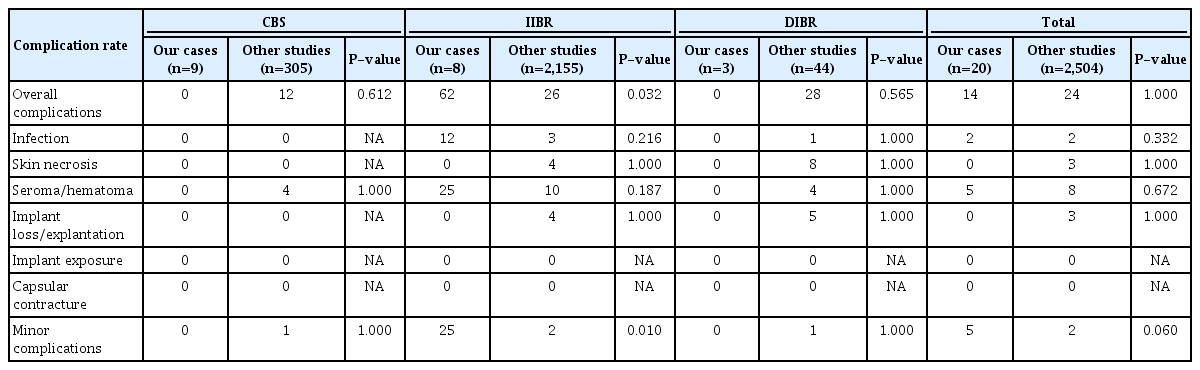
Comparative analysis between our study and other studies
In the comparative analysis, the overall rate of complications in the total group cohort was 14% in our study and 24% in the other studies, showing no significant difference. In the subgroup analysis, the overall complication rates in the CBS group and the DIBR group were lower in our study (CBS: 0% vs. 12%; DIBR: 0% vs. 28%), but significant differences were not found between our study and the other studies. Although most complications were minor and did not require hospitalization or reoperation (25% vs. 2%, P=0.01), the overall complication rate in the IIBR group was significantly higher in our study (62% vs. 26%, P=0.03). In particular, no complications were observed in the CBS group or the DIBR group in our research. In the CBS group, the incidence of infection, skin necrosis, implant loss and explantation, implant exposure, and capsular contracture was 0% in both our study and the other studies. In the IIBR group and the DIBR group, the incidence of implant exposure and capsular contracture was also 0% in both our study and the other studies. The difference in the complication rates in Tables 1 and 3 is due to the statistical difference caused by the sum of the number of study populations included in the systematic review during the subgroup analysis. All comparative analysis data are provided in Table 3.
DISCUSSION
In breast surgery, implants have been broadly used for reconstruction following nipple-sparing mastectomy or cosmetic surgery. When using an implant, the surgeon should decide the position of the implant pocket. Opinions on the optimal pocket for a breast implant remain divergent; however, prepectoral pocket placement using ADM has increasingly been implemented in recent years. This approach is simple, fast, and preserves the PMM. Thus, it does not have the disadvantages of subpectoral implant placement. Preserving the PMM was reported to play a major role not only in the simplicity of the operation but also in improving the quality of life (QoL) of patients [1]. Cattelani et al. [2] reported that the impairment of upper limb function may persist over the long term, thereby adversely influencing the QoL. They also showed that prepectoral breast reconstruction allowed patients to recover complete function of the upper limb more quickly with more improved QoL than subpectoral procedures. Our results also showed that animation deformity could affect the QoL in terms of aesthetic outcomes. In our study, no patients showed upper limb mobility restriction or animation deformity. This contributed to their satisfaction and QoL.
To reduce the risk of capsular contracture in the prepectoral approach, surgeons have used ADM to completely cover the implant. ADM can also be used to treat and prevent capsular contracture [13]. In our study, four cases of capsular contracture without recurrence were treated.
Previously, the majority of studies and evidence based on the use of ADM in breast surgery were based on HADM. However, many studies using non-human ADMs derived from bovine pericardium, bovine dermis, or porcine dermis have been recently reported because they showed similar capacities to those of HADM in various surgical fields, including dura repair, ventral hernia, chest wall reconstruction, and breast surgery [3,4,8,11,16]. Ball et al. [11] performed a direct comparison of porcine and bovine ADM (BADM) in implant-based immediate reconstruction and reported that using BADM showed significantly higher rates of skin erythema and a trend toward higher complication rates. PADM was also found to be histologically similar to HADM without being functionally inferior to HADM [4]. In a comparative study between Alloderm and Strattice, the incidence of seroma was rather high in patients who received Alloderm, which was technically supplemented by Strattice, a PADM developed later, and this finding is thought to have been due to the absence of polarity or basement membrane. Other complications were reported similarly [6]. For this reason, we used a prepectoral implant location for PADM for the first time in Korea.
The use of PADM has several advantages compared to HADM. First, PADM is more economical and easier to supply than HADM. Second, it can avoid ethical conflicts because it uses a non-human dermal matrix. Third, the incidence of complications associated with the use of PADM is not high compared to HADM. In terms of cost, Cattelani et al. [2] reported that ADM-assisted prepectoral breast reconstruction had economic superiority not only to tissue expander procedures but also to the subpectoral implant location when considering the significantly lower rate of requiring a second operation to achieve symmetry. Since the plane of breast implant placement in Korea does not make a difference in cost, even if it is covered by insurance, prepectoral implant placement using HADM for full implant coverage is extremely expensive. However, PADM is more economical. Assuming that the same size ADM is used for complete implant coverage, which is about 30×20 cm, the price of PADM (about $7,000) is almost one-third that of HADM (about $24,300). Unfortunately, only HADM is covered by health insurance in Korea and PADM is not. Nevertheless, it still has an economical advantage over HADM even after receiving health insurance benefits. This could be a new option for cosmetic reoperation patients who are paying for the procedure without insurance coverage. Furthermore, patients with reconstructive indications may benefit economically from fewer reoperations [21,24].
The results of the comparative study analyzing the effect of PADM showed that the postoperative overall complication rate in our study was 14%, which was lower than that in other studies. In our study, complications did not occur in the CBS group or the DIBR group. In contrast, the incidence of complications was relatively high in the IIBR group in our study. This difference might have been exaggerated due to the small number of cases. There were no major complications such as implant loss or explantation or implant exposure requiring hospitalization or reoperation. Compared to other studies, complications related to PADM such as implant exposure and capsular contracture did not occur in the total group. Infection, skin necrosis, and implant loss also did not occur in the CBS group. Thus, the use of PADM during breast surgery is expected to be helpful in this field. In a systematic review of the literature, high complication rates (incidence of 50% or higher) after PADM surgery were observed in three studies related to IIBR. Dikman et al. [22] performed a retrospective study on the use of Strattice in single-stage breast reconstruction and reported that the complication rate was rather high at 78% (seroma, 21%; skin necrosis, 20%). The reoperation rate was also high at 23%. The most obvious factors influencing complications were related to the patients’ choices. In particular, those who received radiation therapy and smokers were more likely to undergo reoperation. Other causes included the quality of the skin flap after mastectomy and the learning curve for the surgeon’s ADM application. Two other studies by Mazari et al. [10] and Ball et al. [11] compared Strattice and SurgiMend in IIBR. The most common complication was also seroma in one study. In that study, the cause of seroma was reported to be the high percentage of patients undergoing axillary surgery. Other complications such as implant loss, ADM loss, and reoperation could be due to the learning curve. In another study, the incidence of skin erythema and complications were significantly high, possibly due to higher mastectomy breast weight in the Strattice group.
Several limitations of our study should be noted. First, our study included a small number of cases and a short-term follow-up for complications. The proportion of complications tended to increase. This might have been because the number of cases in our study was small, and the complications were mostly concentrated in the IIBR group. Recruitment of large patient populations and long-term follow-up are needed for further analysis. Complications that require long-term follow-up, such as capsular contracture, may also increase over time, and we were unable to evaluate that possibility in the current study. Second, although a subgroup analysis was performed, there was substantial heterogeneity in the meta-analysis due to the clinical diversity in the studies included. This was the result of the limited selection of papers from which to obtain maximum information on complications and safety in breast implant surgery with PADM. The cause of such heterogeneity may also reflect the technological advances over time from 2012 to 2019 and that these studies were from several different countries, with different study designs and patient groups. Among several studies comparing HADM, PADM, and BADM, only PADM was extracted for analysis. In subgroup analysis, there were inevitably overlapping studies in the study design. For example, one study compared two or more groups of CBS, IIBR, and DIBR, and some were divided into one-stage and two-stage breast reconstruction in IIBR. The timing of reconstruction may have a somewhat different effect on PADM. This possibility requires further research. Third, radiotherapy, chemotherapy, and skin diseases that would be confused with inflammation, immune diseases, and the use of topical steroids were not included in the data analysis, so the possible effect of these factors on safety outcomes was not identified.
Our literature review and cases support the effectiveness of PADM-assisted prepectoral breast implant surgery. To the best of our knowledge, this is the first case series report of PADM-assisted prepectoral breast implant surgery in Korea. Our single-center complication rates were comparable to those of other studies. The overall complication rate was relatively low. PADM-assisted prepectoral breast implant surgery was particularly effective in revision CBS and DIBR. In IIBR, PADM was helpful in preventing implant loss, implant exposure, and capsular contracture. PADM-assisted prepectoral breast implant surgery for cosmetic and reconstructive indications had financial benefits due to its lower resource usage compared to HADM. It also provided fewer ethical conflicts and lower complication rates compared to HADM and avoided the disadvantages of subpectoral placement by detaching the PMM. However, the results of the studies included in the systematic review should be interpreted cautiously due to the influence of publication bias and substantial heterogeneity. To summarize, when consulting with patients about breast implant surgery, PADM-assisted prepectoral implant placement could be another option besides the traditional technique if it is provided with appropriate patient selection and an improved learning curve.
Notes
No potential conflict of interest relevant to this article was reported.
Ethical approval
The study was approved by the Institutional Review Board of Soonchunhyang University Hospital (IRB No. SCHUH 2019-06-006-002) and performed in accordance with the principles of the Declaration of Helsinki.
Patient consent
The patients provided written informed consent for the publication and use of their images.
Supplemental material
Supplementary materials can be found via https://doi.org/10.14730/aaps.2021.00402