|
 |
- Search
| Arch Aesthetic Plast Surg > Volume 29(2); 2023 > Article |
|
Abstract
Background
Many people with a longer second toe or lesser toes experience symptoms such as corns, hammertoe, and numerous others, especially when wearing open-toe shoes. Proximal interphalangeal joint arthrodesis using intraosseous loop wiring performed through a hidden side incision is a useful method to shorten the lesser toes aesthetically.
Methods
Aesthetic toe-shortening procedures were performed in 30 patients. All patients were evaluated by a physical examination and X-rays, and they underwent proximal interphalangeal joint arthrodesis using intraosseous loop wiring through a medial incision. Demographic characteristics, including foot morphology, were analyzed. The number of resected toes and resection amounts of each toe were measured. PatientsŌĆÖ satisfaction was determined through a questionnaire administered at each follow-up.
Results
In total, 91 toe-shortening procedures were performed in 30 patients who were followed up for an average of 24 months (range, 6ŌĆō48 months). Sixteen patients had Greek-type feet (53.3%) and 14 had square-type feet (46.7%). Twelve patients had hammer toe deformity (40.0%) and 13 had corns (43.3%). The average length of the resected second and third toes was 9.66┬▒2.79 mm (range, 5ŌĆō15 mm) and 7.78┬▒2.51 mm (range, 5ŌĆō12 mm), respectively. The vast majority of patients were satisfied with the final results. No significant complications such as nonunion occurred. Only one case of mild angulation of the second toe was noted.
The feet, especially the toes, are often exposed in daily life. Although there is wide variation in the appearance of the toes among individuals, as with all human morphological features, large discrepancies in toe size may cause discomfort when wearing footwear. If one or two toes are excessively longer than the others or deformed, it is impossible to find a pair of premanufactured shoes that fit correctly. In those situations, a person must buy a larger pair of shoes or forcibly fit his or her feet into tight shoes, leading to immense discomfort and possibly greater deformity. Other than general calluses and corns, severe lesser toe deformities include hammer toe, mallet toe, claw toe, curly toe, and crossover toe [1].
Hammer toe and mallet toe deformities are commonly encountered by foot surgeons worldwide [2]. Hammer toe is characterized by flexion abnormality of the proximal interphalangeal (PIP) joint associated with hyperextension of the metatarsophalangeal (MTP) joint and frequently occurs in conjunction with MTP joint instability [1,3]. Mallet toe is distinguished by flexion deformity at the distal interphalangeal joint and is caused by the pressure of the toe against the end of the shoe [1,3]. These abnormalities reduce mobility and negatively affect physical and psychological quality of life [4]. In cases of extensively severe hammer toe deformities, amputation of the second toe may be considered in elderly patients not in good health who do not want to undergo reconstruction [5].
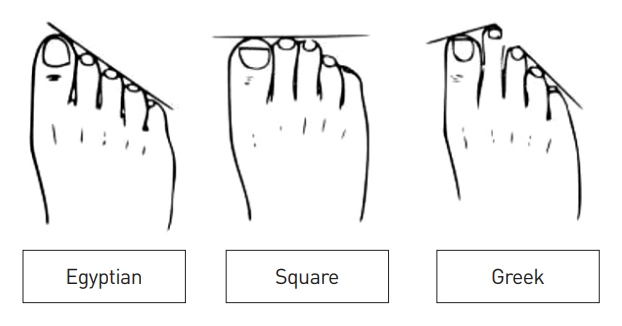
Baek et al. [6] conducted a morphological classification of feet in Korean subjects, and found that 50.3% had Egyptian-type feet, 29.4% had square-type feet, and 20.3% had Greek-type feet (Fig. 1). The Egyptian type was defined as a foot where the hallux is the longest toe, with the other lesser toes sequentially smaller to the distal side [6]. The square type was characterized as the second toe having a similar size to the hallux, and a Greek-type foot as a foot where the second toe is longer than the hallux [6]. A Greek-type foot with a long second toe may be susceptible to the development of mallet toe, hammer toe, and corns [6]. In addition, wearing high heels may lead to or worsen such deformities [6].
Common surgical techniques to address mallet toe include arthroplasty with resection of the head of the proximal phalanx and arthrodesis of the PIP joint [7]. These traditional techniques were developed to treat foot deformities, and leave prominent scars. Thus, we adopted and modified the arthrodesis method for preventive and cosmetic toe shortening. In this paper, we describe successful cases of aesthetic toe shortening. Our technique prevents future deformities without leaving prominent scars, and can thereby alleviate psychological stress and enhance the quality of life of individuals with longer second or lesser toes.
We retrospectively analyzed the medical records of patients who underwent aesthetic toe-shortening procedures from March 2009 to April 2018 at a single institution. This study was approved by Yonsei University Gangnam Severance Hospital, Institutional Review Board (#3-2018-0276).
Patients who wanted to shorten their toes for purely aesthetic purposes were included. These patients only had long toes, with no need to correct a deformity. Patients who had any other toe or foot deformity with functional disability were excluded. Individuals with diabetes or smokers were excluded because of wound healing problems.
In total, 91 toes in 30 patients were included and underwent PIP arthrodesis using intraosseous loop wiring through a medial incision that could be hidden in a normal posture. An operation on both feet was also possible on the same day. The patients underwent surgery for one toe (mostly the second) or multiple toes (second to fourth toes). The patients were evaluated through physical examinations and X-rays preoperatively and at postoperative 1 year.
We analyzed patientsŌĆÖ demographic characteristics, including foot morphology, mallet toe deformity, and the presence of corns. The number of resected toes and resection amounts of each toe were also measured. We evaluated complications, such as infection, hematoma, nonunion, and wound dehiscence. The patients also completed a satisfaction survey in which they were asked to rate their overall level of satisfaction on 5-point scale, where 1 was ŌĆ£very dissatisfied,ŌĆØ 2 was ŌĆ£dissatisfied,ŌĆØ 3 was ŌĆ£neither satisfied nor dissatisfied,ŌĆØ 4 was ŌĆ£satisfied,ŌĆØ and 5 was ŌĆ£very satisfied.ŌĆØ
Statistical analysis was performed using SPSS version 18.0 (SPSS Inc.). The categorical variables were presented as frequency and percentage, and continuous variables were as mean and standard deviation or as median and range.
All operations were performed by a single surgeon (YDL) (Fig. 2, Supplementary Video 1). First, the patient, in a supine position, was given local anesthetic near the operation site for digital block anesthesia. After sufficient preparation, a 1-inch medial longitudinal incision over the PIP joint in the neutral position was made to create an invisible scar for aesthetic reasons (Fig. 2A). The neurovascular structures at the medial and lateral aspects were carefully retracted. The extensor hood, capsule, synovium, and medial and lateral collateral ligaments at the PIP joint were released (Fig. 2B), and the PIP joint was dislocated manually (Fig. 2C). The plantar plate was not cut, and the flexor tendon was not visualized or released. The adjacent digital length was taken into consideration. After marking the resection margin on the middle and proximal phalanx (Fig. 2D), the base of the middle phalanx and the head of the proximal phalanx were resected at right angles with a sagittal saw (Fig. 2E). Excessive resection was avoided.
With appropriate shortening and alignment mimicking the natural slight angulation of the PIP joint (Fig. 2F), an electric surgical drill was used to create two transverse intraosseous channels (Fig. 2G). One channel was created 5 mm proximal to the distal stump of the proximal phalanx, and the other was formed 5 mm distal to the proximal stump of the middle phalanx. Then, an appropriately sized stainless wire (usually 20 or 22 gauge) was inserted into the channels to form a ŌĆ£boxŌĆØ loop (Fig. 2H). After confirming the formation of a box loop, the intraosseous loop of wire was gradually twisted until sufficient and firm fixation was achieved (Fig. 2I). Excess wire was cut and bent to create a soft contour. It is important to ensure adequate soft tissue coverage of the fusion site and wire loop with no irritation on the lateral toe. After the completion of fixation, the wound was closed by layers (Fig. 2J) and a soft dressing was applied.
Patients were advised to elevate the foot for 2 days after the operation and to wear a surgical shoe or shoes for 2 weeks. Patients were allowed to wear regular exercise shoes from the third week postoperatively and perform limited exercise, and they were allowed to move without restrictions after 4 weeks. At 6 weeks, the patients could resume as vigorous activity as they could tolerate.
In total, 91 toe-shortening procedures were performed in 30 patients. The ages ranged from 23 to 48 years, with a mean age of 32.9 years. Of the 30 patients, 93.3% (28 of 30) were women and 96.7% (29 of 30) had long toes bilaterally. Sixteen patients had Greek-type feet (53.3%), and 14 had square-type feet (46.7%). Regardless of the type, 12 had hammer toe deformity (40.0%) and 13 had corns (43.3%). All patients with hammer toe deformity also had corns (Table 1). The average follow-up period was 24 months (range, 6ŌĆō48 months).
Intraoperative measurements showed that the average number of resected toes was 3.03┬▒1.03 in each case. The average length of the resected second toe was 9.66┬▒2.79 mm (range, 5ŌĆō15 mm) and the average length of the resected third toe was 7.78┬▒2.51 mm (range, 5ŌĆō12 mm) (Table 2). All the operations had successful results without significant complications, such as infection, hematoma, or wound complications. Fig. 3 presents preoperative and postoperative photographs. The postoperative scar via a lateral longitudinal incision was invisible when the foot was in its natural position (Fig. 4). Radiographs revealed complete bony union in all patients. Mild angulation of the second toe was noted in one case, but it did not cause discomfort or require a secondary procedure (Fig. 5).
In the questionnaire, 96.6% of patients (29 of 30) answered that they were either ŌĆ£very satisfiedŌĆØ or ŌĆ£satisfiedŌĆØ during a follow-up examination. No patient developed problems with walking or daily activities.
Toe deformities, especially of the lesser toes, are frequently encountered conditions associated with significant morbidity [8]. It may be challenging to decide the most appropriate treatment strategy for each patient and each toe, even with an understanding of the anatomy and pathology of toe deformities [8]. Deformities of the toes often occur gradually due to ill-fitting or high-heeled footwear [8]. The main deformities are claw toe, hammer toe, and mallet toe, which result from imbalances between the forces of flexion and extension [9]. When symptoms are present, tissues such as ligaments, capsules, joint structures, and tendons may already have been irreversibly damaged, and ankle pain or deformities may result [9]. Various operative methods have been developed to address the underlying issues when symptoms are present [7].
Numerous surgical techniques have been described, and each has its advantages and disadvantages. The most traditional technique is PIP joint arthrodesis, which involves using a K-wire to transfix the fusion site; the K-wire exits the toe distally to allow future removal [2,10-12]. Typically, drilling for the K-wire is performed from the PIP joint, through the middle phalanx, and out of the distal phalanx, followed by retrograde insertion across the PIP joint to the base of the proximal phalanx. The K-wire is usually maintained for 4 to 6 weeks to stabilize the joint and reduce recurrence [13]. A K-wire is easy to insert, there is minimal need for instruments, and it maintains alignment [10-12]. However, pin tract infection is a known potential problem with any pin that exits through the skin, and immobilization delays the use of normal shoes [7,14,15]. Furthermore, removal of the K-wire may cause the patient anxiety and pain, and it is a time-consuming postoperative procedure for the surgeon [14,15].
Absorbable intramedullary pins have also been used [16,17]. Unlike K-wires, no procedure is required to remove absorbable pins, and they remain in the foot much longer than a traditional K-wire, facilitating fusion across the arthrodesis site [16,17]. Disadvantages include prolonged digital swelling and marrow edema; furthermore, they are less rigid than K-wires, making them prone to bending and breakage [10]. Absorbable pins are also more expensive than K-wires and do not provide rotational stability like K-wires [10].
Intramedullary implants are also being utilized with increasing frequency [10,18,19]. Implants have the benefits of better pain control, good union rates, decreased infection risk, and better patient satisfaction [10,18]. However, if there is an infection, the procedure required to remove the intramedullary implant is very invasive and damages the surrounding tissues, which can lead to additional bone loss or bony instability [19]. Furthermore, these implants are very expensive compared to K-wires [18].
Harris et al. [2] suggested using an intraosseous loop of stainless steel wire, and we modified HarrisŌĆÖs technique. PIP joint arthrodesis and fixation with an intraosseous box wire loop do not require hardware maintenance or removal. Despite the relative simplicity of the procedure and minimal instrumentation, box wire loop fixation is known to be resistant to displacement and to be able to maintain sufficient strength. Similar to other methods, the orientation and placement of the cut are important. Bone healing is optimized by increasing the apposition of the fusion interface. To obtain the largest surface area for fusion, the level of the metaphyseal bone should be optimized to supply sufficient blood and complete the union [20]. Furthermore, arthrodesis with accurate alignment is important. In our procedure, an additional K-wire is not required, although others have suggested that an additional K-wire can help improve the stability of PIP arthrodesis and the alignment of the corresponding MTP joint [2].
Several complications are associated with toe-shortening surgery, including angulation deformity, too-straight toes, floating toes, infection, nonunion, delayed wound healing, and wire exposure [21]. We observed only a single angulation deformity that did not require additional surgery in our case series.
The aesthetic toe-shortening procedure has several advantages. First, our procedure is performed before the irreversible changes of the second or other toes. During the dissection or subluxation, there is no need to correct irreversible damage to the soft tissues or resect a bony deformity. Therefore, the operative procedures are easier and the operative time is shortened. Second, we make an incision on the medial side of the toe. Most surgeons prefer a dorsal longitudinal incision over the midline of the digit centered over the PIP joint to create a good visible field for the correction of toe deformity [21]. Although a medial incision restricts the operative field and increases technical difficulties, it makes the postoperative scar invisible and therefore increases aesthetic satisfaction. Third, this operation could prevent toe deformities arising from abnormal anatomy or posture. Although PIP joint arthrodesis could lead to stiffness, hyperextension, or another extension deformity of the PIP joint, no patients in this study had symptomatic complications with deformities related to arthrodesis.
The limitations of this study include the small number of subjects and the short follow-up period. Furthermore, these cases were performed at a single institution. This procedure is not only suitable for treating toe deformities, but can also be used for aesthetic foot surgery. There is a debate regarding whether aesthetic toe-shortening surgery is actually needed. The American Orthopedic Foot and Ankle Society warns patients to avoid cosmetic foot surgery, emphasizing that the risks associated with foot surgery, such as infection, pain, scarring, and neurovascular damage, are much greater than the benefits. However, aesthetic toe shortening can relieve daily discomfort, prevent future deformity, and result in a cosmetically ideal foot shape, ultimately leading to better quality of life. Our excellent results indicate that our surgical method is feasible and effective.
Although the toe is a very small part of the body, its anatomical and aesthetic importance far surpasses its size. Because most shoes are fit for Egyptian-type feet, a longer lesser toe can cause substantial daily discomfort. Customized shoes are available, yet their high price and small spectrum of choice limit their accessibility. In this era of preventive medicine, the performance of a toe-shortening procedure before the development of pain and deformity could greatly improve the quality of life of many individuals. This operation can alleviate the stress caused by foot appearance with minimal risk. This technique can potentially be further modified to enhance efficiency and convenience for patients and surgeons.
Notes
Ethical approval
The study was approved by the Institutional Review Board of Yonsei University Gangnam Severance Hospital (IRB No. #3-2018-0276) and performed in accordance with the principles of the Declaration of Helsinki.
Patient consent
The patients provided written informed consent for the publication and use of their images.
Supplemental material
Supplementary materials can be found via https://doi.org/10.14730/aaps.2023.00815
Fig.┬Ā2.
Operative procedure. (A) A lateral longitudinal incision over the proximal interphalangeal (PIP) joint in the neutral position. (B) Dissection and release of soft tissue and the PIP joint. (C) Manual dislocation of the PIP joint. (D) Marking the resection margin on the middle and proximal phalanx. (E) Resection of the middle and proximal phalanx heads at right angles with a sagittal saw. (F) Appropriate shortening and alignment mimicking the natural slight angulation of the PIP joint. (G) Creation of the transverse intraosseous channel in the proximal phalanx. (H) Insertion of a stainless wire (usually 20 or 22 gauge) into the channels to form a ŌĆ£boxŌĆØ loop. (I) Twisting the intraosseous loop of wire until sufficient and firm fixation is achieved. (J) Wound closure.
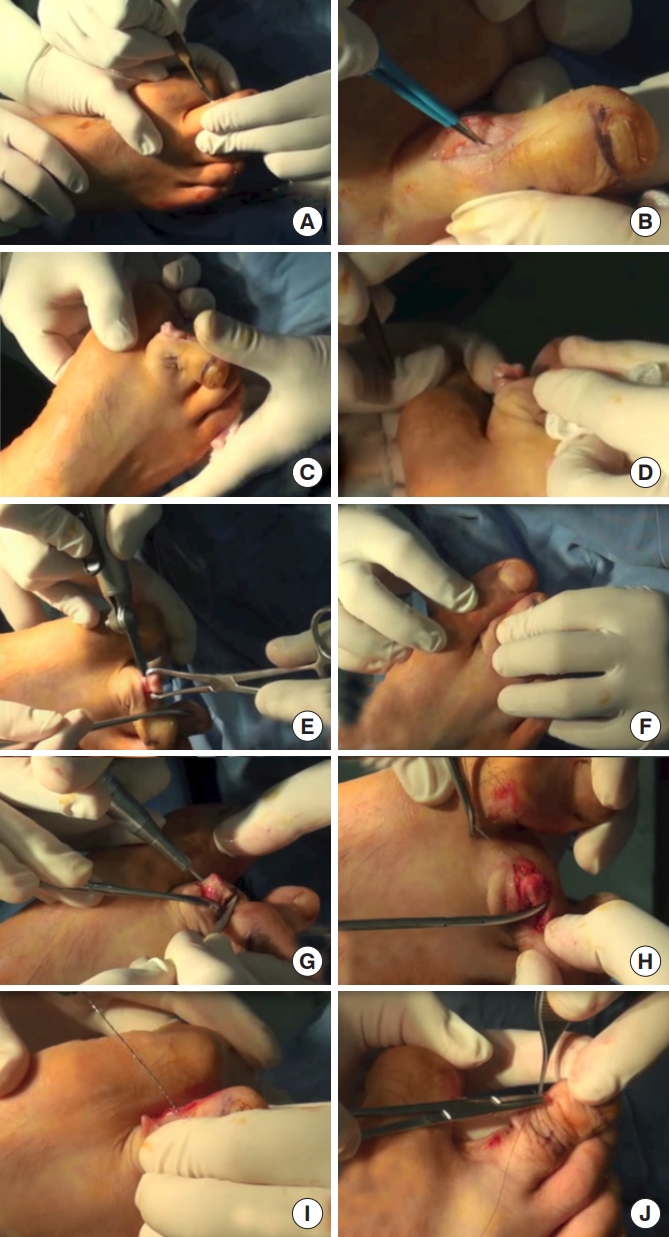
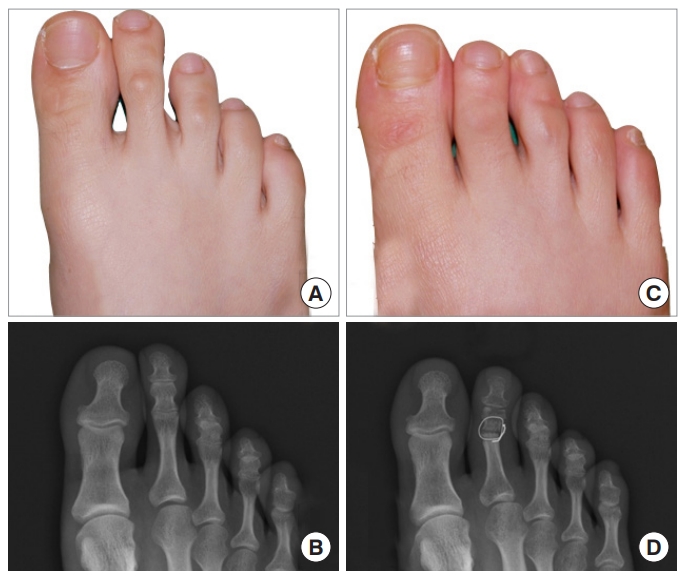
Fig.┬Ā3.
Preoperative and postoperative clinical and radiographic appearances. A 23-year-old woman had long left and right second toes. The length of the left toe was 11 mm and that of the right toe was 8 mm. Toe-shortening surgery with interosseous wiring was done. (A, B) Preoperative photographs. (C, D) One-year postoperative photographs.
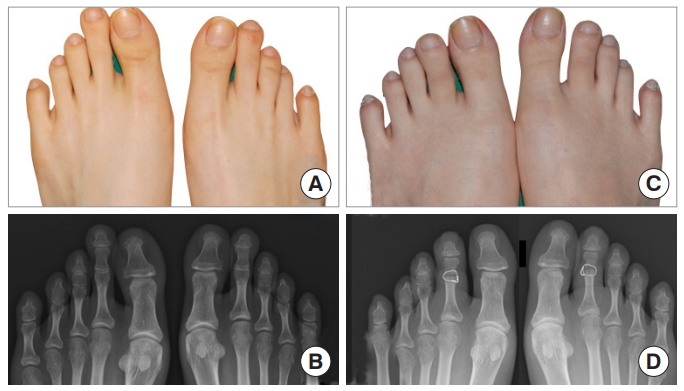
Fig.┬Ā4.
Postoperative scar after aesthetic toe-shortening surgery. Surgery was performed via a lateral longitudinal incision, and the postoperative scar was hidden when the foot was in its natural position. (A) A 23-year-old woman with long left and right second toes underwent toe-shortening surgery with interosseous wiring. The scar was not visible after 1 year postoperatively. (B) A 35-year-old woman with a long left second toe, right second toe, and right third toe underwent toe shortening surgery with interosseous wiring. The scar was not visible after 1 year postoperatively.

Fig.┬Ā5.
Complications after aesthetic toe shortening surgery. A 28year-old woman had a long right second toe. This toe was 10 mm in length (A, B). After aesthetic toe shortening surgery on the right second toe, mild angulation to the lateral side was observed (C, D). The angulation was minimal and the patient was not claimed; therefore, she did not undergo revisional surgery.
Table┬Ā1.
Demographic characteristics of patients
Table┬Ā2.
Details of the resected toes
REFERENCES
1. Shirzad K, Kiesau CD, DeOrio JK, et al. Lesser toe deformities. J Am Acad Orthop Surg 2011;19:505-14.


2. Harris W 4th, Mote GA, Malay DS. Fixation of the proximal interphalangeal arthrodesis with the use of an intraosseous loop of stainless-steel wire suture. J Foot Ankle Surg 2009;48:411-4.


4. Chen J, Devine A, Dick IM, et al. Prevalence of lower extremity pain and its association with functionality and quality of life in elderly women in Australia. J Rheumatol 2003;30:2689-93.

5. Gallentine JW, DeOrio JK. Removal of the second toe for severe hammertoe deformity in elderly patients. Foot Ankle Int 2005;26:353-8.



6. Baek SS, Park SB, Lee KM. The morphologic classification of foot in Korean. J Korean Acad Rehabil Med 1996;20:180-5.
7. Ceccarini P, Ceccarini A, Rinonapoli G, et al. Correction of hammer toe deformity of lateral toes with subtraction osteotomy of the proximal phalanx neck. J Foot Ankle Surg 2015;54:601-6.


8. OŌĆÖKane C, Kilmartin T. Review of proximal interphalangeal joint excisional arthroplasty for the correction of second hammer toe deformity in 100 cases. Foot Ankle Int 2005;26:320-5.



9. Kwon OY, Tuttle LJ, Johnson JE, et al. Muscle imbalance and reduced ankle joint motion in people with hammer toe deformity. Clin Biomech (Bristol, Avon) 2009;24:670-5.



10. Richman SH, Siqueira MB, McCullough KA, et al. Correction of hammertoe deformity with novel intramedullary PIP fusion device versus K-wire fixation. Foot Ankle Int 2017;38:174-80.



11. Hood CR, Blacklidge DK, Hoffman SM. Diverging dual intramedullary Kirschner wire technique for arthrodesis of the proximal interphalangeal joint in hammertoe correction. Foot Ankle Spec 2016;9:432-7.



12. Yassin M, Garti A, Heller E, et al. Hammertoe correction with K-wire fixation compared with percutaneous correction. Foot Ankle Spec 2017;10:421-7.



13. Coughlin MJ, Dorris J, Polk E. Operative repair of the fixed hammertoe deformity. Foot Ankle Int 2000;21:94-104.



14. Caterini R, Farsetti P, Tarantino U, et al. Arthrodesis of the toe joints with an intramedullary cannulated screw for correction of hammertoe deformity. Foot Ankle Int 2004;25:256-61.



15. Miller SJ. Hammer toe correction by arthrodesis of the proximal interphalangeal joint using a cortical bone allograft pin. J Am Podiatr Med Assoc 2002;92:563-9.



16. Konkel KF, Sover ER, Menger AG, et al. Hammer toe correction using an absorbable pin. Foot Ankle Int 2011;32:973-8.



17. Konkel KF, Menger AG, Retzlaff SA. Hammer toe correction using an absorbable intramedullary pin. Foot Ankle Int 2007;28:916-20.



18. Pietrzak WS, Lessek TP, Perns SV. A bioabsorbable fixation implant for use in proximal interphalangeal joint (hammer toe) arthrodesis: biomechanical testing in a synthetic bone substrate. J Foot Ankle Surg 2006;45:288-94.


19. Shaw AH, Alvarez G. The use of digital implants for the correction of hammer toe deformity and their potential complications and management. J Foot Surg 1992;31:63-74.

- TOOLS