|
 |
- Search
| Arch Aesthetic Plast Surg > Volume 29(3); 2023 > Article |
|
Abstract
Scars are still a challenging problem in medical practice, despite advancements in treatment modalities. Numerous treatment modalities, ranging from simple revision, Z-plasty, and W-plasty to laser treatments, have been used to treat scar deformities. However, for wide depressed scars, additional methods are needed to completely restore the contour of the depression caused by tissue adhesion. We report on the case of a 34-year-old woman with a wide depressed scar deformity on the left upper buttock and the encouraging results of an autologous fat graft injection technique that utilized a cutting wire to form a pocket for the fat graft site, while simultaneously resolving the adhesion caused by the tissue. This method is safe and easily reproducible, making it a useful addition to the surgeon’s toolkit when dealing with such lesions.
Posttraumatic scarring in various parts of the body poses a common and challenging problem for plastic surgeons. When evaluating treatment options for scar deformities, both functional and aesthetic aspects are considered in order to develop the most effective treatment plan. A wide range of surgical and non-surgical approaches have been documented for the treatment of scars. Surgical techniques such as simple excision, Z-plasty, and W-plasty have been found to effectively address the root cause of scarring, thereby increasing patient satisfaction [1]. However, postoperative scarring can become a new challenge if the initial scar is wide or long. Non-surgical options such as laser treatments are commonly employed for scar treatment, but their efficacy may be suboptimal, especially in cases of depressed scars where satisfactory outcomes may not be achieved through revision alone [2]. Although fat injection can be performed to correct the contour of a scar [3], it may not produce desirable results if performed alone due to uneven distribution and rapid fat tissue absorption [4]. It may also require release and dissection of the contracted scar tissue. This study presents a new correction method that utilizes a cutting wire and autologous fat grafting, which yielded satisfactory results in correcting a wide, depressed scar.
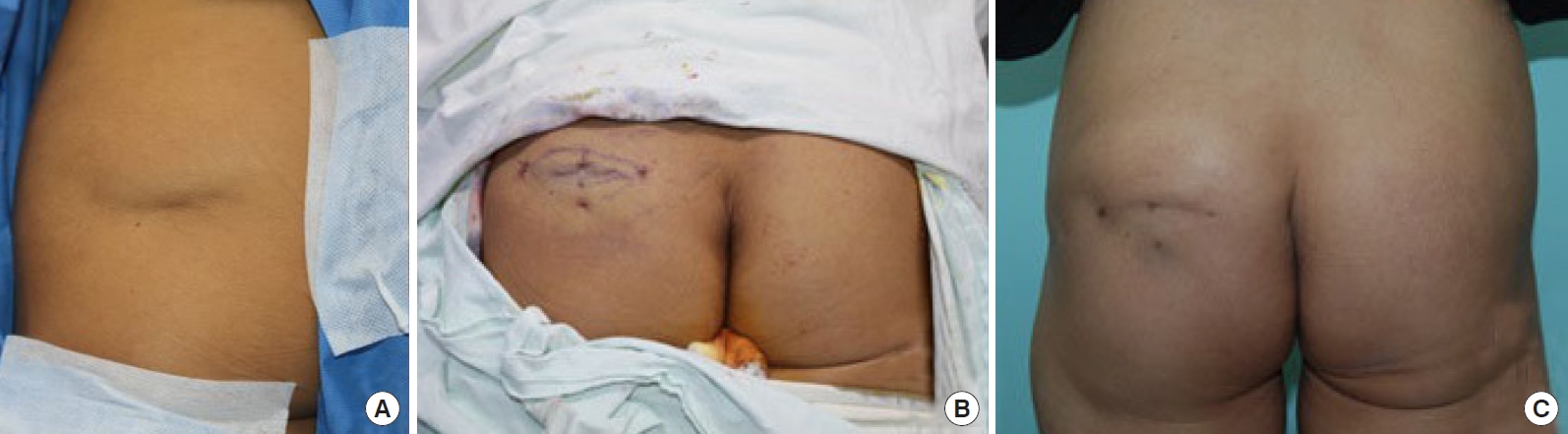
The patient, a 34-year-old female, presented with a 6 × 3-cm scar on her left hip. The scar was caused by blunt trauma when the patient slipped 7 months earlier, resulting in a closed wound. The shape of the scar was a depressed oval, which blended in color with the surrounding outer skin. Furthermore, the scar was affixed to the surface and did not move in relation to gluteus muscle motion.
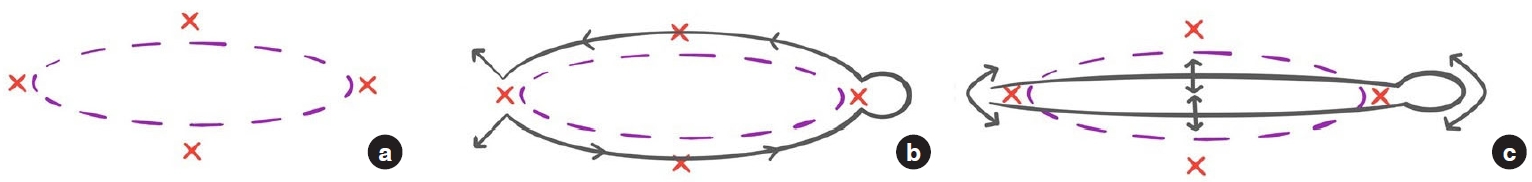
Following the traced margin of the oval-shaped scar, a surgical opening was planned in four directions at 1 cm to the left, right, upper, and lower borders of the margin (Fig. 1). Stab incisions were made to create the four opening points. Next, the prepared Ethicon No. 5 steel wire (Steel, Ethicon; J&J Surgical Technologies) was inserted through the opening on the left side of the scar and exited from the lower opening (part a in Fig. 1). The depth of the entry point in relation to the scar was set as the dermis-subcutaneous junction of the buttock below the scar tissue (approximately 5 mm to 1 cm) to avoid direct incision into the scar by running parallel to it. The wire exiting from the lower opening was then reinserted into the lower opening and brought out at the right margin of the scar border. The end of the wire that came out through the right opening was circularly curved to hold its shape for handling and then inserted through the same opening on the right. The wire was then advanced in a counterclockwise direction until the end exited through the upper opening, where it was reinserted into the upper opening once more and brought out through the first left opening. Ultimately, the entire scar tissue was circumferentially surrounded by the wire (part b in Fig. 1, Fig. 2A).
The shaped wire was then pulled back and forth in a sawing motion to release the scar from the adherent subcutaneous tissue, and elevation of the depressed scar tissue was visually confirmed (part c in Fig. 1). Active bleeding was checked throughout the procedure by applying compressive force on the opening wound. The central portion of the elevated scar was further pulled apart by tagging it with a large bite using a 4-0 nylon suture and pulling on the tagged suture, allowing the deep portion of the scar to become completely mobile (Fig. 2B and C). After the dissection, the wire was removed by pulling the two ends of the wire at the left opening while maintaining the tagging suture. As a result, a small pocket was created that lay just beneath the scar and adjacent skin.
The lower abdomen was utilized as the donor site for fat grafting and was prepared using a tumescent solution. The syringe method, using a 5 mm cannula in a standard liposuction setting, was used for the harvesting and collection of fat. The harvested fat was then placed in sterile tubes and centrifuged at 2,000 rpm for 5 minutes to separate lipid particles from the saline, tumescent, and other soft tissue particles. The saline and blood mixture was aspirated, and the remaining yellow-white mixture (containing mainly fat cells) was stored for injection.
Ultimately, 30 cc of fat was harvested from the donor site after centrifugation. The fat was then gently injected into both sides of the scar, with careful visual assessment of the contour and elevation of the scar tissue. Injection of the fat ceased once the depression was obliterated and a slight overcorrection of approximately 20% was achieved. Following repair of the depression, even distribution of the grafted fat tissue was achieved by gentle massage on the skin surface. The operation was completed by removing the tagging suture that held the central portion of the scar and closing the four stab incisions using 5-0 nylon sutures. Postoperatively, a foam dressing and pressure on the surgical site were maintained for 2 weeks. The dressing was placed to compress the circumference of the treated area, while avoiding direct pressure on the scar to prevent displacement of the fat and adhesion of the scar to the underlying fascia. Postoperative follow-up examinations were conducted shortly after surgery and again at 6 months. The contour was maintained without recurrence of depression, and the patient expressed high satisfaction with the outcome (Fig. 3).
Scarring resulting from abnormal collagen production can lead to irregular scars on the surface and result in depressions [5]. Over the years, several techniques have been introduced to correct wound depressions by resolving adhesions in the underlying deep tissue. Inchingolo et al. [6] introduced a method to correct scar depression by making a U-shaped suture after direct dissection of the adhesion with a surgical scissor. A new technique called dermal tunneling was proposed by Lima [7] to treat scar depression by loosening the fibrotic tissue in the dermal layer, but it was only reproducible in the transepidermal depth. In addition, Graivier [8] reported treatment methods using diamond wire, SurgiWire, and wire scalpel, in which the dissection was performed through an insertion made into the subcutaneous tissue below the dermal-subcutaneous junction [8]. However, these methods have limitations, particularly in patients with deep depressions that are difficult to resolve with subcutaneous tissue dissection.
In this study, the movement of the buttock scar was fixed to the motion of the gluteus muscle, which corresponded to sparing of the muscle layer [9]. However, a deep and wide scar could be inferred by the involvement of the fat tissue below. Therefore, we restored the contour of the tissue by separating the boundary between the scar tissue and the normal tissue below to secure space for the fat graft.
Although buttock scars are usually covered by clothes and may be considered less important aesthetically, we could not ignore the aesthetic outcome of the revised scar in this case because the patient worked as a model. Our surgical methods increased the patient’s satisfaction by only leaving a tiny incisional scar where the wire passed without leaving a visible linear postoperative scar. We were also able to restore the contour of the deformity by using the fat graft as tissue padding to correct the depression of the scar. Furthermore, the cutting wire used for this case was Ethicon No. 5 stainless steel wire (Ethicon, J&J Surgical Technologie), which is generally used in hernia repair and bone wiring [10]. Since surgical steel wires are stiff, resilient, and inexpensive, this procedure is easily accessible and reproducible [11].
During the procedure, we made a wide enough bite when tagging and holding the central portion of the scar with a 4-0 nylon suture to prevent thinning of the skin. We also ensured that the cutting plane was parallel to the scar by carefully controlling the wire during the incision. By taking a wide enough bite, the suture was able to hold the entire scar tissue without putting excessive tension on any one area, which helped prevent thinning of the skin. In addition, by controlling the wire and ensuring that the cutting plane was parallel to the scar, the surgeon could minimize the risk of damaging surrounding tissues and structures.
The wire was penetrated into the junction just below the scar tissue and not directly into it to minimize direct bleeding during the procedure. To prevent the possibility of unseen internal bleeding due to the small openings, periodic compressive hemostasis was also performed.
There were a few limitations in this case other than the complexity of the procedure. First, since the cutting wire was used to perform a closed blind dissection, the targeted layer could only be inferred by the resistance of the dissection plane, without direct visual confirmation. Second, the evaluation and confirmation of postoperative results relied solely on visual measurements and patient satisfaction. Finally, the fat tissue that was injected demonstrated notable longevity, which can be attributed to the non-involvement of the muscular layer. This is supported by the absence of skin dimpling during muscle contracture [9]. Using the hip region as the injection site was also advantageous, as it already possessed a high concentration of fat tissue and was less susceptible to movement-related disruption, thus aiding in the maintenance of the injected fat tissue. Other areas of the body may have different tissue characteristics and respond differently to the surgical technique. Therefore, while the technique may hold promise for scar revision in other areas of the body, additional research and clinical trials are needed to determine its potential effectiveness and safety in other areas.
Nevertheless, we report this surgical method as a simple and effective procedure that can resolve depressed contour deformities, leaving a minimal scar.
Notes
Ethical approval
The study was approved for exemption by the Institutional Review Board of Soonchunhyang University Hospital (IRB exemption No. 2022-19).
Patient consent
The patient provided written informed consent for the publication and use of her images.
Fig. 1.
Schematic diagram of cutting wire insertion into the scar tissue. (a) Schematic diagram of the scar correction shown by the boundaries of the scars (dotted line) and the incisional opening (X) around the scar for insertion of the wire. (b) Schematic diagram of wire (solid line) insertion showing the direction (arrow) and the path of the wire surrounding the boundary of the scar. (c) Schematic diagram showing the traction force (double-headed arrow) of the wire and the resulting dissection of the scar tissue above.
REFERENCES
1. Beausang E, Floyd H, Dunn KW, et al. A new quantitative scale for clinical scar assessment. Plast Reconstr Surg 1998;102:1954-61.


2. Dastagir K, Obed D, Bucher F, et al. Non-invasive and surgical modalities for scar management: a clinical algorithm. J Pers Med 2021;11:1259.



3. de Benito J, Fernandez I, Nanda V. Treatment of depressed scars with a dissecting cannula and an autologous fat graft. Aesthetic Plast Surg 1999;23:367-70.



5. Diegelmann RF, Evans MC. Wound healing: an overview of acute, fibrotic and delayed healing. Front Biosci 2004;9:283-9.


6. Inchingolo F, Tatullo M, Abenavoli FM, et al. Surgical treatment of depressed scar: a simple technique. Int J Med Sci 2011;8:377-9.



7. Lima EV. Dermal tunneling: a proposed treatment for depressed scars. An Bras Dermatol 2016;91:697-9.



8. Graivier M. Wire subcision for complete release of depressions, subdermal attachments, and scars. Aesthet Surg J 2006;26:387-94.


9. Rai S, Meng C, Wang X, et al. Gluteal muscle contracture: diagnosis and management options. SICOT J 2017;3:1.