Reconstruction of a medium-sized congenital melanocytic nevus defect using a thin thoracodorsal artery perforator free flap: a case report
Article information
Abstract
Congenital melanocytic nevus (CMN) is a benign condition that either is present at birth or develops in the first weeks of life. Surgical removal is typically performed to improve cosmetic appearance and reduce the risk of malignant transformation. In this report, we present the case of a 26-year-old woman with a medium-sized CMN on her left breast. The nevus measured 14×8 cm, and the patient desired a single-stage excision. However, this approach would result in a large skin defect that would be challenging to reconstruct using a local flap or skin graft. Moreover, it could potentially compromise the maintenance of natural sagging and the contour of the breast. Consequently, we opted to place a thin thoracodorsal artery perforator free flap following the removal of the CMN. The patient was satisfied with the overall surgical results. By utilizing this free flap for reconstruction, we successfully preserved the natural shape and contour of the breast without complications such as postoperative hypertrophic scarring or contracture at the recipient site.
INTRODUCTION
Congenital melanocytic nevus (CMN) is a benign proliferation of melanocytic cells that either is present at birth or develops within the first few weeks of life [1]. Generally, CMN classification is based on size, with a large lesion defined as one for which the greatest diameter in adulthood is 20 cm or more, a medium lesion as between 1.5 and 19.9 cm, and a small lesion as smaller than 1.5 cm [2]. The likelihood of a nevus transforming into a malignant melanoma varies depending on its size [3]. However, even if the development of malignant melanoma is unlikely, surgical removal of CMNs (except giant CMNs) is performed for two main reasons: to improve cosmetic appearance [4] and to reduce the risk of malignant transformation [3]. In this report, we describe a successful case of excision of a medium-sized CMN from the breast of a young woman and the subsequent restoration of the resulting soft tissue defect using a thin thoracodorsal artery perforator (TDAP) free flap.
CASE REPORT
A 26-year-old woman presented with a medium-sized CMN (14 × 8 cm) on her left breast that had partially invaded the nipple-areola complex (NAC) (Fig. 1A). The lesion had been present since birth and had expanded as she grew; however, no change in size was observed upon reaching adulthood, and no malignant transformation had been identified in a biopsy conducted 4 years prior. Due to aesthetic concerns, she sought surgical removal of the lesion. However, complete removal of the nevus would produce a soft tissue defect too large for primary closure. Moreover, using a local flap or skin graft to reconstruct such a soft tissue defect could make it challenging to maintain the natural shape of the woman’s breast due to postoperative hypertrophic scarring, contracture, and skin texture changes. Consequently, we opted for a free flap to close the surgical defect, as this would help preserve the natural shape, sagging, contour, and skin texture of the breast. We then decided to elevate a TDAP free flap from the right flank to cover the scarring at the donor site after surgery.

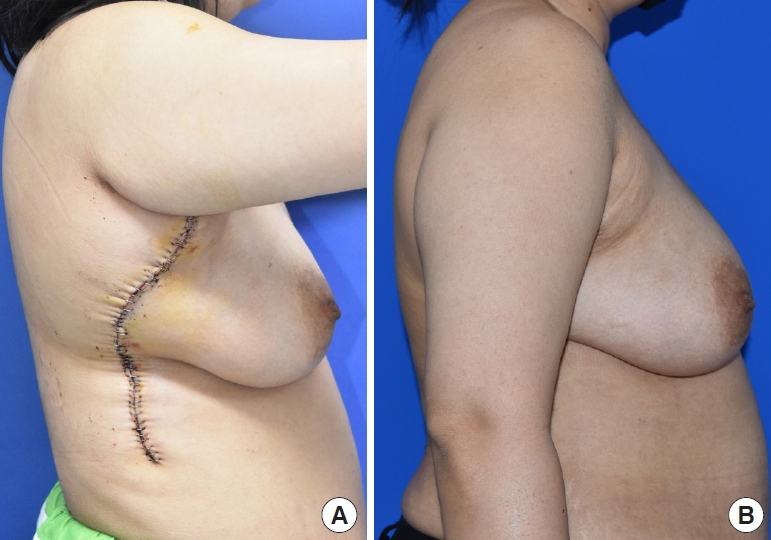
Preoperative and postoperative photographs of the surgical site. (A) Preoperative photograph. (B) One week postoperatively. (C) Three months postoperatively.
The nevus was completely excised, resulting in a soft tissue defect measuring approximately 15 × 9 cm and 7 mm thick. We selected the left internal mammary vessels as the recipient vessels. After palpation of the third rib, a small (3 cm) incision was made through the pectoralis major muscle using electrocautery. The perichondrium anterior to the cartilage was incised, and an elevator was employed to separate the perichondrium from the cartilage. A rongeur was utilized to remove the cartilage in small fragments. After cartilage removal, the perichondrium was exposed, and its dissection was carried out to identify the internal mammary vessels. Extreme caution is crucial when dissecting the internal mammary vessels using a microscope, as the vessels are very fragile.
To harvest the flap, the patient was placed in the supine position with her right arm extended and abducted at 90° to expose the flank. After confirming the location of the perforator vessel using a handheld Doppler device, we designed the flap around it. The lateral border of the latissimus dorsi (LD) muscle was marked, and a parallel incision was made 2 cm in front of the border. After identifying the LD, we split the muscle in the direction of the fibers, immediately below the skin incision. A reliable perforator piercing the LD muscle was marked with a vessel loop. We performed intramuscular perforator dissection using the deroofing technique, gradually separating the lateral border of the LD muscle from the serratus anterior muscle and the chest wall. After confirming the perforator path up to the point where it met the thoracodorsal vessels, we marked it with a surgical pen. The perforator was then elevated using bipolar electrocautery and the vessel loop, including approximately 5 to 10 mm of the muscle cuff surrounding the perforator. We dissected the thoracodorsal vessels at the bifurcation point of the transverse and descending branches and followed the branches proximally to the axillary vessels. To enable a more proximal dissection and secure a longer pedicle, we ligated the serratus anterior branch.
We then harvested a thin TDAP free flap with an approximately 10-cm-long pedicle (Fig. 2A). The thoracodorsal and internal mammary vessels were anastomosed end-to-end using 10/0 Ethilon (Ethicon) (Fig. 2B). Prior to flap insertion, the operating table was tilted at a 60° angle to assess the shape and sagging of the contralateral breast. Afterward, the flap was trimmed and inserted, and the procedure was completed.

Intraoperative photographs. (A) A thin thoracodorsal artery perforator free flap harvested from the right flank. (B) Microanastomoses between thoracodorsal vessels (yellow arrow) and internal mammary vessels (green arrow).
The patient expressed satisfaction with the overall surgical outcomes, including the similarity in skin texture between the flap and breast, the vertical donor scar, and the natural contour of the breast (Fig. 1B and C).
DISCUSSION
At present, surgical excision of CMNs is generally favored both for aesthetic purposes and to prevent their potential progression to malignancy. For smaller lesions, primary closure may be achievable; however, larger lesions necessitate reconstruction techniques, such as employing a split-thickness skin graft (STSG) [5]. While most small CMNs can be readily excised and the resulting defects easily repaired, larger lesions demand tailored approaches based on their size, location, and depth. Surgical management of large CMNs may involve serial excisions, tissue expanders, and skin grafts [6-9].
Based on the nature of the present lesion, STSG was a potential approach, since the postoperative soft tissue defect was anticipated to be too large for primary closure and the depth was expected to be shallow. However, STSG was not deemed the most favorable option because the graft donor site may have a meaningfully different skin texture and color, leading to a mismatch with the surrounding tissue, and graft contractures can cause deformities in the adjacent tissue [10]. In this case, since the surgical site was a woman’s breast, we had to take into account the anticipated postoperative cosmetic results. Serial excision was not considered, as the patient preferred a single-stage excision and because a serial excision could alter the shape of the breast. Additionally, we concluded that an STSG could result in a wide donor-site scar on the anterior thigh, which the young woman would not consider aesthetically pleasing.
We determined that a flap from the right flank would be advantageous, as the donor-site scar could be concealed when the arm was naturally lowered (Fig. 3). Selecting an inguinal area as the flap donor site, rather than the flank, may have been more appropriate for cosmetic reasons in terms of hiding scarring. After excision of the nevus, a pedicle length of approximately 6 to 7 cm was needed to anastomose to the internal mammary vessel through the glandular tissue and the pectoralis major with intact glandular tissue. However, the average pedicle length of a superficial circumflex iliac artery perforator (SCIP) flap is known to be 5 cm [11]. Since we were uncertain whether such a pedicle length would be sufficient to achieve anastomosis through the SCIP flap, we did not consider it. Additionally, the average diameter of the SCIP flap pedicle is approximately 0.7 cm [11], while the diameter of the internal mammary artery ranges from 1.9 to 2.6 mm in adults [12]. The expected difference in diameter between the superficial circumflex iliac artery and the internal mammary artery was large, and we anticipated that vascular anastomosis would be challenging. Since the present patient was obese, a deep inferior epigastric artery perforator (DIEP) flap was also considered. However, a DIEP flap is too thick to be suitable for a shallow defect, such as the one in our case. Furthermore, the patient did not want a scar on her abdomen and therefore declined the DIEP flap option.
Postoperative donor site scar. (A) Scar at the flap donor site on the right flank. (B) Donor site scar concealed by the arm at 3 months postoperatively.
In the present case, we utilized a thin TDAP free flap. Depending on whether the perforator of a flap harvested from the lateral chest wall is musculocutaneous or septocutaneous, it may be denoted as an LD perforator (for the former) or a TDAP (for the latter) [13]. In this case, we used a musculocutaneous perforator piercing the LD muscle, making it appropriate to present it as an LD perforator. However, the two terms (LD perforator and TDAP) are commonly described interchangeably as TDAPs, so we used the term “TDAP” in this report. For optimal flap positioning and anastomosis of the internal mammary vessels, long flap pedicles are required. The average pedicle length of the TDAP free flap is 20 cm (range, 16–23 cm) [14]. Another reason for choosing the TDAP free flap is that a “super-thin” flap can be achieved by excluding the deep adipose layer during harvesting. The flap can be further thinned to < 5 mm as long as sufficient fatty tissue remains around the perforators [15]. Additionally, since both the breast and flank are anatomically located in the thorax, they share similar skin textures. For these reasons, we used a thin TDAP free flap to reconstruct the soft tissue defect occurring after a medium-sized CMN excision.
A limitation of this case was the inability to perform NAC tattooing due to the patient’s refusal, which led to suboptimal NAC reconstruction and a widened scar at the donor site on the right flank. Furthermore, the flap width was somewhat inadequate, resulting in a flattened appearance of the breast’s lower pole and a visible inframammary fold post-surgery. We anticipate that future revisions, such as fat grafting, may be necessary to address this volume deficiency.
Among the various free-flap donor sites utilized for breast reconstruction, a thin TDAP free flap appears to be the ideal choice for covering shallow defects, such as those resulting from medium-sized CMN resections, as demonstrated in the present case. This approach offers optimal results with regard to postoperative scarring and cosmetic outcomes.
Notes
No potential conflict of interest relevant to this article was reported.
Ethical approval
The study received approval from the Institutional Review Board of Chungnam National University Hospital (IRB No. 2023-04-094).
Patient consent
The patient provided written informed consent for the publication and use of the images.
