 |
 |
- Search
| Arch Aesthetic Plast Surg > Volume 20(2); 2014 > Article |
Abstract
Background
Ablative fractional carbon dioxide laser is widely used for the treatment of various scars including burn injuries. We applied ablative fractional CO2 laser on the skin graft scar of faces.
Methods
Fourteen patients between 2010 and 2013 who underwent facial skin graft were included in this study. The ablative fractional CO2 laser was applied to 7 patients in the laser therapy group. It was initiated at 5th week after the skin graft. Clinical photographs were taken, and Patient Scar Assessment Score (PAS) was obtained during every visit from a patient at the outpatient clinic and 4 weeks after the last laser treatment. In the untreated control group, clinical photographs and PAS were taken at 5th and 21st weeks after the skin graft. Vancouver Scar Scale (VSS) and Observer Scar Assessment score (OAS) was rated by single independent plastic surgeon with the clinical photographs.
Autologous skin graft is considered as one of the most useful method to cover partial or full thickness of skin defects [1]. However, after the skin graft, operative site has characteristics of poor skin elasticity, hypertrophy or atrophy and depression. These can cause poor functional or aesthetic outcomes and are the major short-comings of this procedure [2].
To improve the scarring after the graft, resurfacing methods such as the conventional dermabrasion, ablative carbon dioxide lasers and chemical peels can be performed. However, these methods have a limitation because there are risks of hypo-, hyperpigmentation or prolonged downtime. A higher incidence of scarring due to the delivery of laser radiation or excessive mechanical stimulation also makes surgeon to avoid the ordinary use of ablative carbon dioxide laser or conventional dermabrasions in skin graft scar treatment [1,3,4]. Also, conventional ablative laser treatment needs relatively a long time for re-epithelialization and patient can be suffered from discharge, pain and severe erythema during the healing process [5,6].
On the other hand, ablative fractional laser that is widely used in scar management, makes it possible to overcome the discomfort and complications of conventional ablative laser by reducing the downtime and epithelization time after the laser therapy [5]. The concept of fractional photothermolysis has been introduced in 2004 [6], and numerous articles revealed the effectiveness of fractional lasers in various scars such as acne and burn scars. Because of its excellent effect on collagen remodeling [7,8] and fewer side effect compared to conventional ablative laser, fractional photothermolytic devices became the one of the most useful methods to management of scar in the present [9-12].
Although fractional laser has been applied on various types of scars originated from trauma, burn or clean surgery such as a thyroidectomy, no tries have been made to use the fractional laser on the skin graft scar to our knowledge. In this study, we applied the fractional laser device to the skin graft scar and evaluate the results.
We designed prospective study to compare the result between fractional laser treatment group and untreated group. From 2010 and 2013, seven patients received ablative fractional carbon dioxide laser treatment in early period of scar maturation after skin graft in Wonju Severance Christian Hospital. Seven patients who did not receive the any scar management even silicone sheet or gel were included as a control group. Skin graft location, cause of defect, skin graft type and skin graft size were presented (Table 1).
The laser treatment was prepared with skin cleanser. Occlusive application of topical anesthetic cream containing 2.5% lidocaine and 2.5% prilocaine (EMLA; AstraZeneca LP, Wilmington, DE) was maintained for 30 minutes prior to the treatment. The entire grafted site and the surrounding normal-appearing skin was treated with a 10,600 nm fractional carbon dioxide laser (eCO2 ® ablative fractional CO2 laser; Lutronic Corporation, Goyang, Korea) with the following settings: two pass, pulse energy 60 mJ, 30 w and 120 μm pitch.
Each patient was treated three times at 4 week interval using above mentioned laser parameter. Laser therapy was started in 5 week after skin graft.
The same photographer photographed participants using identical camera settings and lighting conditions at every visit (Canon EOS200D, 10.0 megapixels, Tokyo, Japan). The effectiveness of treatment was evaluated using the Vancouver Scar Scale (VSS), the Observer Scar Assessment Scale (OAS) and Patient Scar Assessment Scale (PAS). VSS and OSA was evaluated by an independent plastic surgeon and PAS was assessed by each participants (Tables 2, 3).
In this group, no additional treatment was applied in the skin graft scar exception to moisturizer essential for the postoperative skin graft management. Clinical photography was taken two times at 5th and 21st weeks after the skin graft surgery. With clinical photographs, VSS was assessed by an independent plastic surgeon.
The Wilcoxon Signed Ranks test was used to compare with each pre-treatment and post-treatment scores of VSS, PAS and OAS. Also, statistical differences between the laser groupŌĆÖs VSS and control groupŌĆÖs VSS was tested by Mann-Whitrney U test. MedCalc program version 13.3 (MedCalc software, Ostend, Belgium) was used in statistical analysis.
Mean age of the patients was 50 years old (12ŌĆō80) (Table 3). Mean size of skin grafts was 4.5 cm2 in the laser treatment group and 2.8 cm2 in the control group. Most common cause of defect for skin graft was basal cell carcinoma.
Before the laser treatment, median of VSS was 8 (Min 5, Max 10). After the treatment, median of VSS decreased to 2 (Min 1, Max 3). Wilcoxon Signed Ranks test revealed that P-value was 0.017 between the 2 scores (Table 4).
Before the laser treatment, median of OAS was 26 (Min 25, Max 30) and median of PAS was 23 (Min 24, Max 26). After the treatment, median of OAS was 8 (Min 7, Max 8), and median of PAS changed to 6 (Min 5, Max 7). Both of OAS and PAS decreased significantly after the laser treatment. P-values were 0.018 in OAS and 0.016 in PAS (Table 5).
At 5th weeks after the skin graft procedure, median of VSS in the untreated group was 8 (Min 7, Max 9). Median of VSS was 6 (Min 6, Max 7) 21 weeks after the skin graft. Wilcoxon Signed Ranks test showed statistically significant difference between the 5th and 21st weeksŌĆÖ VSSs (P=0.017) (Table 6).
Median reduction of VSS between 5 week and 21 week of follow up, was significantly higher in laser group (5 [Min 4, Max 8] vs 2 [Min 1, Max 4], P<0.001) than control group (P<0.001) (Fig. 1).
A 40 year-old female initially visited our clinic due to basal cell carcinoma on her left upper brow area. We performed wide excision of the skin cancer and full thickness skin graft that was harvested from pre-auricular area. After the procedure, skin contraction was observed. Fractional CO2 laser was applied using our protocol, 3 times every 4 weeks. After the laser, skin contour had improved, and the texture of skin graft had also softened when compared to the pre-laser state. Her VSS in pre-laser status was 8, and it had improved to 3 after the laser treatment (Fig. 2).
A 24 year-old female underwent the split thickness skin graft that was harvested from upper arm due to deep abrasion and crushing injury in the forehead. Some times after the skin graft, dyschromia, skin contraction and hard texture were complained by the patient. We applied fractional laser to the skin graft scar in accordance with our protocol. After applying the laser 3 times every 4 weeks, skin texture had markedly improved, and the patient was satisfied with the result. Her VSS in pre laser-status was 6, and it had improved to 1 after the treatment (Fig. 3).
In this study, fractional ablative CO2 laser treatment made a significant improvement in VSS, PAS and OAS in the skin graft scar. Of course, VSS is improved in the untreated control group without any treatment in the course of time by scar maturation and remodeling process. However, there was marked reductions of VSSs during the follow-up periods between the untreated and treated groups. These results indicate that carbon dioxide fractional lasers are useful tools to treat skin graft scars.
To evaluate results of treatment, the VSS, PAS, and OSA were used. VSS is most widely received burn scar scale [13,14]. Sometimes, VSS is not enough to make an interpretation the conditions of other scars besides the burn scar. However, before this study design, we paid a special attention to the skin graft scar characteristics similar to those found in the burn scar. As above mentioned, skin graft scars usually has poor skin elasticity, hypertrophy or atrophy and scar depression and this characteristics can be sufficiently expressed by VSS. We consider the VSS that can be an appropriate method to represent the degree of skin graft scar. To complement the VSS, PAS and OAS were added in our study design.
We started the laser therapy at 5th weeks after the skin graft. Optimal initiation time of the fractional laser treatment on scar has not been established till now. Since it has been becoming known that the fractional laser can induce the wound epithelialization quicker than conventional laser, many clinicians opt to initiate the laser therapy in early stage of scar maturation [9-11]. Park et al. insisted the optimal time of fractional laser therapy is 3 weeks after an operation [15]. In this study, we considered the healing time of skin graft is longer than any other scars like the thyroidectomy scar, and we started the laser therapy at 5th weeks after the graft.
Although we did not present all the subcategories of VSS in the results, scores were mostly improved in pliability and height after laser therapy. There was little improvement in vascularity with laser. According to these results, the fractional laser mostly affects the skin pliability and height. However, due to small sample size, definitive conclusion cannot be elucidated in this study.
Antibiotic ointment and ice bag was applied after laser treatment. Complete re-epithelization after an ablative fractional laser treatment generally required 3 to 6 days, compared to 2 to 3 weeks in the traditional CO2 laser systems [5-7,10]. Owing to the rapid re-epithelization, occlusive dressing materials was not necessary.
This study has some limitations. First, number of cases in the treated and untreated groups is too small. To assess the results of small group, the nonparametric test was used. For definitive conclusion, more patients should be recruited in the further study. Second, follow-up period was limited to less than 4 weeks after the last laser therapy. Finally, we were concerned whether laser application to the skin graft scar after wide excision of skin cancer can affect the skin cancer recurrence. The current study observed 3 skin cancer patients for average of 4 years, and no recurrence was observed. We believe that laser and skin cancer recurrence is irrelevant when wide excision of skin cancer and confirmation of negative skin cancer through pathologic analysis is completed. However, more cases should be followed up to prove this assumption.
In this study, the ablative fractional carbon dioxide laser applied to scar formed after skin graft, and significant improvements were observed in the assessment using VSS, PAS, and OAS. Although this study has limitations in sample size of study design, and short follow up period, ablative fractional laser can be an alternative treatment option of skin graft scar management.
Fig.┬Ā1.
Comparison between the laser group and untreated groups. Delta value of each group. Green bar denotes 95% confidence interval. Orange small box in the green bar signifies median of data. Improvement of VSS between follow up periods (between in 5 weeks and 21 weeks after skin graft surgery) is markedly displayed in laser group in compare with control group (P-value < 0.001).

Fig.┬Ā2.
A 40 year-old female patient received wide excision and full thickness skin graft that is harvested from preauricular area. (A) Before the treatment (5 weeks after surgery). (B) After single course of the laser therapy (9 weeks after surgery). (C) Final result. After 3 times of laser therapy, skin texture and fine wrinkles in skin graft were improved.

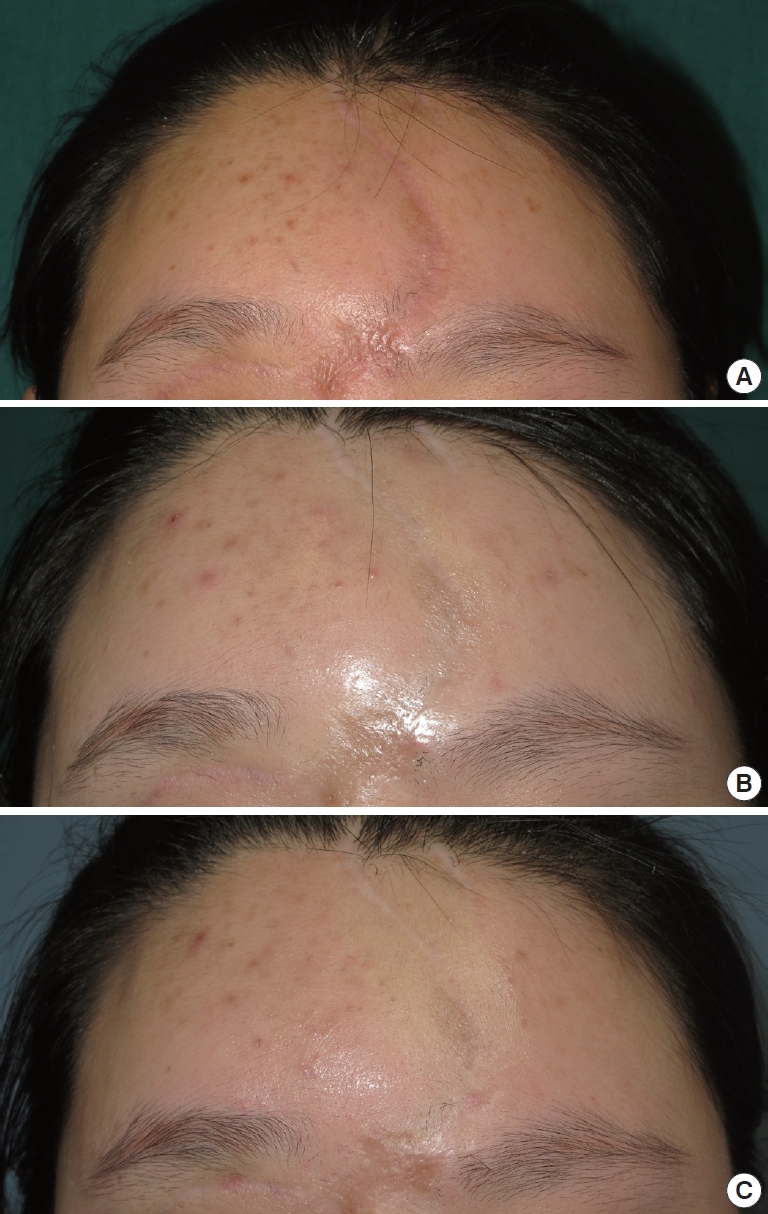
Fig.┬Ā3.
A 24 year-old female underwent the split thickness skin graft that was harvested from upper arm due to deep abrasion and crushing injury in the forehead. (A) Before the laser therapy (5 weeks after surgery). (B) After single course of the laser therapy (9 weeks after surgery). (C) Final result. After 3 times of laser therapy, secondary contraction of skin graft was markedly improved and the skin color underwent improvement to a degree.
Table┬Ā1.
Patient demographic data
Table┬Ā2.
Vancouver scar scale
Table 3.
Observer assessment score and patient assessment score
(A) Observer scar assessment scale
(B) patient scar assessment scale
Table┬Ā4.
Vancouver scar score change in laser treatment group (n = 7)
|
Pre-treatment |
Post-laser treatment |
P-value | ||
|---|---|---|---|---|
| Median | (Min, Max) | Median | (Min, Max) | |
| 8 | (5, 10) | 2 | (1, 3) | 0.017 |
Table┬Ā5.
Observer scar assessment score and patient scar assessment score change in laser treatment group (n = 7)
REFERENCES
2. Ryssel H, Gazyakan E, Germann G, et al. The use of Matriderm in early excision and simulatneous autologous skin grafting in burns-a pilot study. Burns 2008;34:93-97.


3. Ragnell A. The secondary contracting tendency of free skin grafts. British J Plast Surg 1952;5:6-24.

4. Bernstein LJ, Kauvar AN, Grossman MC, et al. Scar resurfacing with high-energy, short-pulsed and flash scanning carbon dioxide lasers. Dermatol Surg 1998;24:101-7.


5. Marqa MF, Mordon S. Laser fractional photothermolysis of the skin: numerical simulation of microthermal zones. J Cosmet Laser Ther 2014;16:57-65.


6. Manstein D, Herron GS, Sink RK, et al. Fractional photothermolysis: a new concept for cutaneous remodeling using microscopic patterns of thermal injury. Lasers Surg Med 2004;34:426-38.


7. Reilly MJ, Cohen M, Hokugo A, et al. Molecular effects of fractional carbon dioxide laser resurfacing on photodamaged human skin. Arch Facial Plast Surg 2010;12:321-5.


8. Ozog DM, Liu A, Chaffins ML, et al. Evaluation of clinical results, histological architecture, and collagen expression following treatment of mature burn scars with a fractional carbon dioxide laser. JAMA Dermatol 2013;149:50-7.


9. Shumaker PR, Kwan JM, Landers JT, et al. Functional improvements in traumatic scars and scar contractures using an ablative fractional laser protocol. J Trauma Acute Care Surg 2012;73:S116-21.


10. Jung JY, Jeong JJ, Roh HJ, et al. Early postoperative treatment of thyroidectomy scars using a fractional carbon dioxide laser. Dermatol Surg 2011;37:217-23.


11. Kim HS, Lee JH, Park YM, et al. Comparison of the effectiveness of nonablative fractional laser versus ablative fractional laser in thyroidectomy scar prevention: a pilot study. J Cosmet Laser Ther 2012;14:8993.

12. Kim SG, Kim EY, Kim YJ, et al. The efficacy and safety of ablative fractional resurfacing using a 2,940-Nm Er:YAG laser for traumatic scars in the early posttraumatic period. Arch Plast Surg 2012;39:232-7.



13. van der Wal MB, Verhaegen PD, Middelkoop E, et al. A clinimetric overview of scar assessment scales. J Burn Care Res 2012;33:e79-87.


-
METRICS

-
- 1 Crossref
- 3,992 View
- 52 Download
- Related articles in AAPS





