The anterior frontal hairline incision has been used for subcutaneous forehead lifts [
1-
8], shortening of the forehead [
9], and endoscopic forehead lifts [
10] in patients with long foreheads. Moreover, it has been used to expose benign tumors such as lipomas and osteomas occurring in the forehead. However, the visible scar resulting from the incision concerned surgeons, although the scar could be camouflaged by a hairstyle change. When performing an anterior frontal hairline incision, surgeons face a dilemma in choosing the incision direction, location, and shape. Until the beveled incision was introduced, an incision parallel to hair direction had been used routinely because it was believed to preserve hair follicles and prevent alopecia, hence providing a less visible scar [
1-
4]. However, the parallel incision did not yield the desirable result, and would occasionally result in a noticeable scar due to alopecia and hypopigmentation. In 1976, Nataf et al. [
11] published their study on scalp flap treatment, claiming that hair grew through the scar when they inserted a dermal graft containing hair follicles beneath the scar. In 1985, Mayer and Flemming [
12] reported that 1~2 mm of the anterior margin of the transposed Juri flap was deepithelialized along the new hairline and sutured to the forehead skin with the expectation of hair growth through the scar. In 1992, Mayer and Flemming [
13] referred to this incision as “trichophytic” (
trich-meaning hair and
phyte, growth). In 1997, Camirand and Doucet [
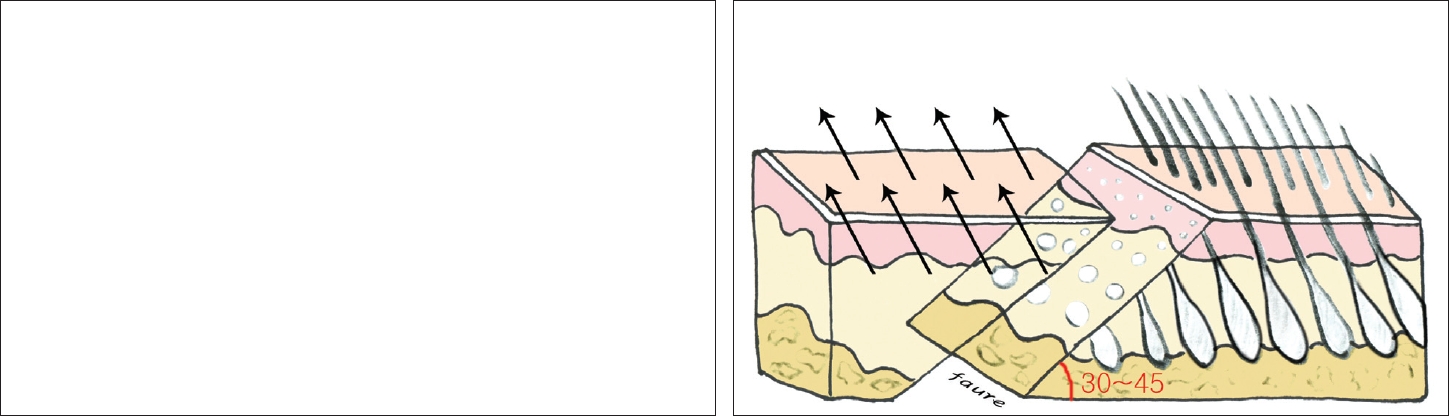
14] conducted a double-blinded comparative study between parallel and perpendicular incision scars from a facelift. They reported that the incision perpendicular to hair follicles provided a more aesthetic result than the incision parallel to hairfollicles and that an incision 30~45° perpendicular to the hair shaft preserved hair follicles in the proximal flap, allowing hair to grow into the scar and in front of the scar. We had the opportunity to compare scars between parallel and beveled incisions in a patient who provided preoperative informed consent, and we obtained the same result as that obtained by Camirand and Doucet [
14] (
Fig. 5), although only 1 patient was observed. In 1998, Ullmann and Levy [
6] evaluated the scars resulting from anterior hairline beveled incisions performed for subcutaneous forehead lifts and reported satisfactory results. The beveled incision should be directed anteriorly because the hair follicles over the frontal scalp are directed anteriorly and inferiorly. Guyuron et al [
10] used beveled anterior hairline incisions in patients who wanted to shorten their long foreheads. However, Ullmann and Levy [
6] did not mention the incision site, whereas Guyuron et al. made an incision at pretrichial area. Even though an anterior beveled incision was made, hair growth might not be expected through the resulting scar if the incision was made at the pretrichial area, because this surface does not contain sufficient hair follicles and papillae. Therefore, making an incision at or in front of the hairline will produce a noticeable scar. Niamtu [
6] advocated a 10~20° beveled incision 4~5 mm behind the anterior hairline, where the follicular density changes. We agree that an incision should be made 4~5 mm or more behind the anterior hairline to obtain a proximal flap with sufficient hair follicles in the beveled surface. Because an incision made inside the scalp was believed to recede the hairline and lengthen the forehead, the anterior hairline incision has long been preferred forthe patients with long foreheads. Several authors [
7,
8] have contraindicated the anterior hairline incision in patients with short foreheads.; however, this seems to be a mistake. The anterior hairline incision can also be used in patients with short foreheads. In our study, a beveled incision was made 4~5 mm behind the anterior frontal hairline in the patients with long foreheads as well as short foreheads. In patients with long foreheads, excessive tissue was removed from the forehead flap, while in patients with short foreheads, residual tissue was excised from the scalp flap using the same beveled incision to meet the counter surface of the forehead flap, which resulted in lengthening of the forehead. Most of the patients with short foreheads were satisfied with the postoperative lengthening of their foreheads. However, the required optimal bevel angle to the skin surface to achieve hair growth through the scar still remains unknown. Camirand and Doucet [
14] reported excellent results with the 30~45° beveled incision, whereas Niamtu recommended a more acute angled incision of 20~30°. In addition to its direction and location, the shape of an incision is likely to affect the final scar. A broken-line scar looks more natural than a straight-line scar. An aesthetic incision with a zigzag shape was recommended by de Benito [
5], and Niamtu [
8] preferred an irregular incision along the undulation of the anterior frontal hairline. Camirand and Doucet [
14] used a micro W incision for better results and postulated that there is a mathematical increase in the real length of the incision (by 41%) with the micro W technique; thus, the minimal tension is decreased by 41%. Tension on the wound is another factor that influences the final scar because melanocytes are extremely vulnerable to tension and ischemia, which induces hypopigmentation of scars. In cases where an incision is required in the temporal region, an anteriorly beveled incision with a similar degree of angle is also recommended because the hairfollicles of the anteriortemporal hairline are also oriented anteriorly and inferiorly [
15]. In ourstudy, there were no complications such as permanent scalp paresthesia and pruritis, which are frequently associated with bicoronal incisions. One patient developed focal alopecia in the temporal scalp but did not request for a scar revision. Most hairline scars in our patients were not easily noticeable and sufficiently acceptable, and did not require any permanent hairstyle change. Moreover, none of the patientsrequested for a scarrevision.