 |
 |
- Search
| Arch Aesthetic Plast Surg > Volume 20(1); 2014 > Article |
Abstract
BACKGROUND
This anthropometric planning is devised for surgeons who assess the esthetic perspectives in Asian rhinoplasty and to provide an easy clinical method using two dimensional photograph. And specific planning in Asian secondary rhinoplasty are also depicted accordingly.
METHOD AND DISCUSSION
In order to use a 2-dimensional digital photograph as a tool for the soft tissue cephalometric analysis (STCA) the surgeon can subjectively rotate the photograph to decide the ideal landmarks. Once this is done, consultation and planning begins. Complicated concepts can be simplified and adaptive ideal points needed in rhinoplasty can be determined according to the Asian concepts of beauty so that it will be used under a clinical setting. Initiation of planning starts by identifying the ideal Sellion and Subnasale, thus, determining the length of the nose. Determination of these two points is the foremost important step in planning. Thereafter, an ideal Tip forms naturally from the nasofrontal angle and the columellar-labial angle. Even with the well performed preoperative planning, the shortcomings in secondary Asian rhinoplasty, such as unexpected scar, may be totally different pitfalls to overcome.
All rhinoplasty starts from accurate planning. Planning of Asian rhinoplasty should be carried out from a different perspective since Asian rhinoplasties are completely different to rhinoplasties in the western part of the world. Asians have a different perspective in beauty, and surgeons not familiar with Asian rhinoplasty techniques attempt to perform a Caucasian rhinoplasty on an Asian nose. The goal of Asian rhinoplasty surgery is not to create a Caucasian nose, but to create a nose that is compatible with the Asian face.
Many Asian rhinoplasty typically involves making the nose larger. This is due to the anatomically low Nasion, low dorsum and underprojected tip. In the last few decades, numerous graft using various materials have been developed for rhinoplasty [1-3].
Apart from the usual nasal bone, septum, and upper and lower lateral cartilage which makes up the bony framework, the resilience and thickness of skin envelope should also be an important factor to consider.
One of the key differences in planning of Asian rhinoplasty is faced during a secondary rhinoplasty. Alloplastic implant augmentation is the most widely performed type of augmentation rhinoplasty in Asia, giving rise to a more complex secondary procedure.
This article was prepared for the practical purpose of explaining the hands-on technique in analyzing the patient using two-dimensional photography, and also to better prepare for secondary rhinoplasties that may arise.
Before taking digital photographs the patients are told to relax and to be at ease. The patients are told to stand up and down 3-5 times to relax the shoulder muscles looking into the mirror in front. It is important to take photographs in which the patient is in his/her natural head position.
To rotate the photographs, Microsoft picture manager┬« (Microsoft Corp. Redmond, WA, USA) was used and micro office sharepoint enabled the program run in 2013 Microsoft Office┬« according to the manufacturerŌĆÖs guide.
Mirror images can be created using ŌĆ£flip the horizontal menuŌĆØ on the program. With respect to the CupidŌĆÖs bow, the surgeon can also decide on the midpoint of columellar base and its direction.
Through consultation, the rotating axis is determined according to the surgeon-patientŌĆÖs preference, then the ideal mid-line is determined. Rotating the photos can be performed using ŌĆ£edit pictures task pane, click rotate by degreesŌĆØ.
A 30 cm ruler is placed in front of the nose when taking lateral photography for better measurement. If the Nasion is too low to visualize in lateral photography the face may be rotated so that the medial portion of the contralateral brow is slightly showing.
When rotating the lateral photography in a clockwise or counter clockwise direction, the FH line is used as a reference with the horizontal line of the photograph. Soft tissue orbitale is marked prior to the photo shoot by taping the right inferior orbital margin.
The ideal nasal length can be planned by the patientŌĆÖs photograph deciding the distance between the ideal Sellion and the ideal nasal Tip. Five ideal landmarks can be reproduced according the adaptive esthetic perspectives on the STCA. From these, the Sellion (S) and Subnasale (Sub) can be estimated and other secondary ideal points such as alar crease junction (ACJ), Pogonion (Pog) and nasal Tip (T) can be marked at the lateral photographs (Fig. 1).
On the lateral view, the ideal sellion is decided at 2-4 mm posterior to the perpendicular line drawn from the FH to the glabella. On the frontal view, this point is located between the mid pupil and lower upper lid margin (Fig. 2).
A natural Subnasale is placed 0-2 mm inferior to the two-thirds of the length of the nose, and 2-4 mm posterior to the superior labrale. It is not always easy to locate the ideal Subnasale, thus, the soft tissue elasticity and the palpable caudal septum should be considered when deciding this ideal points (Fig. 3).
The preferred nasofacial angle starting from the Sellion and the columellar-labial angle automatically determines the ideal point of nasal Tip. The double break of tip lobular angle is also considered (Fig. 4).
On the lateral view, ACJ should be placed more than 2 mm anteriorly than the vertical line drawn from the anterior point of the pupil (Fig. 4).
On the frontal view, a vertical line is drawn from both medial canthi towards the alar base. If the alar base flares more than 0-2 mm from this line, alar base reduction can be considered (Fig. 5).
Nasal bone view x-ray is taken preoperatively to identify the position of the Nasion and the Sellion and also to figure out the implant shape and position relative to the nasal skeleton. The surgeon cannot measure the exact extent of the scar by detailed palpation and even by rhinoscopic examination.
The easiest tool a surgeon can use for rhinoplasty planning is two-dimensional clinical photography. Cephalometry may show the location of the bony Nasion but lacks soft tissue visibility. Therefore, clinical photography plays an important role in planning rhinoplasties as it allows visualization of the lateral view. Despite the advance of three-dimensional imaging, physicians are still using cephalometry when planning for facial bone surgeries. The three-dimensional CT scan can produce rapid protocol models but offers little information needed in planning for rhinoplasty procedure. The notion that CT scans offer a comprehensive evaluation of the nasal bone and helps accurately plan out implant position and shape is a subject of controversy among ŌĆ£radiation phobias.ŌĆØ
Problem with using two-dimensional photograph for analysis is natural head position and the question of attaining a true vertical line [4]. When a patientŌĆÖs photograph is taken preoperatively, the medical photographer may maneuver the patientŌĆÖs head for accurate documentation and planning for surgery. This is different from patientŌĆÖs natural head position. It is important to take photographs in which the patient is in his/her natural head position. We followed the methods described above.
These maneuvers are actually the surgeonŌĆÖs effort to standardize and improve quality control among different patients, thus gaining relatively consistent results. Most people have their chin lifted while taking a picture. Therefore the photograph that the surgeon is seeing is not the patientŌĆÖs normal head posture. When the patient is facing forward in the Frontal view, the face more often than not will be tilting either right or left, showing facial asymmetry. Dental occlusion can also be ascertained by introducing a tongue depressor along the occlusion plane. The tilting habits of the patient may be addressed with the patient with a mirror image of the patientŌĆÖs photograph. Variety of different programs can be used to rotate the two-dimensional photographs for planning. The patient can then offer their preferences on their revised axis and/or posture. Front photos together with its mirror image allowed communication between patient and surgeon by providing a medium through which the surgeon could demonstrate realistic axis of the nose and learned of the patientŌĆÖs desires, such as profile relationships, which might or might not mirror that of the surgeonŌĆÖs preferences.
Similar question of whether it is a ŌĆ£true lateralŌĆØ arises when taking lateral view photographs. On numerous occasions the Nasion is hidden by the eyeball or the upper eyelid. Therefore, when taking lateral view photography one must take into account the amount of eyebrow show on the contralateral side and analyze and plan with the lateral view photography which actually shows the Nasion. Frankfort Horizontal line usually plays as a horizontal guideline and by also considering the true vertical line the extent of tip rotation in a clockwise direction and the length of the nose can be determined preoperatively. On lateral view, nasal-chin relationship should be noted, as a patient with a habit of chin projection may perceive the nose to be upturned. In this case, counter clockwise rotation of the nasal tip should be attenuated. As a patient with inadequate chin projection may perceive the nose to be overprojected when in reality the projection of the nose is adequate. In reality, it is difficult to obtain an accurate profile of the patient, thus, the photograph may be rotated 4 degrees clock-wise or more at the discretion of the surgeon.
Nasion and sellion plays an important part in determining the root of the nose. In STCA the corresponding root is the Sellion. The nasal length can either be tape measured directly on the patient or by the patientŌĆÖs photograph. The distance between the Sellion and the nasal Tip are measured.
One of the ways of determining the length of the nose is by using the golden proportion suggested by Ricketts. Ricketts suggested that nasal length should either be equal to chin vertical measurement (Stomion-Menton) or two-thirds of midface height, and nasal projection should be two-thirds of nasal length. However, these proportions are all female Caucasian parameters. Young people today are seeking plastic surgery for smaller lower facial height (alar base plane-Menton) than the mid facial height (Glabella-alar base plane) (Fig. 6). Thus, the applications of the parameters above are limited [5].
Guyron stated that sellion is the start and ŌĆ£golden pointŌĆØ of the nose and should be located 4-6 mm posterior to the point where the FH and the vertical line meets the glabella [6, 7]. Byrd stated that sellion should be placed on the upper level of the upper eyelid fold and 6 mm superior to the line connecting the two medial canthus [5]. However, it is difficult to apply these values to Asians. Occasionally, it may be difficult to ascertain the vertical line due to a flat glabella in Asians; in this case, the glabella may be identified by taking into account the position of the eyebrow.
Most Asians complain of short nose and want to make their nose longer. It is no exaggeration to say that identifying the Subnasale will ultimately determine the length of the nose. Most Asian rhinoplasties apart from reduction rhinoplasty requires the Subnasale to be placed inferiorly. Adequate resilience of skin envelope and softness is an essential prerequisite for placing the Subnasale inferiorly. Moreover, the success and failure of rhinoplasty may rest upon the position and size of septal caudal margin and its membranous septum. As well, palpation provides the surgeon with the opportunity to determine the nature, volume, strength, and resiliency of the lower lateral cartilages. After dividing the distance between the Sellion and the Stomion into thirds, Guyuron stated that an ideal Subnasale should be 2-3 mm inferior to the two-thirds level and 2-4 mm posterior to the superior labrale. However, again, these values cannot be applied in Asians. Much smaller standards should be took in to consideration when deciding the Subnasale in Asians.
The Tip on the other hand compared to the Sellion and the Subnasale tend to form more automatically. In other words, all other parameters should be confirmed first before deciding on the Tip. The nasofacial angle measuring around 30 degrees and the columellar-labial angle between 90 and 105 degrees automatically determines the ideal point of nasal Tip. A double break is noted between the columella and nasal tip; this double break is created by the intermediate crura of the lower lateral cartilages and plays a key role in giving a natural ŌĆ£lookŌĆØ. An aesthetic tip lobular angle is made when the dome and the middle crura are in harmony. However, most middle crura in Asians are weak and small requiring grafts to reinforce and strengthen the middle crura. Shield graft for example, is the most effective.
The position of the alar crease junction plays an important role in mid face surgery. The patient may need perialar augmentation if the ACJ is retreating back. Apart from this, the lower margin of the nostril and the columella which make up the alar columellar relationship (ACR) also needs to be considered. However, due to its vast content this will be dealt separately. A competent plastic surgeon will consider the position of the chin when ascertaining the nasal tip. Also the ideal chin should be discussed in detail as it has a vast content of its own.
The analysis stated above are standard criteria for primary rhinoplasty. Due to the recent rise in secondary rhinoplasty it is important to understand the components mentioned below before planning for rhinoplasty since technical competence far outweigh identifying ideal points. The planning of secondary Asian rhinoplasty is completely different to the basic principles stated above. The unpredictability of scar tissue formation from previous operation(s) and the destruction of lower lateral cartilage can only be seen once the surgery has begun.
Although the Sellion is the soft-tissue correlate of the Nasion, the Sellion is often placed more superiorly or inferiorly due to soft tissue envelope (Fig. 7, 8). Occasionally patients who had a previous augmentation rhinoplasty complain of long nose, this phenomenon is because the Sellion was pushed upwards due to implant insertion. The surgeon must be prepared for the translocation of the Sellion during secondary rhinoplasty and provide for such changes.
Secondary rhinoplasty is regarded among the most challenging of all cosmetic endeavors. First, secondary rhinoplasty takes far more time. This is because of the obstacles posed by scar tissue and destruction of skeletal framework from previous surgery making dissections far more difficult. In addition to increased treatment time, secondary rhinoplasty nearly always requires the use of graft material. Graft material is usually in the form of cartilage, which is harvested from the patientŌĆÖs own body. Unfortunately, patients may not have sufficient surplus cartilage to rebuild a badly damaged nose. Surgeons are then forced to seek other tissue substitutes.
Another dilemma during secondary rhinoplasty is deciding on the extent of soft tissue dissection. Soft tissues overlying the nasal skeleton, such as skin, muscle, fascia and fat are unavoidably injured during any rhinoplasty. But unlike virgin soft tissues which tend to tolerate surgical disruption with minimal inflammation, swelling or scar formation, previously operated tissues exhibit inflammatory responses that are typically more severe and which may potentially compromise the cosmetic outcome. In patients with severe contracture extensive dissection is needed around the nasal bone and piriform aperture. Additional dissection may be needed around the transverse nasalis muscle to fully lift the soft tissue blanket.
Even after lifting the skin envelop additional dissection and release between the nasal skeleton is needed to successfully relocate the ideal points. The following areas to be dissected are: the junction between the upper lateral cartilage and the nasal bone together with its muchoperichondrium, the subperichondrium between the upper lateral cartilage and the septum, the scar tissue between the upper and lower lateral cartilage, and the submucoperichondrial plane between the lower lateral cartilage including its membranous septum. Moreover, capsule formation from previous implant insertion can be salvaged or sometimes need to be removed fully for the purpose of eradicating all scar tissues.
A patient who complained of her long looking nose after the previous augmentation rhinoplasty went through the adaptive anthropometric planning. An L-type thin and long silicone implant was found on the X-ray and her Sellion was displaced upwardly. The ideal Sellion should be located inferiorly and the ideal Subnasale was decided to be located superiorly to shorten the nasal length. The implant was changed with preserving the anterior capsule according to the planned shape and columellar strut with columellarseptal suture was performed. And perinasal augmentation was performed using folded Gore-Tex® to locate the ideal ACJ more anteriorly (Fig. 7A-D).
A patient who suffered from contracted nose due to the previous implanting went through the same adaptive planning described above. Also an L-type thick implant was found and it was displaced upwardly, and her Sellion was located downwardly. The ideal Sellion was decided to be located more superiorly and her ideal Subnasale was planned to be located inferiorly to lengthen the nose. The implant and surrounding scars was removed totally and her septum was reconstructed by making her septal L-strut extended anteriorly and caudally using the carved her 6th rib. Additional graft at her nasal root and perinasal area was performed using the remaining rib cartilage (Fig. 8A-D).
Simplified preoperative anthropometric planning using the 2 dimensional digital photographs is modified from Western standards to Asian perspectives. Initiation of planning starts and also ends by identifying the ideal Sellion and Subnasale considering the resilience of the soft tissue, thus, the incremental length of the nose can be determined clinically even in the secondary Asian rhinoplasties.
Fig.┬Ā1.
The STCA landmarks: Sellion (S), Subnasale (Sub), alar crease junction (ACJ), Pogonion (Pog) and nasal Tip (T) are indicated.
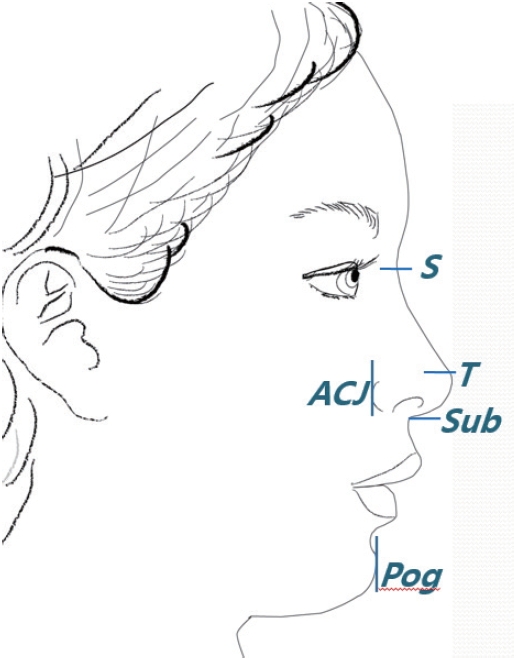
Fig.┬Ā2.
Ideal Sellion (Si): 2-4 mm posterior to the perpendicular line drawn from the FH to the glabella located between the mid pupil and lower upper lid margin.
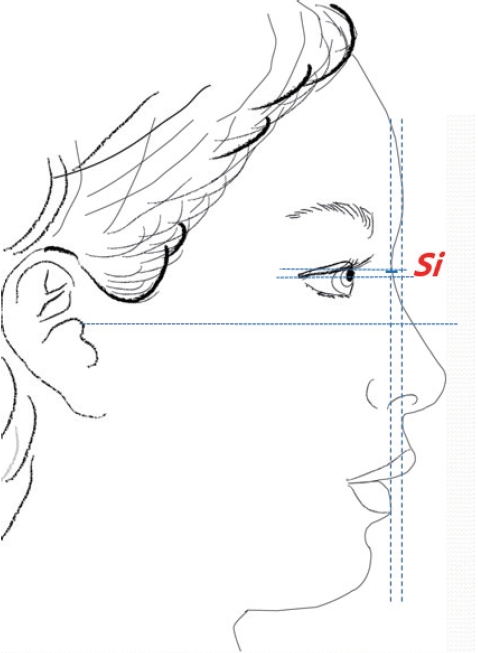
Fig.┬Ā3.
Ideal Subnasale (Subi): 0-2 mm inferior to the two-thirds of the length of the nose (Si-Sto), 2-4 mm posterior to the superior labrale, Sto: Stomion.
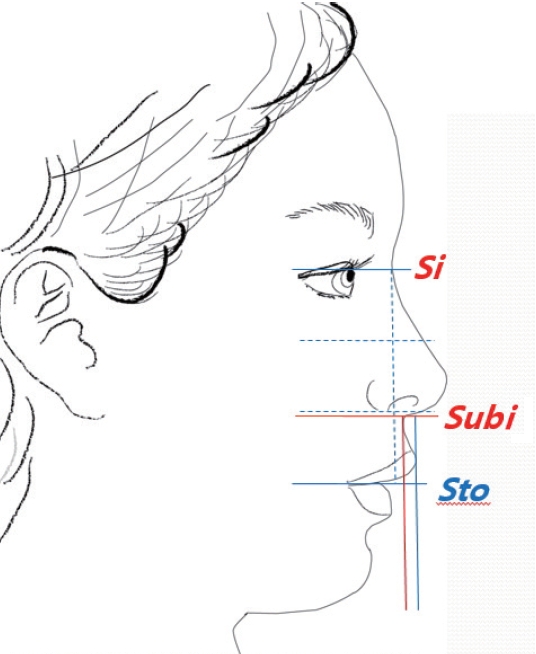
Fig.┬Ā4.
Ideal Tip (Ti) and ideal alar crease junction (ACJi): the nasofacial angle and the columella-labial angle automatically determines Ti: ACJi should be placed anteriorly than the pupil.
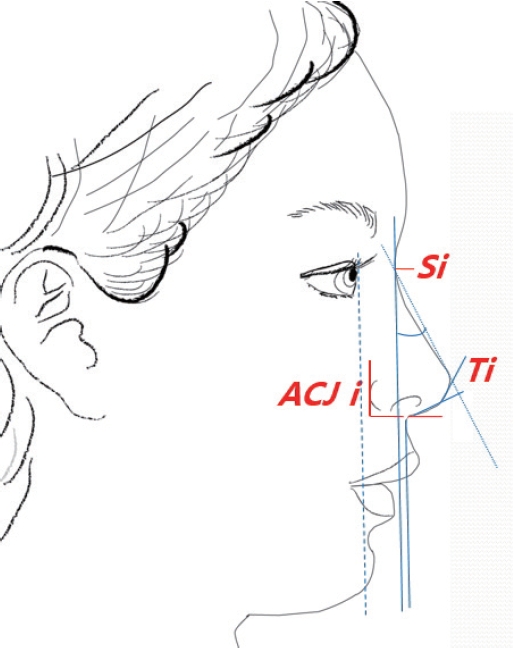
Fig.┬Ā5.
Nasal width: vertical line drawn from both medial canthi towards the alar base. The alar base flares should be not more than 0-2 mm from this line.

Fig.┬Ā6.
Facial proportion: middle facial height (MFH), lower facial height (LFH), Glabella (G), alar base plane (ABP), Stomion (Sto) and Menton (Me).
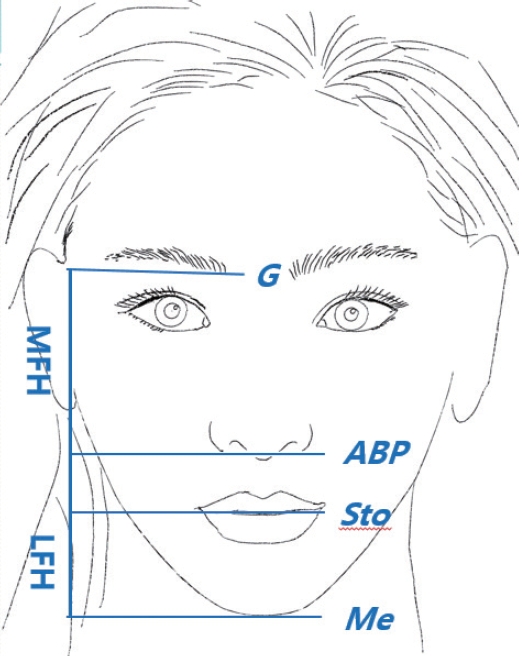
Fig.┬Ā7.
A case of secondary rhinoplasty correcting the long nose (A) preoperative photo, (B) planning of lowering the ideal Sellion, lifting the ideal Subnasale and locating the ideal ACJ anteriorly; ideal points are red, (C) Sellion was displaced upwardly due to the implanting (arrow with asterisk: Sellion displaced upwardly, arrow: original Nasion), and (D) postoperative photo (A-D).
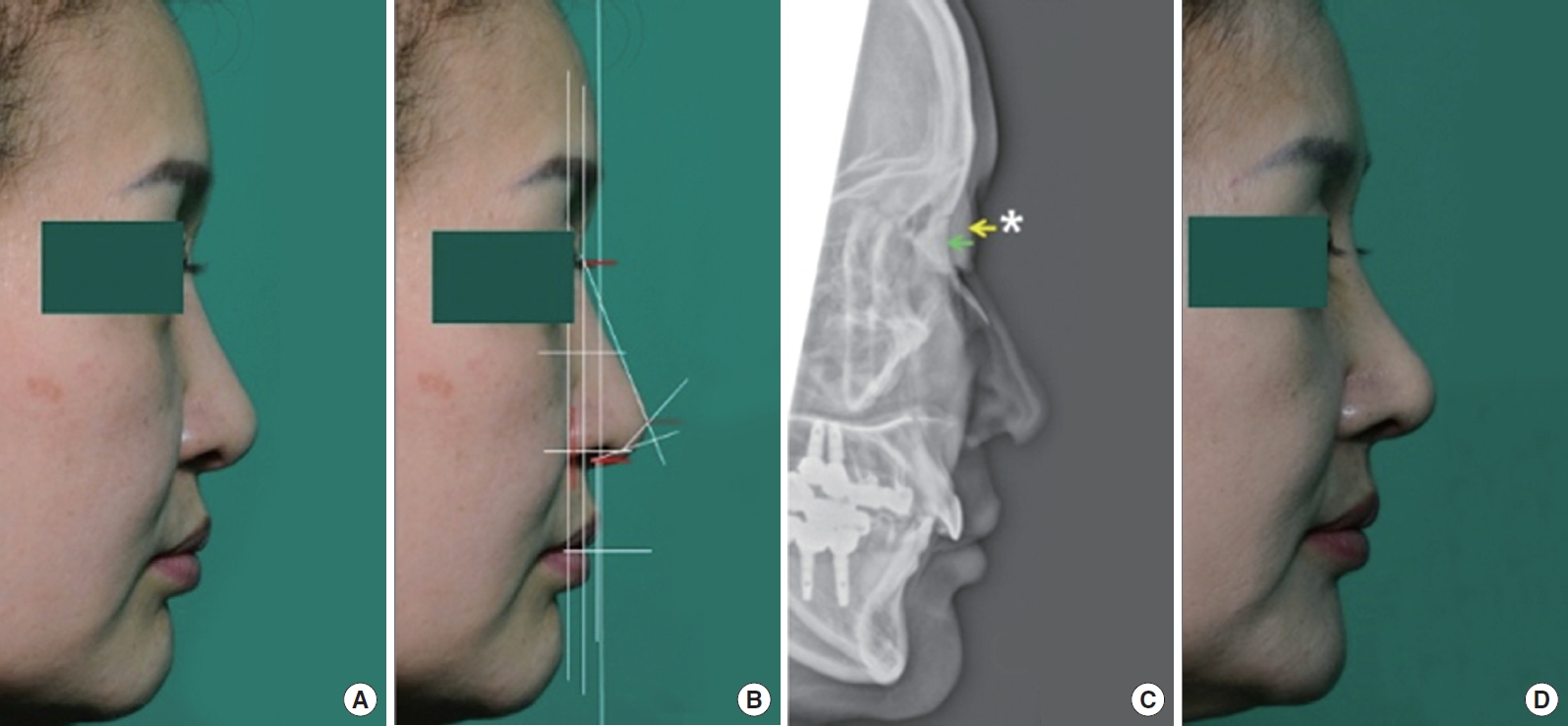
Fig.┬Ā8.
A case of secondary rhinoplasty correcting the short nose: (A) preoperative photo, (B) planning of lengthening the ideal Subnasale and changing the tip angles; locating the ideal Sellion superiorly and the ideal ACJ anteriorly, (C) Implant was found displaced upwardly, and Sellion was located low (arrow with asterisk: Sellion displaced downwardly, arrow: original Nasion), and (D) photo of 1 month postoperatively (A-D).

REFERENCES
1. Gunter JP, Landecker A, Cochran CS. Frequently used grafts in rhinoplasty: nomenclature and analysis. Plast Reconstr Surg 2006;118:14-29.

2. Sajjadian A, Rubinstein R, Naghshineh N. Current status of grafts and implants in rhinoplasty: part I. Autologous grafts. Plast Reconstr Surg 2010;125:40-9.

3. Sajjadian A, Naghshineh N, Rubinstein R. Current status of grafts and implants in rhinoplasty: Part II. Homologous grafts and allogenic implants. Plast Reconstr Surg 2010;125:99-109.



4. Madsen DP, Sampson WJ, Townsend GC. Craniofacial reference plane variation and natural head position. Eur J Orthod 2008;30:532-40.



-
METRICS

-
- 1 Crossref
- 5,197 View
- 86 Download
- Related articles in AAPS
-
Lateral Osteotomies in Oriental Rhinoplasty.1998 September;4(2)
Application of Osteotomies in Aesthetic Rhinoplasty.2010 February;16(1)





