|
 |
- Search
| Arch Aesthetic Plast Surg > Volume 26(2); 2020 > Article |
|
Abstract
Background
In light of increasing demands for the use of a shorter incision during implant-based reconstructive surgery due to a paradigm shift to short-incision mastectomy and prior radiotherapy, as well as concerns about breast implant contamination, the use of funnels during implantation is recommended. We aimed to describe our preliminary experiences with funnel-assisted implant insertion and to determine the indications for funnel usage in reconstructive breast surgery.
Methods
A series of 15 consecutive patients who underwent funnel-assisted implant insertions between March 2018 and January 2019 were included. Funnel-assisted implantation was indicated in patients with a small linear scar (<5 cm) at the mastectomy site and those who previously underwent chest radiotherapy before implant insertion.
Results
Eight patients (53.3%) previously received radiotherapy, while seven (46.6%) underwent total mastectomy using a short incision. In all mastectomy patients, the mean incision length was 4.73 cm (range, 4.5–5.5 cm), while that of patients who previously received radiotherapy was 4.62 cm. The patients did not develop wound-related complications (e.g., major and minor skin necrosis). At 6- and 12-month follow-ups, no patients showed definite capsular contracture (Baker grade III and IV).
Conclusions
The study confirmed that the use of a highly durable and elastic funnel enabled reconstructive surgeons to perform “no touch” implantation using a short incision. This technique is beneficial for patients who previously received radiotherapy and reduces the risk of wound-related complications through the use of a shorter skin incision.
There has been an increasing demand for breast reconstruction after mastectomy worldwide. Although a variety of reconstruction methods can potentially be used, implant-based breast reconstruction is a popular method that has the advantages of preventing sacrifice of the donor site and yielding excellent cosmetic outcomes [1]. During permanent implant insertion, which involves the implant being inserted into the breast pocket, the implants are carefully scrutinized for the presence of microbial biofilms caused by contamination of the implant with skin flora, and studies established an association between biofilms and capsular contracture [2]. Furthermore, although the definite pathogenesis of breast implant-associated anaplastic large cell lymphoma has not yet been established, chronic inflammation from indolent infections and interactions between the textured surface of the implant outer shell and the surrounding host tissue have been recently proposed as a potential factor leading to the stimulation and malignant transformation of T cells around the surface of the implant [3].
Therefore, using a “no touch” technique during implant insertion is essential in implant-based breast surgery. Introduced in 2009, the Keller funnel (Keller Medical, Inc., Stuart, FL, USA) is widely used in cosmetic breast surgery. This device allows surgeons to insert breast implants without touching the patient’s skin, thereby decreasing the risk of skin flora contamination, promoting the creation of smaller incisions, reducing implant trauma during insertion, and even shortening the time needed to push the implant through the incision [4,5]. In a cadaveric study, the use of funnels resulted in a 27-fold decrease in skin contact for all smooth round gel implants [2]. A retrospective cohort study that was conducted in 2,800 patients in whom the Keller funnel was used reported a statistically significant reduction in the prevalence of grade III capsular contracture 12 months after primary breast augmentation using round implants [4].
In the field of reconstructive breast surgery, whether the “no touch” technique is a realistic goal during implantation procedures remains a topic of debate. Traditionally, long skin incisions are made for implant insertion after mastectomy in order to facilitate the insertion of implants; hence, demand for the use of funnels during implant insertion was previously low. Recently, shorter skin incisions have frequently been made during reconstructive breast surgery. With the transition from wide skin excision mastectomy to skin-preserving mastectomy or nipple- and areolar-sparing mastectomy, these techniques have been established as oncologically safe procedures for patients with early-stage breast cancer. Hence, the length of the incision created at the implant insertion site is usually shorter in these types of mastectomy procedures, while the implants used in breast reconstruction are generally larger than those used in breast augmentation [6]. Furthermore, some breast reconstruction patients undergo radiotherapy before implant insertion. In a study of patients who underwent radiotherapy prior to skin-preserving mastectomy, wound-related complications such as impaired wound healing, wound dehiscence, and skin necrosis occurred much more frequently (in 10%–23.5% of irradiated breasts) than in non-irradiated patients (in 1%–2% of breasts) [7]. Therefore, a shorter incision is frequently required in order to minimize wound-related complications such as delayed healing, wound dehiscence, and wound breakdown.
Under these circumstances, it is more difficult to apply the “no touch” technique when manually inserting a large breast implant through a shorter incision using only sterile retractors. Hence, funnels should be used during implantation, even in reconstructive breast surgery. To our knowledge, the insertion of implants through a funnel using the “no touch” technique has not yet been established in the field of reconstructive breast surgery. Hence, we aimed to describe our preliminary experiences of funnel-assisted implant insertion in patients who underwent reconstructive breast surgery and to determine definitive indications for funnel usage in reconstructive breast surgery.
The present study included a series of 15 consecutive patients who underwent funnel-assisted implant insertions for implant-based breast reconstructions between March 2018 and January 2019. In the study, funnel-assisted implant insertion through a short incision was primarily indicated for patients with a small linear scar (length of <5 cm) on the mastectomy site and a history of chest radiotherapy prior to implant insertion.
The Art funnel (Art Meditech, Seoul, Korea), which is composed of a rip-stop nylon sleeve with a hydrophilic inner coating, was used during implant insertion. This hydrophilic inner coating of the funnel can lower the coefficient of friction (Fig. 1). Therefore, this funnel allows the implant to slide into the pocket smoothly and minimizes implant trauma during insertion, while the funnel acts as a barrier against the transmission of skin flora. This retrospective study was reviewed and approved by the Institutional Review Board (IRB No. 2020-01-001) for human subject research, and patient consent was obtained.
All reconstructive procedures were performed by the researcher (SYK) in this study. Before implant insertion, the incision length was measured in all cases and the expected breast pocket for permanent implants was made. A drain was inserted into the breast pocket. All patients were skin-prepped with betadine solution, and the pockets were irrigated sufficiently with an antibiotic solution containing 500 mL of normal saline mixed with 1 g of cefazolin, 80 mg of gentamicin, and 10% povidone solution. The implants were also cleaned and soaked in 10% betadine for 3 minutes before implantation. Considering the implant shape (anatomical or round), volume, and size (especially projection), the distal end of the funnel was trimmed and inserted into a large opening in accordance with the recommended protocols. This allows a smooth and gentle passage of the implant through the funnel and into the breast pocket. Usually, when the volume of the implant is less than 315 mL, trimming is not required. When any type of anatomical implant is to be inserted, the funnel mouth should be 2 cm wider than in the original protocol. Then, the funnel is immersed in a basin of sterile saline to make the inner surface slippery and to induce a low-friction internal surface. Next, the implant is loaded into the large proximal end of the funnel. For anatomical implants, precise loading of the implant through the large proximal end of the funnel and verification of the position of the implant within the distal end of the funnel are essential to avoid implant malposition. The narrow opening of the funnel is placed 1 cm from the center of the surgically prepared and irrigated implant pocket, and a clean retractor is inserted into the pocket. When the incision opening was located in the lateral region of the breast from the breast center, we tried to relocate the opening into the center of the breast using clean retractors. The implant was advanced through the funnel and into the pocket with minimal force and without finger manipulation. During anatomical implant insertion, this kind of implant should be gently and evenly squeezed into the funnel hole, smoothly propelling it forward into the center of the plastic pocket so that it can lodge in the correct location without malrotation. Finally, the exact location of the implant (vertical position) in the plastic pocket was confirmed. Specific cases are presented in Figs. 2 and 3.
Demographic data such as age, obesity (i.e., body mass index >30 kg/m2), diabetes, hypertension, other medical comorbidities, and current smoking (defined as active cigarette use within 4 weeks before surgery) were collected. Patients who previously underwent chest radiotherapy as a breast conservation treatment or postmastectomy adjuvant treatment were investigated. Furthermore, data of patients who received other cancer-related treatments including adjuvant chemotherapy, hormone therapy, and oncogene target treatment were also reviewed. To determine the outcomes of the funnel-assisted implantation technique, the patients were assessed for the presence of immediate postoperative complications, such as infection, seroma, major skin necrosis necessitating surgical treatment, and minor skin necrosis. At 6- and 12-month postoperative follow-ups, the patients were assessed for the presence of capsular contracture, and the degree of contracture was assessed using the Baker classification. Furthermore, patients were also examined for the presence of infection, hypertrophic scarring, and malposition of the anatomical implant.
The mean age of the patients was 44 years (range, 38–54 years). None of the patients had obesity or comorbidities such as diabetes or hypertension. Ten patients (66.6%) underwent a skin-sparing mastectomy, while five (33.3%) underwent a nipple-sparing mastectomy. Except for one patient who underwent augmentation mammoplasty and had a previous history of breast-conserving surgery and adjuvant radiation therapy, most patients underwent two-stage implant-based breast reconstruction because most patients, especially those who underwent nipple-sparing mastectomy, had relatively thin mastectomy skin flaps without no assurance of sufficient tissue viability for the mastectomy flap. The first stage involved the insertion of a tissue expander into a sub-pectoral dual plane, after which the lower lateral portion of the expander was covered with an acellular dermal matrix (ADM; CGCryoDerm, CGBio Co., Seongnam, Korea); the second stage involved the insertion of a permanent implant.
With regard to the indications of funnel-assisted implantation, eight patients (53.3%) had a history of radiotherapy, and seven (46.6%) had a small linear scar at the site of total mastectomy. Two of the patients who previously underwent radiotherapy received chest wall radiation therapy after breast conservation treatment and six received postmastectomy adjuvant treatment after total mastectomy (postmastectomy radiation therapy; PMRT). According to our expansion protocols for PMRT patients, expansion started 3 weeks after mastectomy and the goal volume was reached before the start of PMRT. After PMRT was completed, a minimum period of 6 months was observed for consolidation of the expansion before proceeding to the second stage. The mean period from the end of PMRT to funnel-assisted permanent implant insertion surgery was 10.3 months (range, 6–21 months).
All implants were inserted by making an incision into the previous scar. The mean incision length of all patients was 4.73 cm (range, 4.5–5.5 cm). Among patients with a history of radiotherapy, the mean incision length was 4.62 cm. The cohesive gel implant used was BellaGel (HansBiomed Co., Ltd., Seoul, Korea). A round smooth implant was used in eight patients (53.3%), and a round micro-textured implant was used in five patients (33.3%). An anatomical implant (macro-textured type) was used in two patients (13.3%) (Table 1). The volume of the implants ranged from 125 mL to 425 mL.
In the immediate postoperative period, none of the patients developed infection or seroma. As wound-related complications, neither major nor minor skin necrosis developed. At 6- and 12-month follow-ups, grade III or IV capsular contracture did not occur. Furthermore, hypertrophic scars and malposition of anatomical implants were not detected.
To date, the infection hypothesis, which suggests that subclinical infection may be the primary cause of capsular contracture in patients who undergo augmentation mammoplasty, has been strongly supported [8]. Because the terminal ducts at the nipple and areola are colonized with endogenous flora and the skin is not a sterile organ, contamination occurs when a sterile implant comes in contact with the skin and nipple-areolar complex. Most surgeons who perform breast implant surgery usually follow the “no touch” technique during implant insertion by using nipple shields (placing a waterproof film over the nipple-areolar complex), vigorously irrigating the pocket with an antibiotic solution, changing gloves, and re-preparing the skin prior to implantation. Although these methods help decrease the risk of contamination by reducing the bacterial burden, they do not totally prevent the risk of implant-to-skin contact, and the use of the “no touch” technique, which involves direct insertion of the breast implant into the breast pocket without touching the instruments, drapes, gloves, or the patient’s skin and parenchyma, is recommended.
Introduced in 2006, the funnel, composed of rip-stop nylon with a hydrophilic internal coating, is an innovative device that allows the delivery of the implant from its packaging into the breast pocket without touching the instruments, drapes, gloves, or patient’s skin and breast parenchyma [2]. By using a funnel, surgeons could perform the “low touch” surgical implantation technique in a saline-only area using a more advanced “no touch” implantation technique. Furthermore, by using the funnel, the amount of vigorous finger pushing and finger fatigue is reduced. Vigorous finger pushing not only increases the risk of implant contamination, thereby elevating the risk of subsequent capsular contracture, but it can also compromise the integrity of the outer shell of the implant, thereby increasing the risk of post-implant leakage or rupture. In fact, both Mentor and Allergan silicone implant product guidelines clearly recommend that excessive force should not be applied to any portion of the implant to avoid compromising the integrity of its outer shell, which can increase the risk of post-implant leakage or rupture. According to recent studies, up to 80% of surgeons use the funnel device, and it is widely regarded as essential for implant insertion during cosmetic augmentation mammoplasty [9]. In implant-assisted breast reconstruction, using the “no touch” technique is important during implantation, as well as during augmentation mammoplasty. According to long-term data from patients with anatomical implants, the incidence of capsular contracture was significantly higher among those who underwent reconstructive breast surgery using implants than among those who underwent augmentation mammoplasty [10].
Demand for the use of a funnel during implant insertion has recently increased for several reasons. Previously, long incisions were generally made for total mastectomy in order to facilitate the smooth insertion of implants without finger manipulation. However, with the increasing rate of skin-sparing and nipple-sparing mastectomy, shorter incisions are made and the risk of bacterial contamination from the skin and nipple-areolar complex is also higher. During mastectomy, peri-areolar incisions performed under an endoscope or using the inframammary approach are preferred by general surgeons as they provide better aesthetic outcomes; hence, shorter skin incisions are used in these types of mastectomy than in other approaches. Under these circumstances, funnel-assisted implantation through a short incision is necessary in order to avoid vigorous implant insertion, which could lead to mechanical injury during implant insertion and implant contamination.
Second, as the primary treatment for patients who undergo breast-conserving therapy or as an adjuvant treatment for those with locally advanced breast cancer, radiotherapy to the chest wall is performed with increasing frequency in breast cancer patients. Of course, the option of autologous breast reconstruction is preferred in patients with a history of prior radiation treatment. However, some patients strongly prefer to undergo prosthesis-based breast reconstruction because of their reluctance for donor site sacrifice. Further, in some cases, the choice was made to administer adjuvant radiation treatment based on postmastectomy biopsy results. The detrimental effects of radiation, such as poor tissue quality and diminished healing of the mastectomy skin flap, remain a challenge for breast reconstructive surgeons. Sbitany et al. [11] reported an association between prior radiation therapy and wound breakdown in patients who underwent implant-based breast reconstruction after total skin-sparing mastectomy. de Araujo et al. [12] also reported that the breast-related complications such as infection, major skin necrosis, and capsular contractures (Baker grades II–IV) were significantly more common in patients who underwent reconstruction after receiving radiotherapy. Moreover, patients with prior radiation therapy were 3.5 times more likely to develop skin necrosis. Based on these results, after performing reconstructive breast surgery in patients with a history of chest radiotherapy, funnel-assisted implant insertion through a small incision (<4.5 cm) and minimal undermining of the mastectomy skin flap were performed to reduce the risk of wound-related complications caused by poor skin flap vascularity and weak healing potential. Sometimes, if a discrepancy in the distance between the skin incision and the upper margin of the ADM or serratus fascia is detected, excessive undermining of the mastectomy skin flap is not performed to reach the upper margin of the ADM or serratus fascia. Instead, the pectoralis muscle is transected at the location of the skin incision to open the subpectoral pocket (Fig. 4). In the present study, eight patients (53.3%) had a history of chest radiotherapy prior to implant insertion. They did not develop wound-related complications and showed favorable wound healing progress.
In the present study, we used the Art funnel (Art Meditech), which has been newly developed and marketed in South Korea. Using polymeric vinyl and a hydrophilic coating for internal lubrication, the Art funnel has a thickness of 0.25 mm and is highly durable and elastic, allowing the implants to smoothly pass through the narrow and localized-pressured tunnel. If the edge of the funnel exit is not durable and elastic, the edge could be inverted when a large implant is propelled under high pressure. With regard to the clinical use of the Art funnel, we observed good eversion along the exiting implant surface with proper elasticity, indicating that a smooth shot can be performed. Due to its durability, the risk for malrotation is low, even if a propelling force is applied to the implant within the funnel exit. Moreover, the exact position of an anatomical implant in vivo can be precisely determined following insertion using the Art funnel. Additionally, the Art funnel has to break the surface to avoid the backward slipping of implants inside the internal tunnel, which was not observed in other funnel products. Some surgeons have reported using a plastic insertion sleeve that is open on both sides. Although this technique is beneficial in terms of cost, implant malrotation or migration can occur when the sleeve is removed, as the implant does not fit well inside the sleeve [13]. Furthermore, the use of an anesthetic gel to lubricate the sleeve pocket is required.
Based on our clinical experience in implant-based reconstructive breast surgery, funnel-assisted implant insertion is indicated in (1) patients with a small linear scar on the mastectomy site of less than 5 cm, which is usually the case in procedures performed using the inframammary fold approach, peri-areolar mastectomy, and lateral incision mastectomy; (2) patients with a history of chest radiotherapy as an adjuvant treatment or primary treatment following breast-conserving surgery; and (3) patients with a large discrepancy in the distance between the mastectomy skin flap incision and the upper margin of the ADM or serratus fascia, thus requiring transection of the pectoralis muscle, serratus fascia, or ADM. In cases of transection of the muscles, fascia, or ADM, the funnel should be used during implantation to minimize soft tissue damage caused by vigorous manual implant insertion, as described in the case presented in Fig. 3.
The present study has several limitations. First, the study had a small sample size and lacked consistent and long-term data to confirm whether capsular contracture occurred 3 or more years after reconstructive surgery [14]. As the Art funnel was introduced to the market only 2 years ago, only preliminary and short-term clinical evidence was presented in this study. Furthermore, several factors cause capsular contracture, including the staging of breast reconstruction, incision placement, implant size, implant type, and even patients’ demographic characteristics. Notably, the present study included patients who underwent two-stage breast reconstruction, so there remained a potential risk of subclinical infection developing in the first stage, and this risk, to which capsular contracture might be attributed, could not be excluded despite funnel-assisted implantation in the second stage. A more controlled study with multivariate analysis should be required. Nevertheless, this was the first study to demonstrate the importance of funnel use during implantation in reconstructive breast surgery and to suggest specific indications for funnel-assisted implantation.
As the use of a funnel can reduce the risk of implant contamination and localized stress to the implant caused by vigorous finger pushing, the present study confirmed that the Art funnel, which is highly durable and elastic, allows reconstructive surgeons to perform the “no touch” implantation technique and properly position the anatomical implant through a short incision. The funnel-assisted implantation technique is beneficial for patients with history of radiotherapy and reduces the risk of wound-related complications, as a shorter incision is used.
Notes
Ethical approval
The study was approved by the Institutional Review Board of Sanggye Paik Hospital (IRB No. 2020-01-001) and performed in accordance with the principles of the Declaration of Helsinki.
Patient consent
The patients provided written informed consent for the publication and the use of their images.
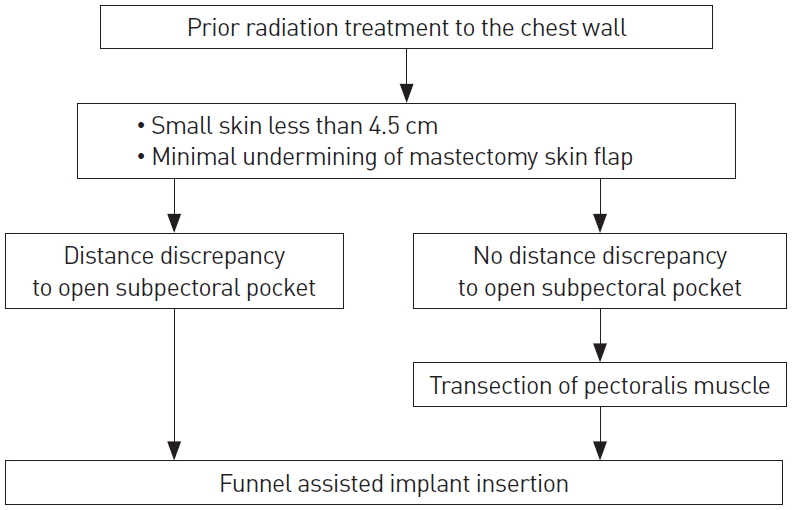
Fig. 1.
Image of the Art funnel used in the present study. Permission to use an image was obtained from the Art Meditech.
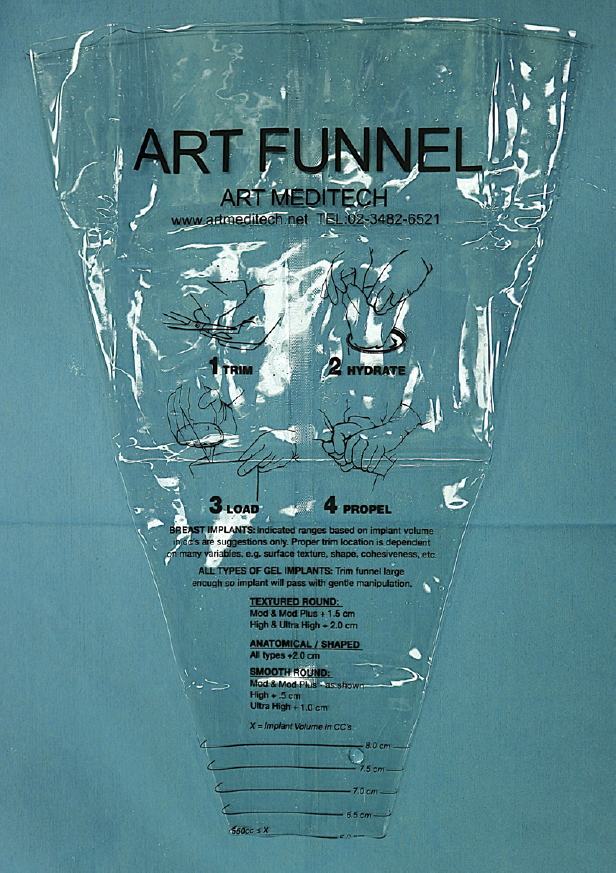
Fig. 2.
A 38-year-old female patient who underwent skin-sparing mastectomy and immediate breast reconstruction with insertion of a tissue expander 15 months previously and was treated with adjuvant postmastectomy radiation therapy underwent another operation to remove a 130-mL inflated expander and to insert a 165-mL smooth round permanent implant. (A) Preoperative design of lowering the inframammary fold and incision. (B) As the patient had a history of radiotherapy prior to the insertion of the permanent implant, a 4.0-cm short incision and minimal undermining between the mastectomy skin flap and pectoralis major muscle were planned, although the previous skin-sparing mastectomy incision length was 9 cm, and capsulectomy and undermining of the mastectomy flap in the inframammary fold area was done. (C) A 165-mL round smooth implant was loaded into the funnel without trimming the exit site, and the narrow opening of the funnel was placed 1 cm into the center of the surgically prepared and irrigated breast pocket. (D) Immediate postoperative image of funnel-assisted implant insertion.

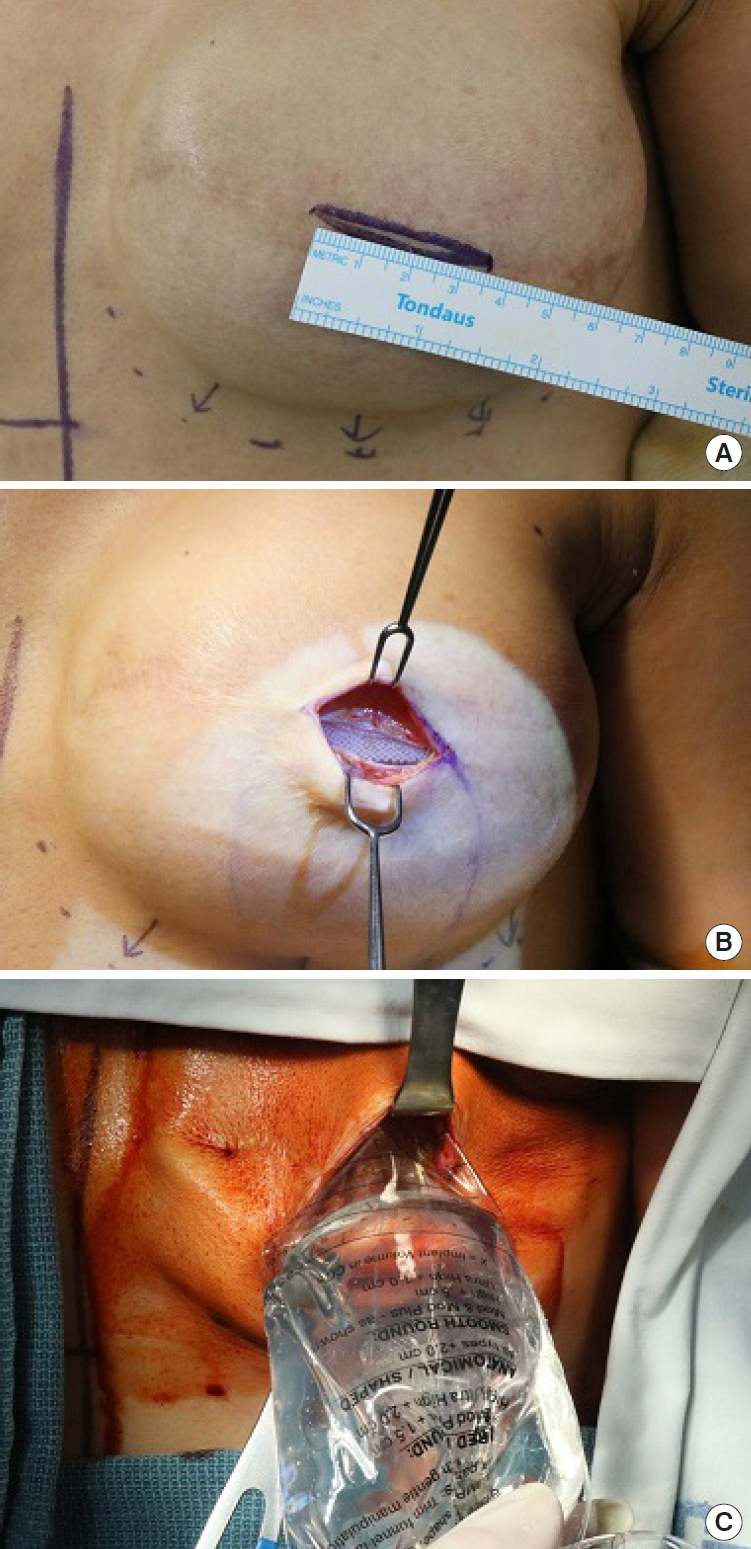
Fig. 3.
A 50-year-old female patient who underwent skin-sparing mastectomy and immediate breast reconstruction with insertion of a tissue expander 20 months previously and was treated with adjuvant chemotherapy and postmastectomy radiation therapy. A 250-mL inflated expander was removed, and a 150-mL smooth round permanent implant was inserted. (A) As the patient had a history of radiotherapy prior to the insertion of the permanent implant, a 4.0-cm short incision was created. (B) After scar tissue excision, minimal undermining between the mastectomy skin flap and pectoralis major muscle and horizontal transection of the pectoralis muscle (length, 4.0 cm) were performed. (C) A 165-mL round smooth implant was inserted through the funnel into the surgically prepared and irrigated breast pocket.
REFERENCES
1. Baek WY, Byun IH, Kim YS, et al. Patient satisfaction with implant based breast reconstruction associated with implant volume and mastectomy specimen weight ratio. J Breast Cancer 2017;20:98-103.



2. Moyer HR, Ghazi B, Saunders N, et al. Contamination in smooth gel breast implant placement: testing a funnel versus digital insertion technique in a cadaver model. Aesthet Surg J 2012;32:194-9.


3. Jones P, Mempin M, Hu H, et al. The functional influence of breast implant outer shell morphology on bacterial attachment and growth. Plast Reconstr Surg 2018;142:837-49.


4. Flugstad NA, Pozner JN, Baxter RA, et al. Does implant insertion with a funnel decrease capsular contracture? A preliminary report. Aesthet Surg J 2016;36:550-6.



5. Montemurro P, Fischer S, Schyllander S, et al. Implant insertion time and incision length in breast augmentation surgery with the Keller Funnel: results from a comparative study. Aesthetic Plast Surg 2019;43:881-9.



6. Galimberti V, Vicini E, Corso G, et al. Nipple-sparing and skin-sparing mastectomy: review of aims, oncological safety and contraindications. Breast 2017;34 Suppl 1:S82-4.


7. Lin KY, Blechman AB, Brenin DR. Implant-based, two-stage breast reconstruction in the setting of radiation injury: an outcome study. Plast Reconstr Surg 2012;129:817-23.


8. Burkhardt BR, Fried M, Schnur PL, et al. Capsules, infection, and intraluminal antibiotics. Plast Reconstr Surg 1981;68:43-9.


9. Chopra K, Gowda AU, McNichols CHL, et al. Antimicrobial prophylaxis practice patterns in breast augmentation: a national survey of current practice. Ann Plast Surg 2017;78:629-32.


10. Hammond DC, Canady JW, Love TR, et al. Mentor Contour Profile Gel implants: clinical outcomes at 10 years. Plast Reconstr Surg 2017;140:1142-50.


11. Sbitany H, Wang F, Peled AW, et al. Immediate implant-based breast reconstruction following total skin-sparing mastectomy: defining the risk of preoperative and postoperative radiation therapy for surgical outcomes. Plast Reconstr Surg 2014;134:396-404.


12. de Araujo TB, Jue Xu M, Susarla SM, et al. Impact of prior unilateral chest wall radiotherapy on outcomes in bilateral breast reconstruction. Plast Reconstr Surg 2016;138:575e-580e.