|
 |
- Search
| Arch Aesthetic Plast Surg > Volume 21(1); 2015 > Article |
Abstract
Although several cases of successful reconstruction of complete nasal amputations have been reported, reconstruction of a traumatic amputated nose remains a challenge both aesthetically and functionally. Even if replantation of the nasal tip is successful, the scar on the nose may develop an irregular appearance, an ill-fitting contour, a trap door deformity, or discoloration. In the predominant nasal tip, these suboptimal results are very stressful for patient. There are no guidelines for both management and postoperative care of traumatic nasal amputation. At the completion of laser scar revision after successful replantation, we present an excellent aesthetic outcome using the 1,550-nm fractional erbiumŌĆōglass laser (MOSAIC┬«, Lutronic Co. Ltd, Seoul, Korea). Based on our experience, a microvascular replantation followed by fractional non-ablative laser therapy was not harmful and was available to maximize the aesthetic outcomes.
Because the nose is one of the most prominent and characteristic features of a face, its successful replantation or replacement of the amputated nasal segment has been a challenging management problem [1-3]. Recently, although several cases of successful microsurgical replantation of an amputated nose have been reported, it still poses significant difficulty from technical and management perspectives. Several factors, such as initial trauma of amputation tissue, medical leech bite wound, infection, arterial insufficiency, or venous congestion induce the marginal or focal skin defect. In the wound healing process, these wounds would be healed with contracted and notable scars. However, scar management for the replanted nose may be out of interest, so far.
There are surgical and non-surgical options for management of scars [4]. In the replanted nasal tip, due to hemodynamically unstable tissue and risk of unpredictable outcome, there is hesitation to perform surgical scar revision. It is not clear which option for scar management is the best choice since facial tissue replantation was successful.
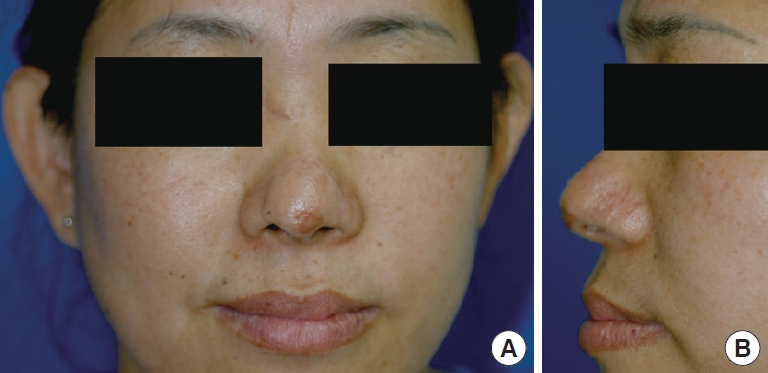
A 41-year-old female presented with a complete amputation of the nasal tip and nasal bone fracture caused by a thick piece of broken glass. The amputated nasal tip segment measured 3.5├Ś2.5├Ś1.0 cm in size, including a distal portion of the greater alar cartilage (Fig. 1). There was a split-thickness skin defect on the distal part of the amputated nasal tip (Fig. 1C). First, nasal bone reduction was performed and two separate lateral nasal branches of a facial artery, with a diameter of 0.2 and 0.3 mm, two columellar arteries with diameters of 0.3 and 0.4 mm, and two subcutaneous veins with a diameter of 0.5 mm were identified. An end-to-end microvascular anastomosis of all four vessels (two lateral nasal branches of the facial artery and two subcutaneous veins) was performed using 11-0 nylon. Anastomosis of the columellar arteries could not be performed due to positional difficulty and the relatively dense surrounding connective tissues limiting the space for microsurgical anastomosis. Once capillary refilling of the replanted nasal tip was confirmed, the cartilage was approximated with 5-0 and 6-0 PDS sutures, and the skin was closed using 6-0 nylon.
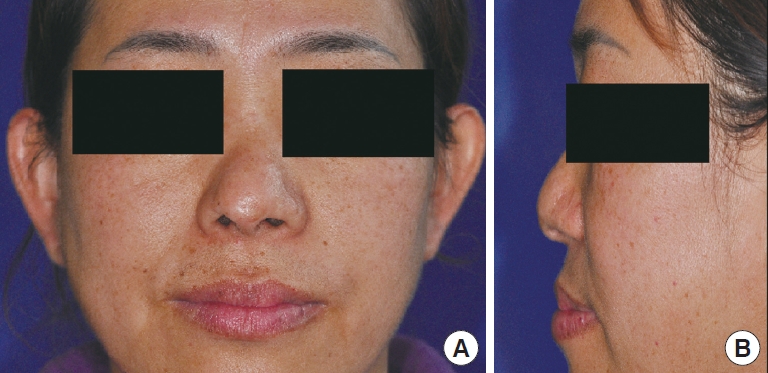
Three medical leeches were used for venous congestion occurred in the replanted nasal segment in the replanted nasal segment for two days. The amputated nasal tip segment survived with a tiny skin defect (Fig. 2).
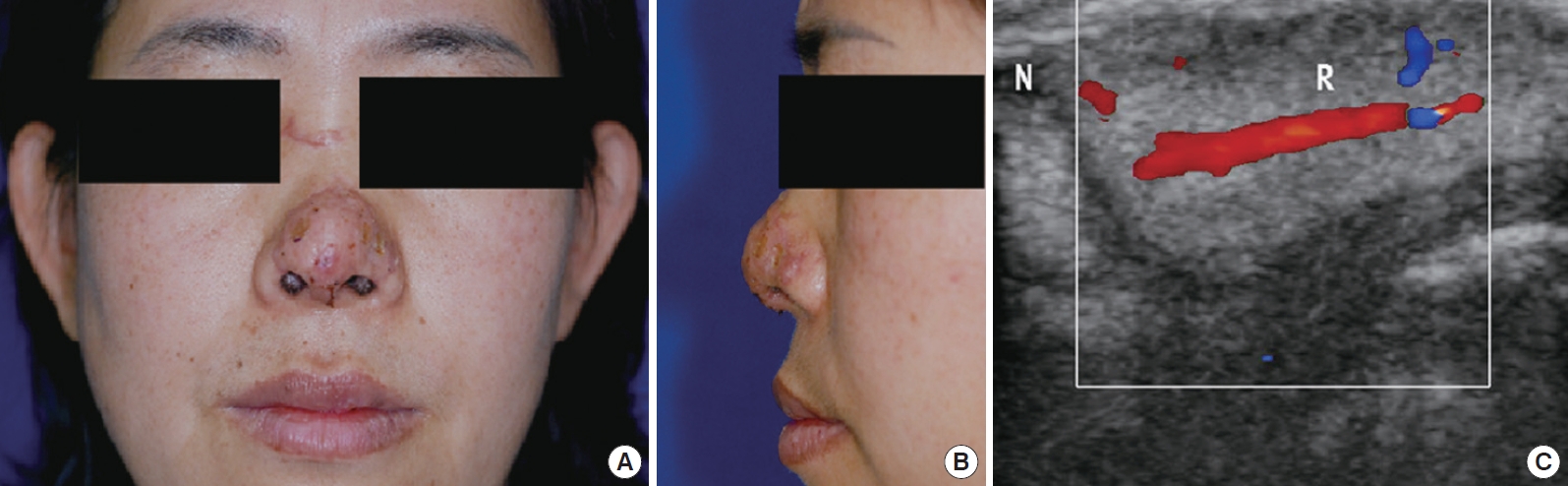
The first scar treatment was performed after postoperative 2 months with a 1,550-nm fractional erbiumŌĆōglass laser (MOSAIC┬«, Lutronic Co. Ltd, Seoul, Korea) and contratubex┬«, but we lost patient follow-up. After nine months, the patient came back to our clinic for improvement of the nasal scar. For treatment of the postoperative scar and the skin graft contracture left at the replanted sites (Fig. 3), same fractional erbiumŌĆōglass laser was used following the nine-month period after surgery. The nose was taken at a pulse energy of 17 to 20 mJ at 125 microthermal zones (MTZ)/cm2 to a final density of 750 (MTZ)/cm2. The patient had received six treatments with three-week intervals in between treatments for the total of 18-week periods. At the completion of fractional laser therapy, no sign of postoperative wounding, erythema, hypopigmentation, infection, hyperpigmentation, or additional scarring was observed (Fig. 4).
Recently, despite technical difficulties in anastomosis of small-sized vessels, several cases of successful microsurgical replantation of an amputated nose have been reported and they proved to be far superior to the conventional composite graft [1-3].
Even if replantation is successful, because the nose is the most critical aesthetic subunit of the face, the need for successful management of the postsurgical scar could never be over-emphasized. The unwanted postoperative scar could have a devastating impact from the psychosocial perspective [5].
Scar management methods, including surgical revision, ablative laser treatment, non-ablative fractional laser, dermabrasion, and intralesional steroid injection were discussed. The patient declined the other methods because of risk of infection, further scaring, hypopigmentation, hyperpigmentation, and anxiety of nose necrosis. Non-ablative fractional laser was chosen because of its safety benefit and easily controlled method compared to other methods [6,7].
Fractional photothermolysis (FPT; Fraxel SR laser) using the 1,550-nm nonablative wavelength has a variety of clinical applications, including pigmented lesions, periorbital rhytides, skin resurfacing, melasma, actinic keratosis, and surgical scars [8]. Microscopic laser columns penetrate deep into sub layers of skin to create multiple evenly-spaced microthermal zones of injury. Within these damaged areas, localized epidermal necrosis and collagen denaturation occur, followed by an expulsion of epidermal debris and neocollagenesis, while the nonablative areas serve as the epithelial bridge to expedite the remodeling process with tighter, fresher, and more youthful-looking skin [8].
Probably due to the rarity of complete nasal amputations in clinical practice, there are no guidelines for both management and postoperative care of traumatic nasal amputation. Based on our experience, as far as we can judge, fractional laser treatment is safe after 2 months nasal replantation. But, it is not sure because we lost the patient follow-up after 1st fractional laser treatment. Although additional cases with a longer follow-up term will be necessary, a microvascular replantation followed by fractional non-ablative laser therapy was not harmful and was available to maximize the aesthetic outcomes.
Fig.┬Ā1.
Preoperative views. (A) Anterior view of the patient. (B) Lateral view of the patient. (C) Anterior surface of the amputated nasal segment. (D) Posterior surface of the amputated nasal segment showing two lateral nasal arteries (A1, A2), two columellar arteries (A3, A4), and two subcutaneous veins (V1, V2).
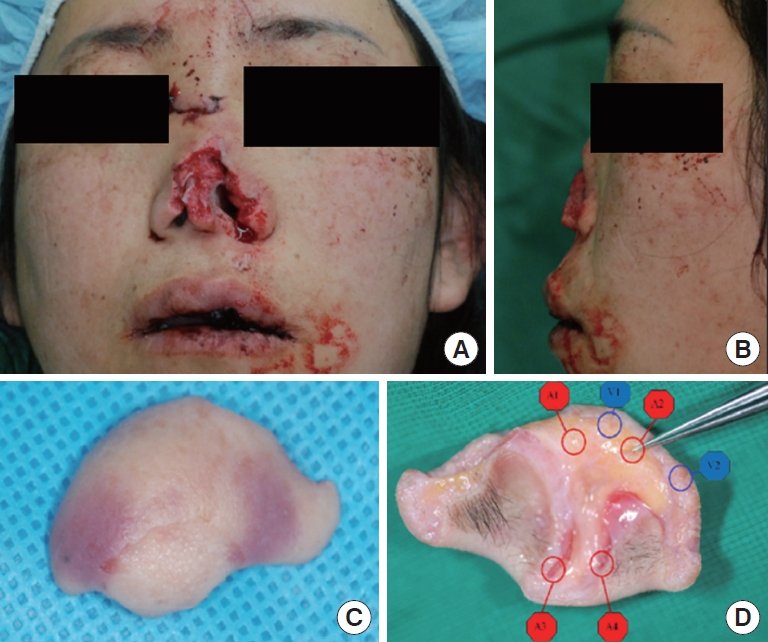
Fig.┬Ā2.
Postoperative view of the nose at Postoperative week 3. (A) Anterior view of the patient. (B) Lateral view of the patient. (C) Color Doppler of anastomosed artery and veins.
REFERENCES
1. Niazi Z, Lee TC, Eadie P, et al. Successful replantation of nose by microsurgical technique, and review of literature. Br J Plast Surg 1990;43:617-20.


2. Aky├╝rek M, Safak T, Ke├¦ik A. Microsurgical revascularization of almost totally amputated alar wing of the nose. Ann Plast Surg 2004;53:181-4.


3. Kim S, Jeong H, Choi TH, et al. Successful re-plantation of an amputated nasal segment by supermicrosurgery: a case report and review of the literature. J Plast Reconstr Aesthet Surg 2010;63:e380-3.


4. Robinson JK, Hanke CW, Sengelmann RD, et al. Surgery of the skin: procedural dermatology. St. Louis, MO: Mosby Inc; 2005.
5. Cantarella G, Mazzola RF, Pagani D. The fate of an amputated nose after replantation. Am J Otolaryngol 2005;26:344-7.


6. Pham AM, Greene RM, Woolery-Lloyd H, et al. 1550-nm nonablative laser resurfacing for facial surgical scars. Arch Facial Plast Surg 2011;13:203-10.


-
METRICS

-
- 0 Crossref
- 3,314 View
- 36 Download
- Related articles in AAPS
-
Actinomycosis in a Mucosal Lesion on a Created Perioral Dimple: A Case Report.2017 October;23(3)