Local Flap Surgical Scar Management Caused by Skin Cancer Using Fractional CO2 Laser Treatment
Article information
Abstract
Background
Despite careful and atraumatic surgical techniques, surgical treatment and reconstruction can result in scarring. Scar from skin cancer on the face may continue for a long time. This current report demonstrates the utility of a fractional CO2 laser to treat facial scar resulting from local flap coverage to remove skin cancer.
Methods
Five patients underwent local flap coverage after removing facial skin cancer tumors. The resulting scars after reconstruction of these skin cancer defects are on face. Each received 6 treatments with a fractional CO2 laser device (LineXel®; UTI Co. Ltd, Seoul, Korea). Treatments were spaced about 1 month apart. Results were evaluated before the initial treatment, and at 1 month after the last treatment session.
Results
The fractional CO2 laser device is effective for treating surgical scars especially on scar texture and thickness without significant adverse effects. Prior to the laser session, these scars concerned different pigmentation, pliability, height, vascularity compared to the surrounding skin. Patients also expressed a 4-point subjective scale of satisfaction. Patients were satisfied with the treated scars.
Conclusions
The fractional CO2 laser device of the present report is an effective treatment modality for facial scars after reconstruction of skin cancer defects. Besides this laser also does not show any serious adverse effect.
INTRODUCTION
Despite the improvements in treating scars, surgical scar management has given major challenges. In some cases, facial scars are suitable to revise by surgical management. But in most cases, the favorable outcome for improving scar texture can be obtained by facial resurfacing. Fractional photodermolysis introduced in 2004 to set a matrix of energy beams to form an array of microscopic thermal wounds and to provoke a therapeutic response in the dermis [1]. Non-ablative fractional photothermolysis at wave lengths of 1,550 and 1,540 nm has been thought to be effective for scar treatment, but fractional ablative laser has been prevalent in the last years because of its potentially more efficacy in the treatment of both the dermal and epidermal components of scar tissue [2-7]. The fractional ablative laser has been a useful strategy for the treatment of scars [8]. This present study was designed to evaluate the safety and efficacy of treatment with ablative CO2 fractional laser for facial scar resulting from local flap coverage to remove skin cancer.
METHODS
We performed a retrospective study on the postoperative scars of five patients (3 men, 2 women) of ages from 49 to 74 (average age, 59.4 years) who underwent local flap coverage after removing facial skin cancer tumors. We have recruited the patient for studying November 2011 to November 2014 (Table 1). The anatomic distribution of scars was completely on the face. In our study, Exclusion criteria were a history of keloid scarring, isotretinoin use, infection of the postoperative scar, and oral anticoagulant use. Each patient provided signed informed consent to treatment and use of their photographs for scientific and teaching purposes
The resulting scars after reconstruction of these skin cancer defects are on the upper lip (Case 1), philtral area (Case 2), left lower eyelid (Case 3, Case 5) and nose. When the wounds were completely healed and 1 month had passed, the resulting surgical scars each received 6 treatments with a fractional CO2 laser device (LineXel®; UTI Co. Ltd, Seoul, Korea). Treatments were spaced about 1 month apart. Topical anesthetic cream (eutectic mixture of 2.5% lidocaine hydrochloric acid and 2.5% prilocaine; EMLA cream, AstraZeneca AB, Södertälje, Sweden) applied 1 hour before treatment to reduce patient discomfort during the procedure. The laser treatment was performed with a pulse duration of 200–340 milliseconds and a distance of 0.8–0.9 mm. Around periorbital area, an eye protector is given to the patient. After treatment, the treated areas were cooled with ice packs for 5 to 10 minutes to remove heatness and relieve pain. To make complete epithelization, a moisturizer and antibiotics oint were applied for 1 week and the a sunblock was applied throughout all these treatment period.
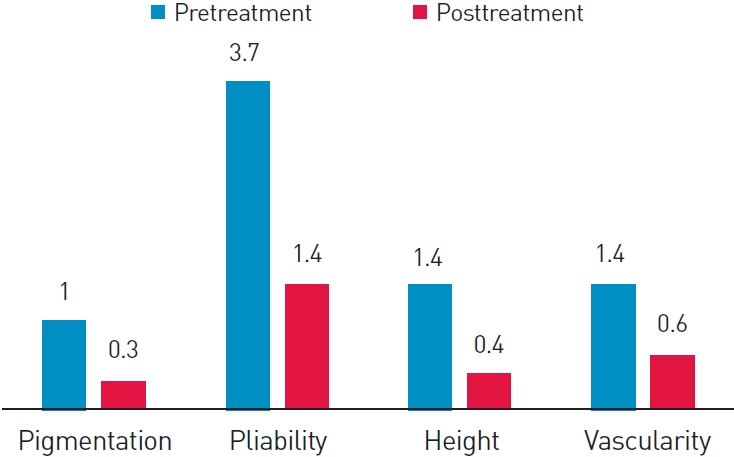
Photographs were obtained using identical camera setting, lighting and patient positioning at baseline, every treatment session and 1 month after the last session. The experienced 2 independent physicians made objective assessments using the Vancouver scar scale (VSS), which includes pigmentation (0=normal, 1=hypopigmented, 2 =mixed pigmentation, 3 =hyperpigmented), pliability (0 = normal, 1=supple, 2=yielding, 3=firm, 4=ropes, 5=contracture), height (0=flat, 1–2 mm, 2=2–5 mm, 3–5 mm), and vascularity (0=normal, 1=pink, 2=red, 3=purple). In evaluation of pliability and height scores based on clinical photos in diverse angle of camera (Standard 5 views) and medical records. One months after the last treatment, patients were asked to estimate their overall satisfaction using a grading scale (excellent, good, fair, poor). Patients were also questioned about side effects of the treatment.
We compared patient satisfaction degrees using VSS, and adverse events using a Wilcoxon signed-rank test with SPSS version 17.0 (SPSS Inc., Chicago, IL, USA). Differences were considered statistically significant when P<0.05.
RESULTS
Mean VSS scores for the treated scars were 7.5 (standard deviation [SD] 1.70) before treatment, 2.7 (SD 0.57) six months after treatment. The mean improvement of VSS score was 4.8, which was evaluated by 2 experienced physicians (P<0.05) (Table 1). The surgical scar was significantly improved by fractional CO2 laser treatment during the followed period (Fig. 1). There was significant improvement in scar quality after treatment (Fig. 2-4) The patient’s overall satisfaction using a grading scale was also significantly high with the their treated scar. Three of the 5 patients (60%) were excellent, 2 (40%) were good with the results.
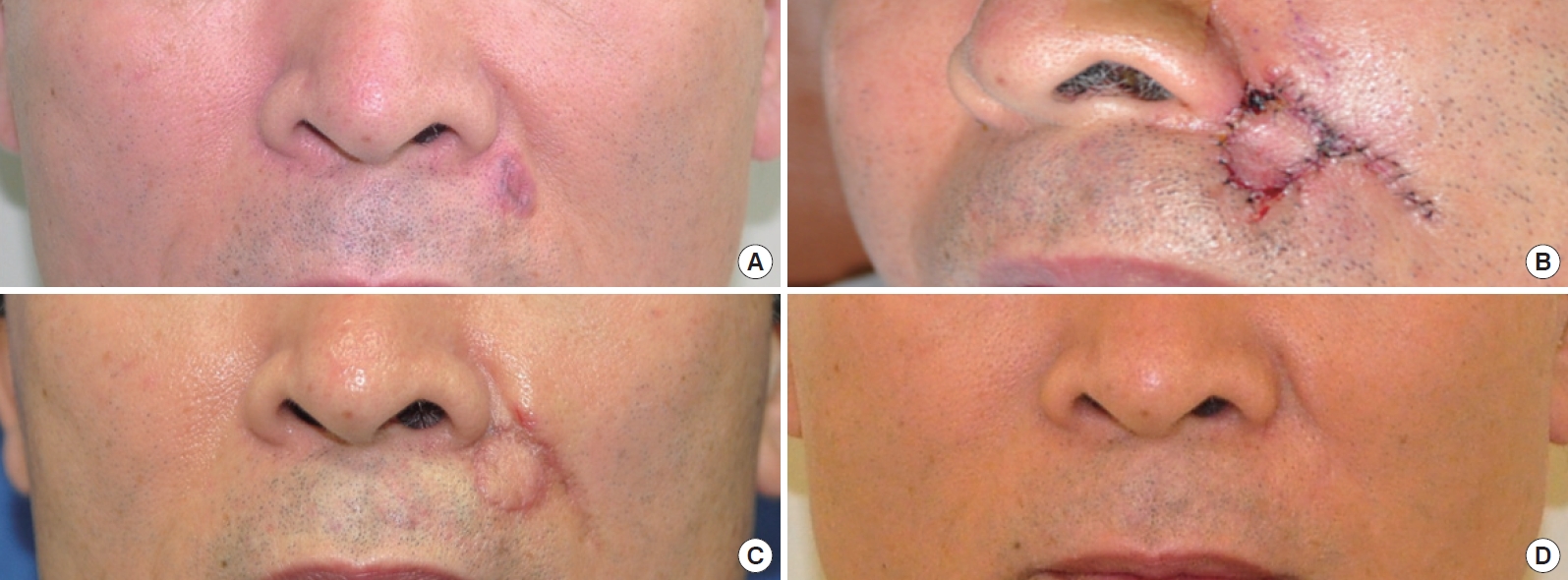
54 year-old male. (A) Preoperative. (B) Postoperative delirium (POD) #2. (C) 1 month post-surgery but prior to first laser treatment. (D) 4 months after the last fractional CO2 laser treatments, showing nearly complete resolution and blending of the scar line with the surrounding skin.
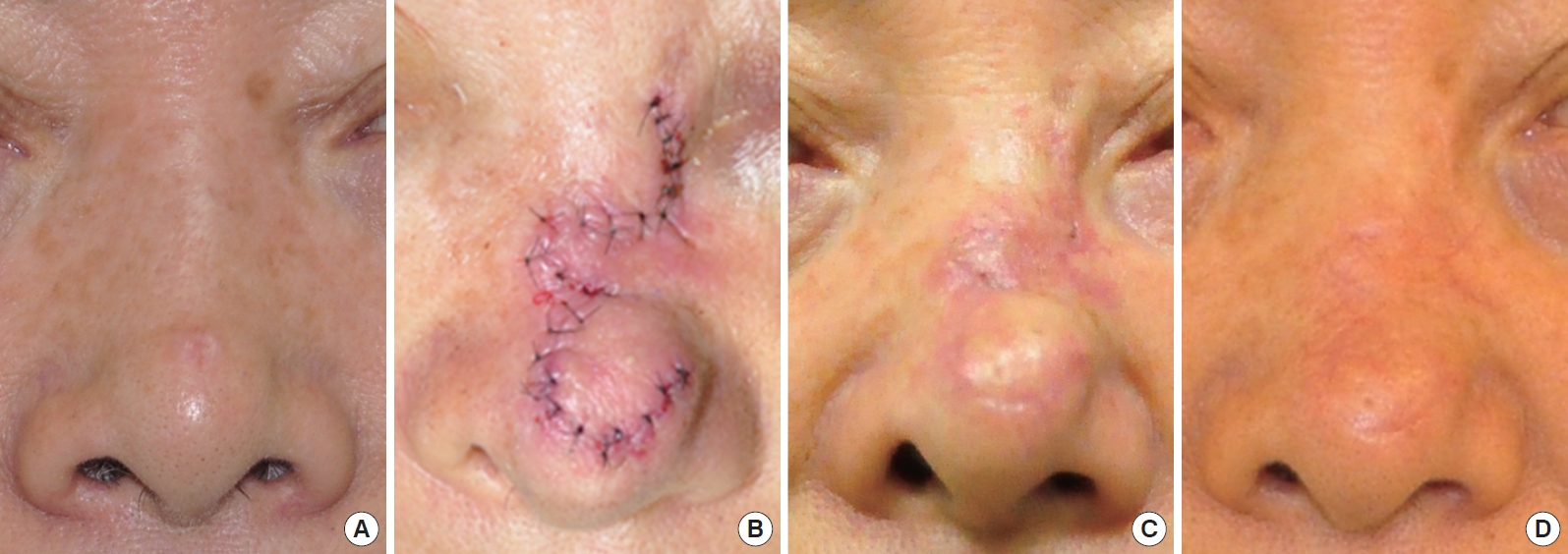
Seventy-three-year-old male. (A) Preoperative. (B) 1 day after a local bilobed flap coverage repair. (C) 1 month after surgery (prior to first laser treatment). (D) 1 month after the third fractional CO2 laser treatments (approximately 4 months after the original surgery).
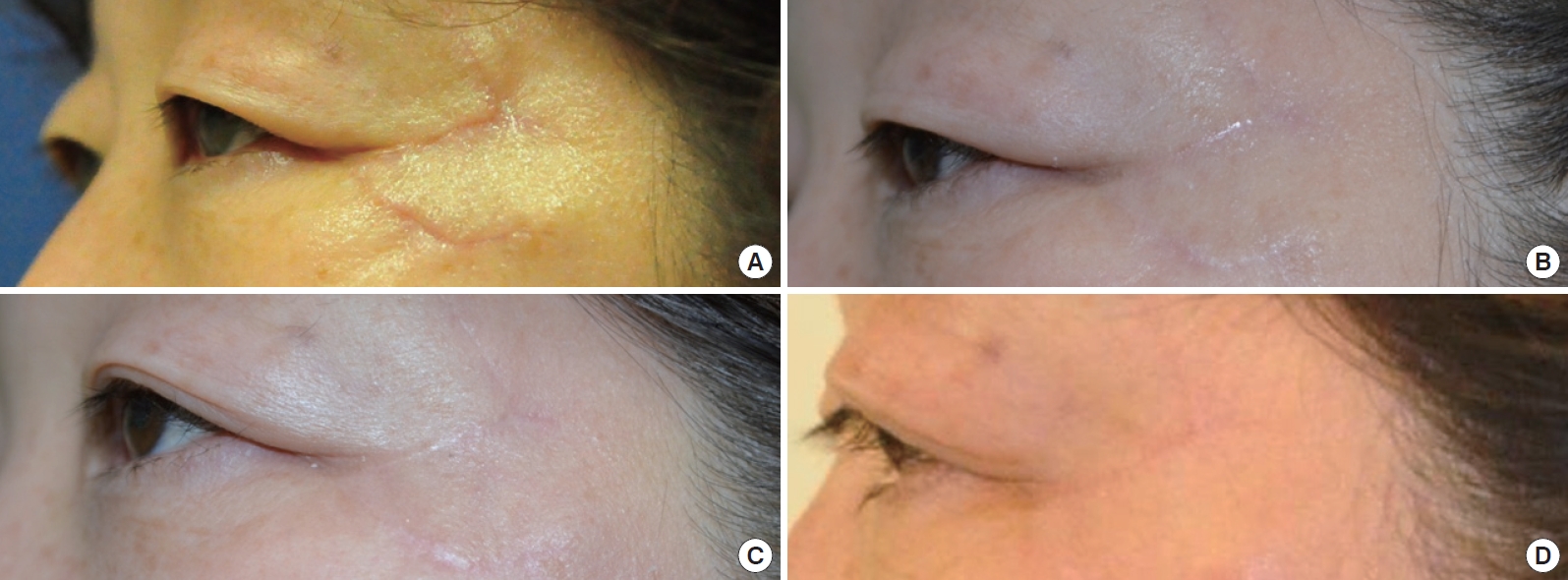
Forty-eight-year-old female underwent local transposition flap. She have taken fractional CO2 laser treatment. (A) Before first laser treatment. (B) 1 month after first laser treatment. (C) 1 month after second laser treatment. (D) 1 month after third laser treatment.
The average of time to reepithelization of epithelial cell was 7 days. After fractional CO2 laser treatment, minor complications, such as pain, erythema, scaling, have remained for 3 days up to 2 weeks. Any serious adverse effects, such as wound disruption, postinflammatory hyperpigmentation, or dyspigmentation, were not shown in this study. And The laser treatment we used is relatively easy to use and apply any facial scar regardless of an aesthetic unit or relaxed skin tension line.
DISCUSSION
Ablative lasers including CO2 and erbium (Er):YAG lasers used for scar management can significantly improve the characteristics of scars. Some adverse effects limit their use, so nonablative lasers have become as a safer alternative therapy, but treatment outcomes are unsatisfactory. Recently, ablative CO2 fractional lasers have become more popular. because of their high pulses of energy, this approach results in minor adverse effects and keeps the epidermal architecture surrounding each coagulated, microtreated area intact. Although the mechanism has not clearly explained until now, some authors have hypothesized about how the laser affects the scar remodeling phase after trauma or surgery. One hypothesis concerns thermal injury to the dermis (during which disulfide bond disruption occurs due to tissue heating) where neocollagenesis and remodeling transpire [9]. Another hypothesis focuses on the stimulation of growth factors and cytokines by lasers [3], or the initiation of collagen signaling cascades [10]. Laser-induced hypoxia may also play a role in treatment effects [11].
Ablative fractional resurfacing (AFR) with 10,600 nm CO2 lasers uses fractionated laser beams to generate an array of microscopic columns of controlled deep dermal tissue volumetric ablation and vaporization surrounded by thermally induced annular coagulation zones of denatured collagen with interspersed regions of untreated tissue [12,13]. Because of the thermal effect of ablative CO2 laser, fractional CO2 lasers can gain most of the powerful collagen remodeling capability of traditional CO2 laser resurfacing and decrease the possibility of the adverse effects at the same time.
The timing of initiation of laser treatment, we chose, was 4 weeks after local flap surgery. Because there are some literatures which recommend early laser treatment after surgery. Jung et al. [9] studied the timing of initiation of fractional CO2 laser in thyroidectomy scars. They thought re-epithelization would be complete within 2 to 3 weeks after surgery. Hong et al. [14] treated scars using fractional CO2 laser 4 weeks after revision surgery. They suggested the early laser treatment can minimize undesirable cosmetic results, such as hypertrophy, increased erythema, and hardened/contracted scars.
We evaluated the state of pigmentation, vascularity, pliability, and thickness. The fractional CO2 laser made an improvement in pliability and thickness than in vascularity and pigmentation. It is suggested that the fractional CO2 laser is effective for treating surgical scars in the facial area in the postoperative period, especially on scar texture and thickness. Treatment using fractional CO2 laser may provide scars to improve rapidly and may prevent scar formation. The laser abrasion may help scars to flatten the irregular surface of surgical scars and flatten the margin between scars and adjacent tissue to make properties of scar margin look similar. The shrinkage of a scar tissue makes scar size smaller. The arrange of collagen of regenerated tissue is regular, which may have an effect on improvement of scar texture and scar pliability without any serious adverse effects. The fractional CO2 laser device successfully blurred scar texture and surface irregularity with that of the surrounding skin by clearing pigmentary abnormalities and telangiectasis as well as improving the scar line.
In our research, most of patients received post-treatment care well and the adverse effects such as pain, erythema, scaling, have remained for 3 days up to 2 weeks. Any serious adverse effects, such as wound disruption, postinflammatory hyperpigmentation, or dyspigmentation, were not shown in this study.
The limitations of this study include the lack of comparison with the control group. A split-scar study could help understand the effects of fractional CO2 laser treatment more precisely. Second, the number of patients is relatively small. In large population in study, it could help to evaluate the result more accurately and to describe the effect of laser treatment would be varied according to age, scar site and local flap method. Last, the term of study is relatively short. Longer-term follow-up is needed to evaluate the course of treated scars.
These encouraging results suggest that scars resulting from skin cancer surgery can be treated safely and effectively with fractionated CO2 laser technology.
CONCLUSION
The CO2 laser device of the present study is effective modality to improve facial scars resulting from skin cancer surgery. This laser also does not show any serious adverse effect. But we have to take care of occurring erythema and post inflammatory hyperpigmentation (PIH) after the treatment. In our research, even Fitzpatrick classification skin type III-IV, common in Korean, also shows satisfying results and the cautious posttreatement care help results not to remain severe adverse effects. Almost skin cancer develops at facial area, and it also can be surgically excised totally and completely cured. In case of middle-aged patient, the posoperative scar can make some troubles in social life. So using laser to minimize surgical scars makes it possible to achieve more ideal treatment when treating skin cancer which can be totally excied in middle-aged patient.
Acknowledgements
This work was supported by the Soonchunhyang University Research Fund.
Notes
No potential conflict of interest relevant to this article was reported.