|
 |
- Search
| Arch Aesthetic Plast Surg > Volume 20(3); 2014 > Article |
This article has been corrected. See Arch Aesthetic Plast Surg. 2015 Jun 30; 21(2): 85.
This article has been corrected. See Arch Aesthetic Plast Surg. 2015 Feb 28; 21(1): 30.
This article has been corrected. See Arch Aesthetic Plast Surg. 2015 Feb 28; 21(1): 30.
Abstract
Blepharoplasty is one of the most common anti-aging operations. Although rare, complications such as ectropion may occur. Thus, we introduced an operative technique to prevent ectropion of the lower lid after blepharoplasty. From January 2012 to August 2013, we performed a nonincisional suspension suture (NISS) technique for 30 patients who visited our clinic for lower blepharoplasty. These patients had a distance of greater than 7 mm on the distraction test and were suspected of having horizontal lid laxity. We performed a slit incision 3 mm superior to the junction between the lateral epicanthus and the orbital bone during lower blepharoplasty. We passed a 7-0 nylon suture through the subcutaneous layer and the orbicularis oculi muscle. Then, we punctured the tarsal plate at the lateral limbus and fixed it to the lateral orbital rim by puncturing the periosteum. We tied a suspension knot through the slit incision. Thirty patients had satisfactory results without major complications, such as scleral exposure or ectropion. The NISS technique could be an effective method by which to prevent postoperative ectropion in cases with a mild to moderate degree lower lid laxity. The use of a NISS procedure is also a simple surgical technique, which saves time and is minimally invasive.
Lower eyelid blepharoplasty is frequently performed as a midface anti-aging treatment. With a growing interest in aging, the frequency of this type of surgery has also increased. However, depending on the type and pattern of the lower eyelid, extensive, frequent surgeries may be required [1,2]. In addition, such complications as ectropion or scleral exposure may occur following lower eyelid blepharoplasty or midface lift [3]. Therefore, we performed both snap back and distraction tests prior to performing lower eyelid blepharoplasty to evaluate lower lid tonicity. We attempted to predict patients who were postoperatively vulnerable to ectropion in order to prevent its postoperative occurrence [4,5]. In patients at risk of developing ectropion postoperatively, we attempted to prevent its occurrence using a nonincisional suspension suture (NISS) technique. We applied this method to patients who were at risk of developing ectropion following lower eyelid blepharoplasty, obtaining satisfactory outcomes. Here, we report our treatment outcomes with a review of the literature.
In the current study, we initially evaluated patients who planned to undergo lower eyelid blepharoplasty at our medical institution from January 2012 to August 2013. Of these, 45 patients were considered for inclusion in the current study, including the following cases:
(1) Patients who were suspected of having horizontal lid laxity based on findings that the lower eyelid returned to the eyeball at a lower velocity after undergoing a snap back test
(2) Patients in whom the distance extending from the eyeball to the lid margin was longer than 7 mm when the lower eyelid was pulled by a finger
These patients have a risk of developing ectropion postoperatively [4,5]. We performed lower eyelid blepharoplasty concomitantly with a NISS technique (Fig. 1). Patients were followed up at 1-week intervals for 1 month; after which, patients were followed up for 1 year at 1-month intervals. We finally enrolled a total of 30 patients in the current study, and their mean follow-up period was 7 months. Our clinical series of patients was composed of 12 men and 18 women, whose mean age was 64.5 years (range, 53-76 years). Following the elevation of the musculocutaneous flap during lower eyelid blepharoplasty, a 1-2-mm incision was made 3 mm superior to the junction between the lateral epicantus and the orbital bone. Then, a small window was made (Fig. 2A). Through the incision window, a 24-mm needle and a 7-0 nylon thread were passed into the subcutaneous layer in the anterior and inferior directions to avoid damaging the eyeball (Fig. 2B). Through the orbicularis oculi muscle, the needle was rotated at an angle of 180° and was passed into the tarsal plate at the lateral limbus (Fig. 2C and D). The needle was then passed into the periosteum of the lateral orbital rim and exited from the incision window via the subcutaneous layer (Fig. 2E). After obtaining posterosuperior traction, we tied a ribbon knot and performed a pinch test. When the tension achieved was such that the lower eyelid was remote from the eyeball at a distance of approximately 3 mm, we tied a knot (Fig. 2F). The same procedure was performed on the contralateral side. After confirming symmetry between the left and right sides, the redundant musculocutaneous flap was excised, and lower eyelid blepharoplasty was completed. The mean surgical time was less than 5 minutes.
A 53-year-old woman visited us complaining of eye bags, a deep lacrimal sulcus, and skin depression (Fig. 3A). During the preoperative snap back test, the patient showed a low velocity in the return of the lower eyelid to the eyeball. Therefore, the patient was suspected to have horizontal lid laxity and thus a high probability of postoperative ectropion. During lower eyelid blepharoplasty, we performed a NISS technique. The patient achieved a tension of the lower eyelid of less than 2 mm on intraoperative or postoperative pinch test. After lower eyelid blepharoplasty, based on the redistribution of fat and skin resection, the patient achieved great improvement in eye bags, the deep lacrimal sulcus, and skin depression. After 6 months, the patient had no findings suggestive of ectropion. In addition, the patient was also satisfied with the cosmetic outcomes (Fig. 3B).
A 62-year-old woman with a past history of lower eyelid blepharoplasty complained of lower eyelid retraction (Fig. 4A). During the distraction test, the distance extending from the eyeball to the lid margin was at least 7 mm (Fig. 4B). Therefore, we planned to perform a suspension suture of the lower eyelid. After elevating the musculocutaneous flap for lower eyelid blepharoplasty, we performed a NISS technique. Then, we performed a distraction test for both eyes, which showed that the margin of the lower eyelid was well attached to the eyeball with moderate tension to the lower eyelid. The patient had an eversion of the temporal portion of the lower eyelid margin, which was resolved over time with posterosuperior fixation using 3M tape. After 1 year, the patient had no findings suggestive of ectropion (Fig. 4C and D). In addition, the patient was also satisfied with the cosmetic outcomes.
There were no findings suggestive of ectropion in most of the 30 patients who were followed up for 1 to 12 months postoperatively. In addition, treatment outcomes were satisfactory in these patients. Regarding complications that occurred during the follow-up period, three patients complained of an unnatural appearance due to bilateral traction when they strongly closed their eyes. Approximately 1 month later, however, most of these symptoms were resolved. Regarding postoperative edema, two patients developed mild eversion of the temporal lid margin or temporal lid bowing. As described here, in patients where the margin of the lower eyelid was slightly detached from the eyeball, there were no further complications with posterosuperior fixation using tape. All symptoms were resolved within 1 week postoperatively.
With the growing interest in aging, lower eyelid blepharoplasty is performed most frequently following upper eyelid blepharoplasty. However, lower eyelid blepharoplasty may cause such complications as ectropion, scleral exposure, cicatrical lower lid retraction, and lagophthalmos. Of these, ectropion may not only lead to functional problems, such as ocular irritation, decreased visual acuity, epiphora, and the frequent use of ocular lubricants, but also to cosmetic problems. These complications thus deserve special attention [3,6].
To preoperatively screen patients who are expected to develop ectropion or scleral exposure, patients may be preoperatively evaluated for horizontal laxity [4,5]. In patients suspected of having horizontal lid laxity by a snap back test, have a distance of greater than 7 mm on a distraction test, and are expected to develop ectropion due to the intraoperative excessive resection of the musculocutaneous flap (although it is impossible to predict the occurrence of ectropion prior to surgery), lateral canthoplasty should be performed [7]. To date, various methods have been proposed for lateral canthoplasty [7-9]. Reech [8] proposed that surgeons perform the Kuhnt-Szymanowski procedure, where the tarsal plate and conjunctiva are directly sutured on a layer-by-layer basis, following the full-thickness excision of the conjunctiva and the tarsal plate in a pentagonal shape at a width of 3-5 mm on the medial side of the lateral canthus, in patients with severe horizontal laxity of the lower eyelid. For the correction of ectropion, Anderson [9] performed the ‘tarsal strip procedure’ by modifying lateral sling canthoplasty. This method is characterized by the removal of the skin and conjunctiva on the lateral side of the eyelid to free a strip of the tarsus. By fixing the tarsal strip to the periosteum of the lateral orbital wall, the appropriate height and tension of the lower eyelid are maintained. These methods have been mainly performed for the correction of ectropion. However, they are time consuming, and technical expertise is essential. Moreover, they require a partial resection of the lower eyelid. There is a possibility that a deformity of the lower eyelid, trichiasis of the lower eyelid, or rounding of the canthus might also occur [10]. Therefore, we need better surgical methods such that surgeons can be satisfied with treatment outcomes from both time and technical perspectives. The NISS technique that we performed at our medical institution can anatomically strengthen the lateral canthal ligament. Moreover, it is also a simpler method and the surgical time is relatively short (~5 minutes), suggesting that it can be used to prevent the occurrence of the ectropion without resecting the lateral canthal tendon during lower eyelid blepharoplasty. In patients with severe horizontal lid laxity or an extended horizontal length, however, surgeons may consider procedures for the excision of the inferior crus of the lateral canthal tendon and the shortening of the horizontal length of the eyelid.
The NISS technique is a relatively simple, less time-consuming modality compared with pre-existing procedures. It is also advantageous in minimizing the occurrence of damage and scars in adjacent tissues, thus lowering the incidence of complications after surgery. Thus, we obtained satisfactory outcomes in preventing the occurrence of ectropion during lower eyelid blepharoplasty.
Fig. 1.
Schematic diagrams: transcutaneous N-I suspension suture (green line). A 7-0 nylon suture is passed through the subcutaneous layer (Subcut. fat) and the orbicularis oculi muscle (Orbicularis m.). The tarsal plate is punctured at the lateral limbus and then inserted through the same route. This procedure is followed by fixation to the lateral orbital rim by puncturing the periosteum.
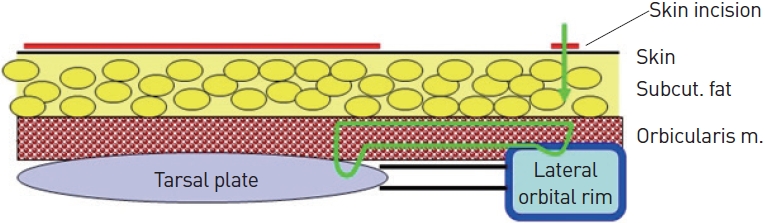
Fig. 2.
Intraoperative findings. (A) A slit incision is made. (B) A 7-0 nylon suture is passed through the subcutaneous layer and the orbicularis oculi muscle. (C) The needle is rotated 180° before puncturing the tarsal plate at the lateral limbus. (D) The tarsal plate is punctured at the lateral limbus and then inserted through the same route. (E) The tarsal plate is fixed to the lateral orbital rim by puncturing the periosteum. (F) A suspension knot is tied through the slit incision window before skin closure, which maintains the tension at a distance of 3 mm from the lower lid margin of the cornea on a pinch test.
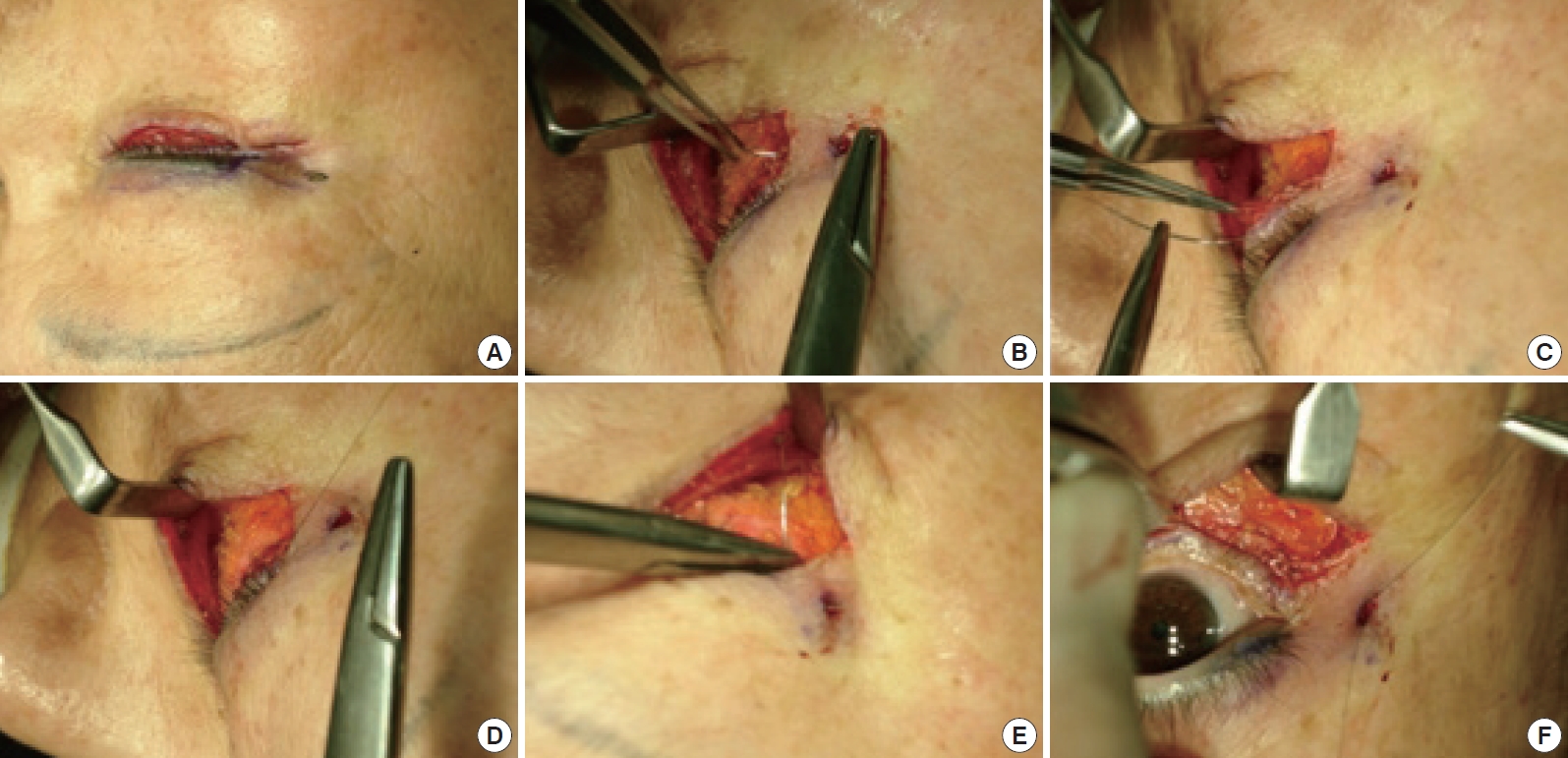
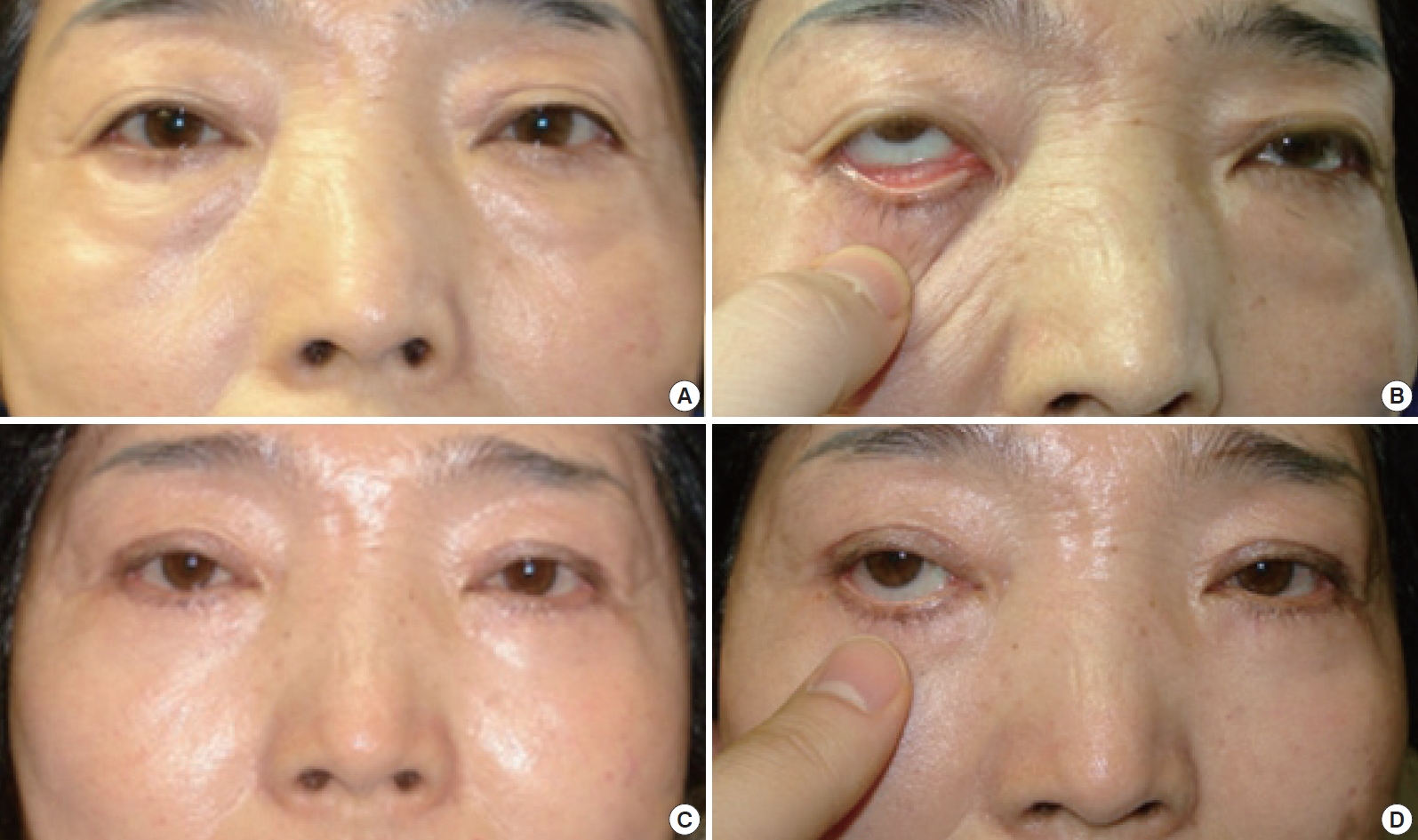
Fig. 3.
Pre- and postoperative clinical photographs. (A) Preoperative photograph shows a 53-year-old woman with lower eyelid bags, accentuation of the tear trough, and increased skin laxity. (B) Postoperative photograph at 6 months showing a lack of ectropion, for which the patient was satisfied with the cosmetic outcomes.

Fig. 4.
Pre- and postoperative clinical photographs. (A) Preoperative photograph showing a 62-year-old woman with a history of the lower eyelid blepharoplasty and lower eyelid involution. (B) Preoperative distraction test shows pulling of the lower eyelid by greater than 7 mm from the eyeball. (C) Postoperative photograph at 1 year showing a lack of ectropion, for which the patient was satisfied with the cosmetic outcomes. (D) Preoperative distraction test shows pulling of the lower eyelid by less than 2 mm from the eyeball.
REFERENCES
1. Hester TR. Subperiosteal malar cheek lift with lower lid blepharoplasty. In: McCord CD, editor. Eyelid surgery. Philadelphia: LippincottRaven; 1955. p. 210-5.
2. Hinderer UT. Vertical preperiosteal rejuvenation of the frame of the eyelids and midface. Plast Reconstr Surg 1999;104:1482-99.


4. Rees TD, LaTrenta GS. Aesthetic plastic surgery. Philadelphia: WB Saunders; 1994.
5. Cho IC. The art of blepharoplasty. Seoul: Koonja; 2013.
6. Lisman RD, Smith B, Bake D, et al. Efficacy of surgical treatment for paralytic ectropion. Ophthalmol 1987;94:671-81.

7. Glat PM, Gelks GW, Jelks EB, et al. Evolution of the lateral canthoplasty: techniques and indications. Plast Reconstr Surg 1997;100:1396-405.


8. Reech ML, Beyer CK, Shannon GM, et al. Practical ophthalmic plastic and reconstructive surgery. Philadelphia: Lea & Febiger; 1976.
-
METRICS

-
- 0 Crossref
- 5,231 View
- 127 Download
- Related articles in AAPS
-
Correction of pseudoptosis occurred after blepharoplasty.2000 September;6(2)