INTRODUCTION
ANATOMICAL BASIS OF ASIAN AESTHETIC OCULOPLASTIC SURGERY
Anatomy and etiology of supratarsal crease
Anatomy and etiology of epicanthal fold
SUPRATRASAL CREASE SURGERY
CREASE CONFIGURATION
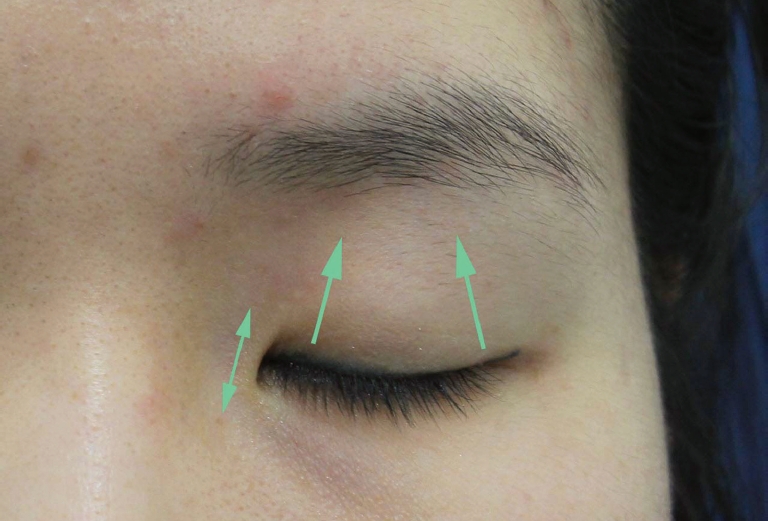
Supratarsal crease placement - Height
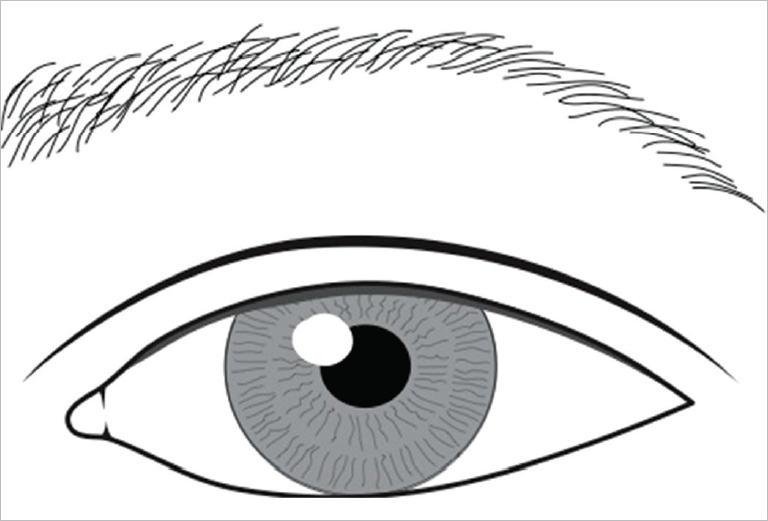
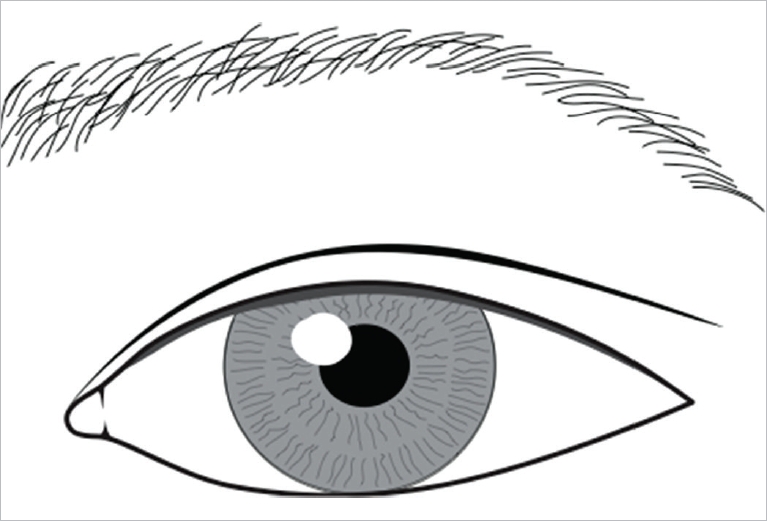
Supratarsal crease configuration - Shape
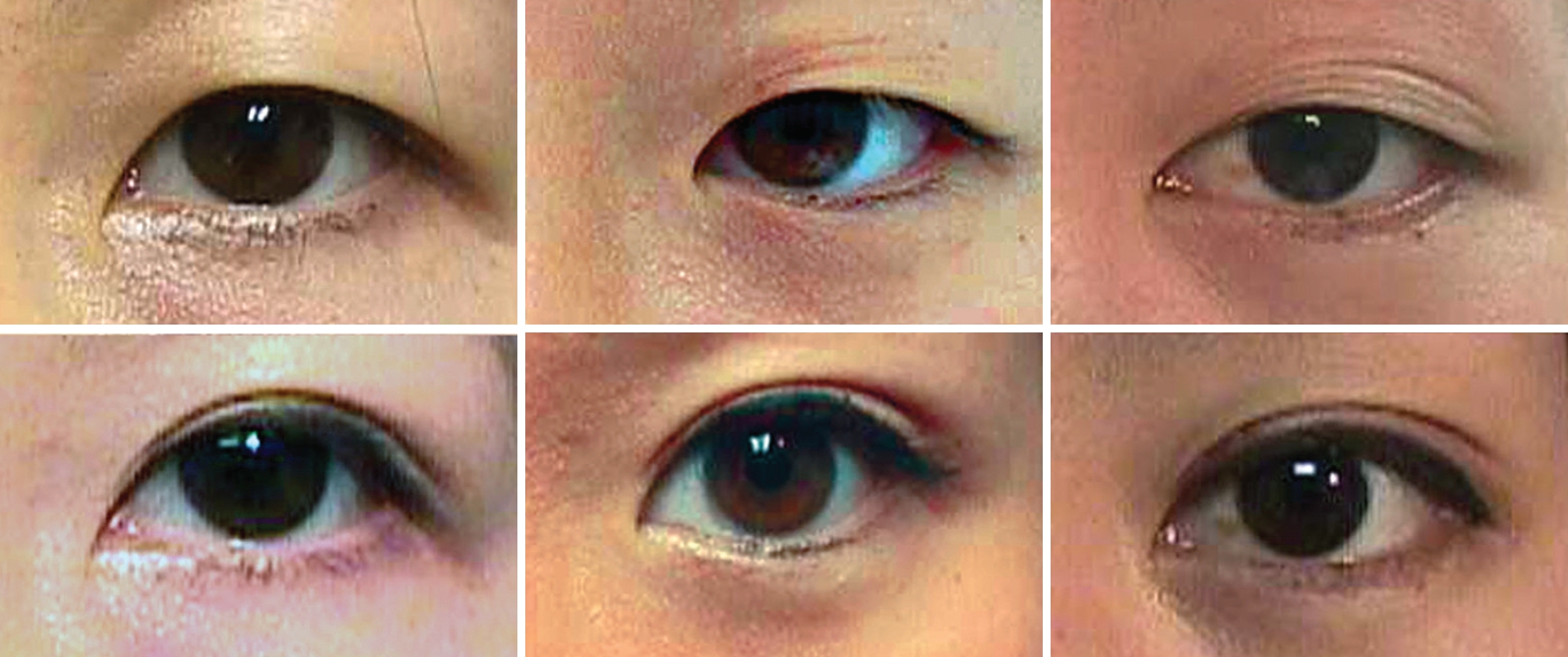
Dynamic crease
Static crease deformity
Aesthetic goals
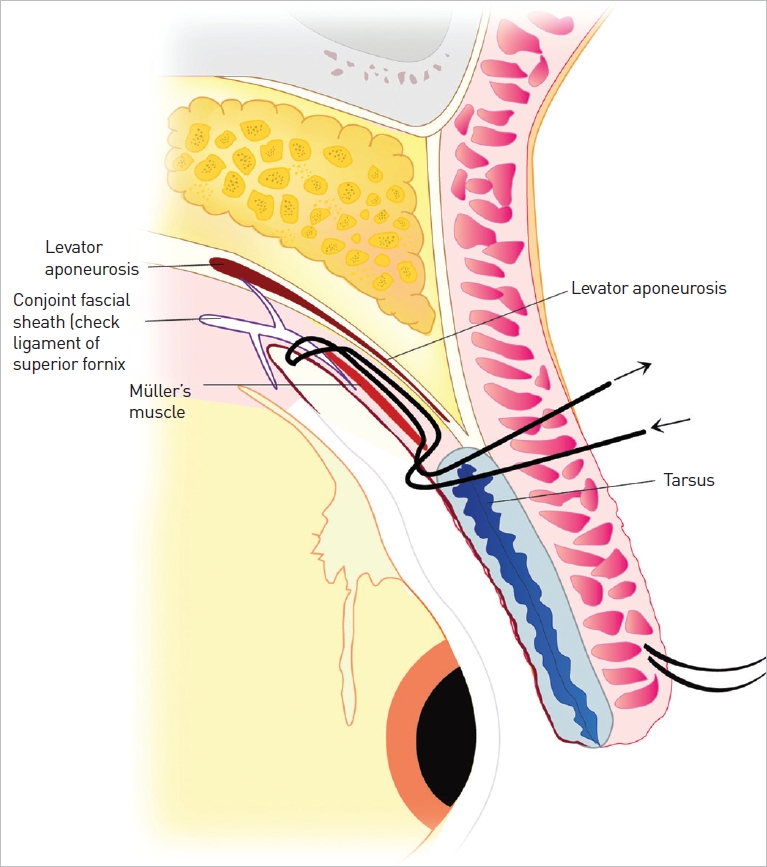
INCISIONAL SUPRATARSAL CREASE SURGICAL TECHNIQUE
Author Chen’s preferred method
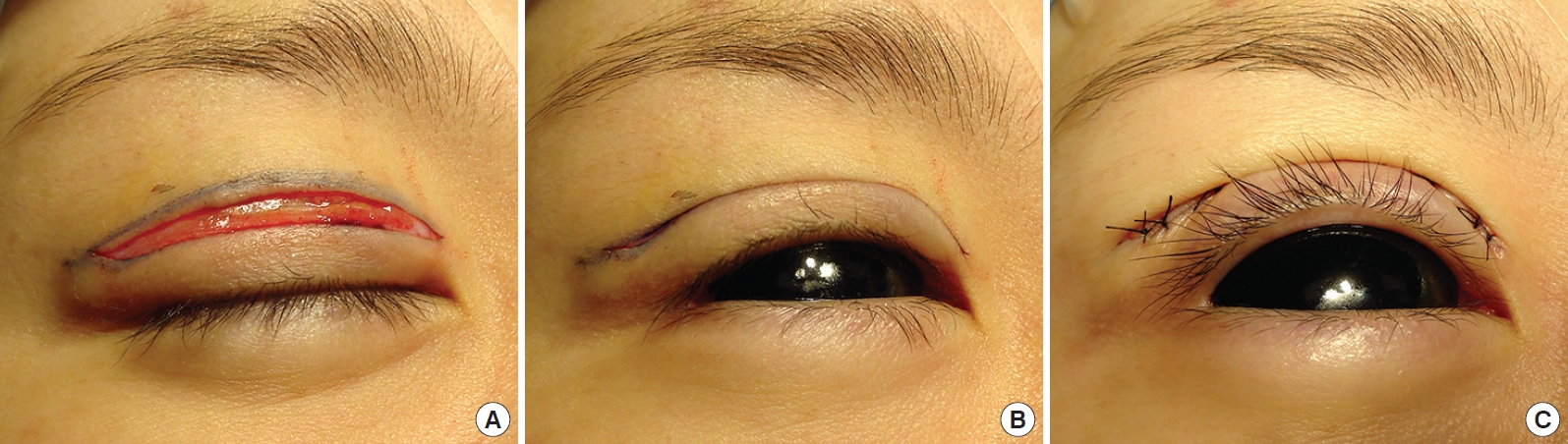
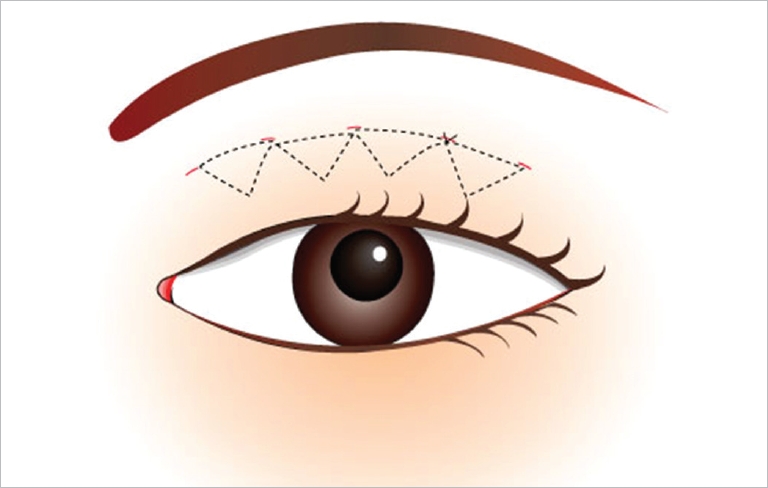
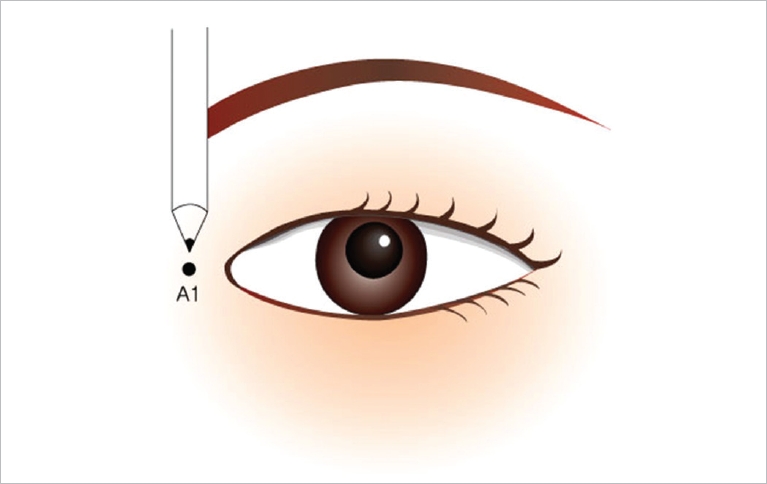
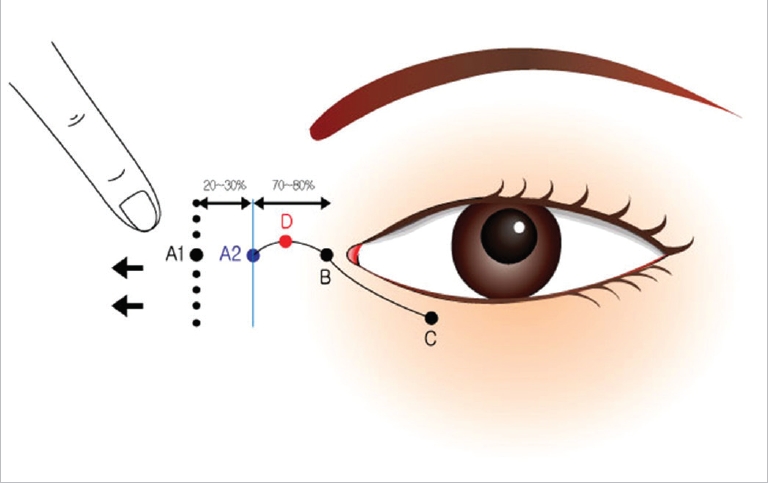
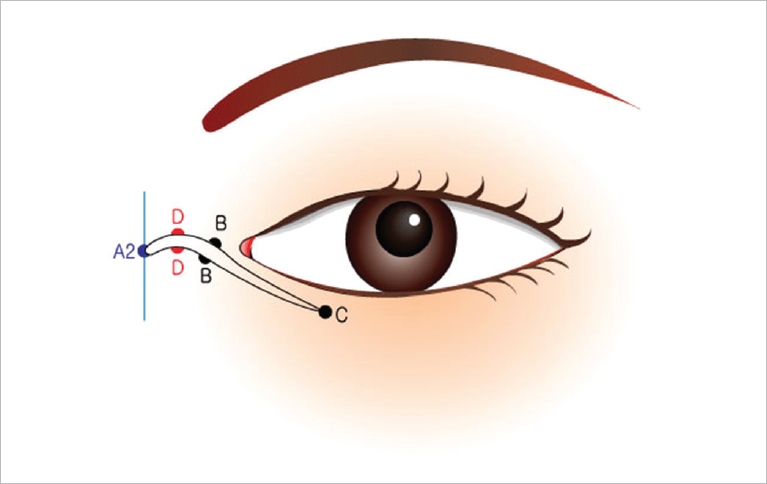
Operative technique – Full incision technique [18,27-31]
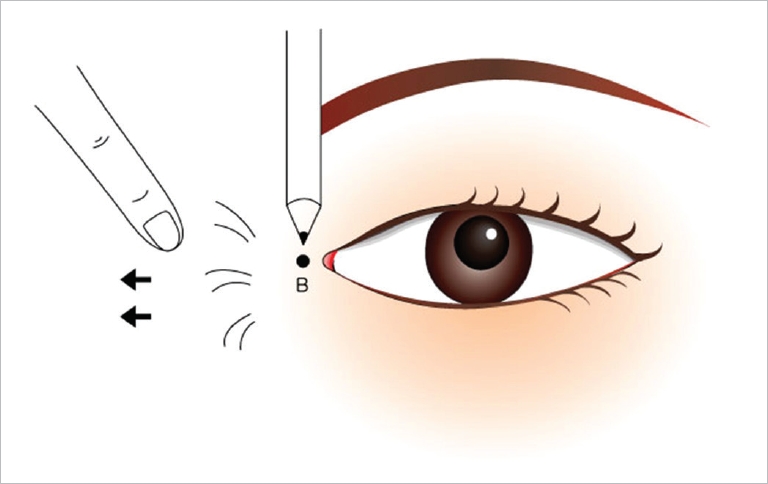
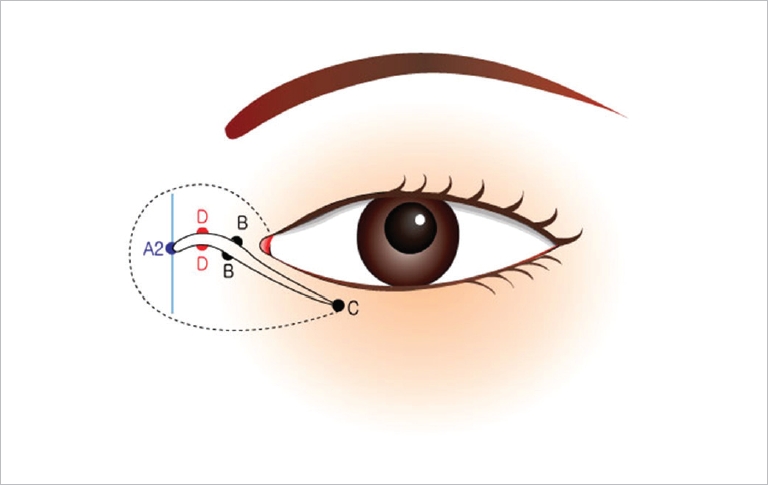
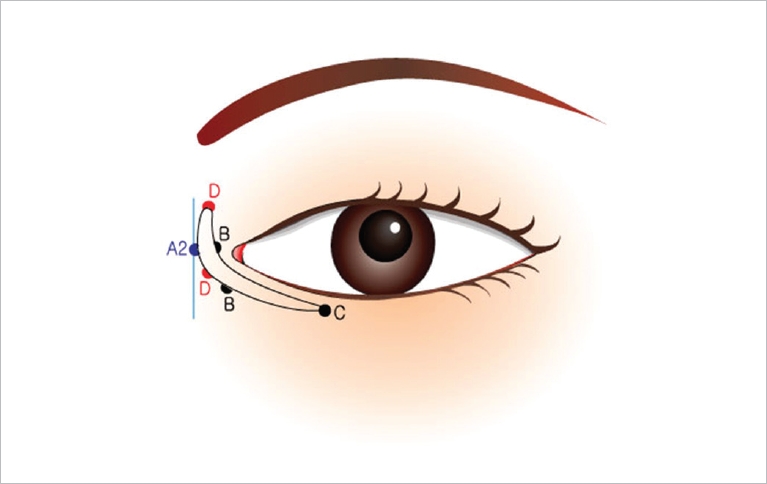
(i) In the design of the nasally-tapered crease, the incision lines are drawn to converge towards the medial canthus as well as the medial fold. To enhance the crease invagination to blend in under the fold, the area is slightly undermined, and excess skin tissue is cut just below the converging crease line (infracrease cut, first snip); the lower edge’s skin is migrated up and a second cut takes care of the small dog-ear. The crease is closed with an interrupted suture placed with the knot on the lower side of the wound edge (infraanchoring of knot,“down-knot” the crease). The goal is to have the nasal-tapering crease indent to beneath (inferior to) the natural residual fold. (Alternatively one may also make the first snip along the crest of the medial canthal fold, and then migrate the lower edge’s excess skin upward to trim it; then infra-anchor its closing knot. It has a slightly higher chance of postoperative induration since the skin along the crest of the medial fold is slightly thicker.)
(ii) With a parallel shape design, after the main steps are carried out and the tissue planes have been reset, the area under the medial fold is slightly undermined. The first relaxing snip near the medial end of the undermined redundant skin is biased towards the lower incision in a slightly oblique fashion (infra-crease cut); the lower edge’s excess skin is migrated upward such that the medial fold is reduced with the second cut removing the dog ear and based along the medial direction of the parallel crease shape. The closure at this end is with a fine interrupted suture tied very lightly and laid on the superior side of the incision (supra-placement of knot without anchoring; “up-knot” the tie loosely, the rationale being that the medial end of a natural parallel crease tends to be shallow). These delicate techniques I used have handled the ethnic non-pathologic medial upper lid fold quite well without the complicated steps usually associated with treatment of epicanthal fold (Epicanthus), which is usually reserved for findings in Down’s syndrome, or patients born with blepharophimosis [32].