 |
 |
- Search
| Arch Aesthetic Plast Surg > Volume 20(1); 2014 > Article |
Abstract
Background
The breast reconstruction using implant has been conducted widely. Many studies were presented to analyze the complications, but most of these studies were conducted with patients relatively short term period follow up. The authors studied with patients who were followed up at least five years.
Methods
Among the patients who were underwent breast reconstruction with implant from 1998 to 2007, 37 patients who met were followed up more than 5 years were selected in the study. Relationships between factors such as the operation methods, volume, type of surfaces of the implants, etc. and the complication rate or reoperation rate were analyzed. The level of satisfactory scoring was measured by patients' and 5 plastic surgeons.
Results
Complications were developed in 21 patients (65.6%) and 9 of them underwent reoperations. Infection was most common cause of complication. Implant removal was conducted to 7 patients, and 5 of them due to infection. The percentages of patients who received postoperative chemotherapy or radiotherapy in complication group and implant removal group were higher than the whole group whereas such correlation was not statistically significant. Direct Implant insertion has 50% of complication and 80% in permanent expander insertion and 73.7% of expanderimplant exchange. The average value of subjective score at last follow up was 4.2 points and the average value of objective score was 5.74.
As incidence rate of breast cancer has recently increased, more attention has been paid to breast reconstruction. The goal of breast reconstruction is to reconstruct breast in proper size, location and shape, symmetry on both sides, and nipple-areolar complex [1].
In general, reconstruction method includes the method that uses autologous tissue such as transverse rectus abdominis myocutaneous flap or latssimus dorsi flap and the method that uses implant or prosthesis.
In case that amount of autologous tissue is insufficient, a patient has experience of receiving surgery on abdomen, or a patient refuses to undergo surgery using autologous tissue, implant is used to perform breast reconstruction.
Breast reconstruction using implant has many strong points such as short time for surgery, relatively low level of technique, low expenses, a few scars that are left behind after surgery, no morbidity such as scar on donor site or hernia, and no risk of flap necrosis or fat necrosis. However, breast reconstruction has some weak points such as high risk of infection, leak or exposure of implant, capsular contracture, and breast shape that looks less natural compared to the case that autologous tissue is used. Therefore, it is necessary to consider both of the strong and weak points before selection of reconstruction method.
However, the reality is that it is difficult to conduct long-term follow-up study on patient group that has undergone breast reconstruction that uses implant. And there are insufficient explanation and understanding on selection of patient and operator when long-term follow-up is performed.
Against this background, the authors conducted the long-term follow-up study for five years or more that targeted 32 patients who received breast reconstruction that used implant in this hospital. They investigated complications of the surgery, patient’s satisfaction, and plastic surgeon’s objective scoring.
This study targeted the patients who were available for the final long-term follow-up that lasted five years or more among the patients who received breast reconstruction that used implant in the period from 1998 to 2007 by one surgeon.
Investigation was conducted for average age of patient group, BMI, additional treatment for cancer or with radiation, and so on. Type of mastectomy and surgical method for implant were generally classified to direct implant, permanent expander and expanderimplant exchange. The preference of surgeon, considering medical history of individual patients, decided type of mastectomy. Surgeon especially considered type of mastectomy in order to choice surgical method for implant. Investigation was conducted also for implant type and surgery time.
In addition, medical records were reviewed to investigate complications and reoperation that was attributable to the complications. As a way to examine patient’s satisfaction, being very unsatisfactory was scored at 2 points while being very satisfactory was scored at 10 points [2]. In objective evaluation of satisfaction with breast shape, the breast shape was scored from 2 points to 10 points by five plastic surgeons with final follow up photographs. When the final follow-up was performed, the authors recorded patient’s willingness to get revision surgery and reason for the surgery.
PASW Statistics 18.0 was used for statistical analysis. The level of statistical significance (P-value) was set at 0.05. For comparison of average in the two groups that consisted of continuous variables, independent sample t-test or Mann Whitney U-test was conducted depending on satisfaction of normality (If normality was satisfied, independent sample t-test was conducted. If not, Mann Whitney U-test was conducted). For analysis of categorical data that consisted of qualitative variables, Chi-square test or Fisher’s exact test was conducted.
When the first surgery for the patient group was performed, 32 patients were targeted. Average age was 45.7 years with average BMI of 25.5 kg/cm2. Average follow-up period was 7.2 years. In regard to location, unilateral cases were found in 29 patients while bilateral cases were found in 3 patients. With respect to mastectomy that was performed in department of surgery, 26 patients had modified radical mastectomy, 1 patient central lumpectomy, 4 patients skin sparing mastectomy, and 2 patients simple mastectomy. The skin incisions and skin flap elevations were conducted with surgical knife, scissors & electrocautery. After the surgery, 17 patients received chemotherapy, 7 patients received radiotherapy, and 23 patients received hormone therapy.
In reference to surgery using implant, 7 patients received direct implant insertion, 5 patients received permanent expander insertion, and 19 patients, which was the highest number, received implant insertion after tissue expansion using expander. Period for replacement of expander and implant was 4.3 months. Saline and smooth surface implant from Mentor® was used mostly for surgery in 23 cases followed by textured surface saline implant, textured silicone implant. Average volume of implant was 296 cc. Implants were inserted under pectoralis major muscle and the pockets were covered with fascia of serratus anterior muscle or serratus anterior muscle, without using acellular dermal matrixes (Table 1).
In the total of 21 cases (65.6%), complications occurred with 9 cases of reoperation. Among various types of complications, infection was found in 12 cases, which was followed by implant rupture and wound disruption (Fig. 1). Infection included skin erythema and using antibiotics. Among the 9 cases of reoperation, 7 cases were implant removal while 2 cases were primary closure due to wound disruption. Among the 7 cases of implant removal, 5 cases were removal due to infection. One case was removal due to implant exposure while one case was removal due to implant rupture. Contracture occurred in 2 cases. Rippling of implant was palpable in 2 cases but was excluded from analysis of complications because such symptom appeared in the initial stage of reconstruction according to the survey for patient so that change was not recognized.
Patients were divided to three groups that included whole group, complication group and implant removal group before risk and correlation were analyzed. Average age and BMI and Diabetes, Hypertension did not show any differences among groups. Each group showed differences between the cases where post-operative chemotherapy was conducted and where radiotherapy was conducted. However, the differences were not statistically significant (Table 2).
When incidence rate of complications was analyzed for each surgical method, 4 cases were infected out of 8 cases where direct implant insertion was performed. In 5 cases of permanent expander insertion, 3 cases showed occurrence of complications. When expander-implant exchange was performed, complications occurred in 14 cases (Table 3). Difference with statistical significance was not found in each surgical method.
When incidence rate of complications was analyzed for cancer stage, In 7 cases of stage I, 4 cases showed occurrence of complications. In 20 cases of stage IIa, 13 cases showed occurrence of complications. In 5 cases of above stage IIa, 4 cases showed occurrence of complications (Table 4). Difference with statistical significance was not found in each cancer stage.
In the final follow-up, patient’s subjective satisfaction was 4.2 points while score by five plastic surgeons was 5.74 point on average. According to the results of analysis when patients’ subjective scores were divided to three groups, 2-4 points were scored by 16 patients, 5-7 points by 12 patients, and 8-10 points by 4 patients. Average age for each group was 53.1 years, 56.9 years and 62.4 years respectively. Average follow-up period was 7.9 years, 8.5 years and 7.6 years respectively. The positive correlation was found between each score group and average age, whereas such correlation was not statistically significant (Fig. 2).
Patients were asked question about intention to get revision surgery when the final follow-up was performed. The total of 17 patients responded to the question. Three patients answered that they wanted to undergo reoperation for reasons of asymmetry and discoloration of nipple-areolar complex. Among the total, 14 patients answered that they did not want to undergo reoperation. The reasons is that the patients did not feel the need for reoperation because they were relatively satisfied with their silhouette while they were wearing clothes, which showed the largest number of cases in 12 patients. Some patients said that they did not want to undergo operation because they were afraid of general anesthesia and surgery itself.
A patient aged 44 received breast reconstruction using permanent expander immediately after undergoing modified radical mastectomy due to breast cancer in stage 1. Implant with smooth surface and in round shape manufactured by Mentor® was used for the breast reconstruction while saline 315 cc was injected. Post-operative hormone therapy only was performed. Personal satisfaction was 9 points while objective score was 7.2 points. The patient wanted to receive neither reconstruction of nipple-areolar complex nor revision surgery (Fig. 3).
A patient received breast reconstruction with implant insertion after undergoing modified radical mastectomy due to breast cancer in stage IIa. Implant with smooth surface and in round shape manufactured by Mentor was used in saline 250 cc. Post-operative chemotherapy and hormone therapy were performed. Personal satisfaction was 6 points while objective score was 8.1 points. In this case also, the patient wanted to receive neither reconstruction of nipple-areolar complex nor revision surgery (Fig. 4).
A patient aged 47 received breast reconstruction with tissue expander insertion after undergoing modified radical mastectomy due to breast cancer in stage IIb. Post-operative hormone therapy and chemotherapy were performed. Personal satisfaction was 2 points while objective score was 3 points. In this case, the patient had to receive tissue expander removal for infection and pain control in postoperative 6 months (Fig. 5).
Immediate reconstruction of breast using implant has the strong points that the technique is simple and results in non-donor site morbidity after operation. Therefore, such reconstruction technique can be used in case that autologous tissue is insufficient or that a patient is afraid of on donor site scarring or morbidity [3]. In particular, the technique can be used for a patient who does not have large breasts without severe mastoptosis because it can provides satisfactory results also in the aesthetic perspective.
However, the technique has some shortcomings. Complications such as capsular contracture may occur due to implant. Shape and touch are less natural compared to the case where autologous tissue is used. If a patient feels uneasy about use of foreign body, the technique cannot be used. On top of this, in the technical aspect of cancer removal surgery, thickness of skin flap and wound tension vary according to surgeon’s technique and capability. These factors may cause partial necrosis of skin and exposure of implant. Since a patient is likely to experience deterioration of blood circulation on skin after undergoing mastectomy or to show partial necrosis or dehiscence of skin due to tension, there is a risk that implant is exposed directly [4-7]. In addition, there have been insufficient studies on the effects that radiotherapy has on the long-term results of reconstruction among patients who are scheduled to receive post-operative radiotherapy. Therefore, it is difficult to make a stable prediction on the results of reconstruction.
Many studies had been presented about breast reconstruction using implant. According to Hwang et al. [2], average score was 8.2 points for patient group that could be followed up for one year or more after skin-sparing and nipple-areolar-sparing mastectomy and breast reconstruction using Alloderm® and saline-filled implant. The researchers reported that rate of complications such as partial necrosis of skin and capsular contracture was 22.2%. According to Kim et al. [8], it was reported that in the 201 cases where breast reconstruction was performed using saline-filled breast implant, rate of implant removal was 23.9% for reasons of infection (10%), capsular contracture (3.5%) and implant exposure (1.0%). Yanko-Arzi et al. [9] reported that after breast reconstruction using tissue expander and implant, incidence rate of major complications was 18% and that of minor complications was 52%. In this study, incidence rate of complications was 65.6% in total with 28.1% of reoperation, which showed the relatively higher rate of complications compared to previous studies. These results seem to be attributable to the fact that this study targeted only the patient group that could be followed up in the long period and that scope of infection that took up the majority of complications started with the case where erythema was found in this study.
In the patient group that received reoperation due to complications, infection was the cause that showed the highest rate. Incidence rate of infection varied according to study, which showed a big difference in the rate from around 3.5% to 24%. Cause of infection may include retrograde infection in drain tube or saline injection and contamination in the process of surgery.
In this study, patients were divided to whole group, complication group and reoperation group before correlation with each risk factor was examined. When incidence rate of complications was analyzed for risk factors, 11 cases developed complications out of 15 cases where post-operative chemotherapy was performed. And 6 cases developed complications out of 7 cases where post-operative chemotherapy and radiation therapy were performed. In the patient group that received radiotherapy and chemotherapy, the complication group and the reoperation group showed the higher correlation than the whole group, which was not statistically significant. Typically, risk factors of complications after breast reconstruction using implant include patient’s age, breast volume, BMI, surgery time, drain indwelling time, incidence rate of seroma or hematoma, chemotherapy, and radiotherapy. Even though many studies have been conducted, the study results have differed significantly depending on patient group and surgery method. According to Han et al. [10], it was reported that any difference with statistical significance, except BMI and pre-operative breast volume of patient, was not found between risk factors of tissue expander infection and incidence rate of infection. In the study by Kim et al. [8] either, any difference with statistical significance was not found, expect leak of implant and surface type of implant.
For evaluation complication risk by each cancer stage, patients were divided to stage I, stage IIa and above stage IIa. The higher cancer stage, complication rate is elevated, which was not statistically significant.
In regard to breast reconstruction using breast implant, the biggest problem in shape of reconstructed breast itself is that there is almost no mastoptosis according to passage of time and that tendon-side upper breast looks unnatural. In this study also, patient’s subjective satisfaction was 4.2 points in the final follow-up with average score by five plastic surgeons at 5.74 points, which showed the relatively low satisfaction and objective esthetic score. However, only 17.6% of the patients wanted to undergo revision surgery. Even though most of the patients were not satisfied with shape of their breast when they were naked, they were satisfied with breast shape and their silhouette while they were wearing underwear and clothes so that they decided not to undergo revision surgery. One of the reasons is believed to be decreasing aesthetic requirements for breast among group of women who reached menopause while they were followed up in the long period. In effect, this study showed the positive correlation between age and score for each score group. When actual consultation with patient was conducted, interest in revision surgery differed according to age.
In the Michigan breast reconstruction outcome study (the University of Michigan in Ann Arbor of the US), “post-surgery evaluation” was conducted for the items that included shape of breast in naked, bra fitting, a case of wearing swim suit, and a case of wearing clothes, which aimed at evaluation of satisfaction. Evaluation was conducted also for relation between breast shape and sexual satisfaction and for physical attractiveness [11]. In this study, breast shape only was scored for evaluation. According to the long-term follow-up study, most of the patients were not satisfied with breast shape itself. However, such dissatisfaction did not result in patient’s willingness to undergo revision surgery. The patients were found to experience no significant inconvenience in wearing clothes and living a social life.
Evaluation for breast shape can be access breast position, symmetry and ptosis. In this study, there is only simply scoring for breast shape. It is true that subjective scoring and objective scoring simply for breast shape itself have limitations in evaluation of breast shape. Scores of five plastic surgeons have limitation of objective evaluation for breast shape. In particular, when patient group is followed up in the long period, distinct characteristics of such group cannot be ignored.
In this study, various analyses were carried out for each surgical method, each patient group and each risk factor, all of which were not statistically significant. Results of such analyses were not satisfactory to operator or patient. In particular, saline-filled implant was mostly used in the past. Recently, silicone gel implant is increasingly used for reconstruction. Also, oncoplastic surgery technique is frequently used for patient group that has undergone breast conserving surgery and have small to moderate size breast, especially East Asian people [12]. As a result, it is difficult to make a simple comparison between the previous results and the results of reconstruction with currently used implant. As there are a variety of shapes and materials of implant with much wider range of selection for surgical method, it is possible to expect better results than in the past. This study was conducted to analyze satisfaction and complications in the patient group that was followed up in the long term period after breast reconstruction with the previously used implant. In this sense, it is believed that the results of this study will be useful as reference to other researches or patients in the future.
The authors conducted the study that targeted the patients that could be followed up for at least five years or more among the patients who underwent breast reconstruction that used prosthesis. According to the study results, the incidence rate of complications was relatively high, which resulted in the high rate of revision surgery. In addition, the final follow-up showed that satisfaction with breast shape was low. The reasons are believed to be complex: implant itself is infected, implant is ruptured, or difference between contracture and tendon-side breasts gets bigger with advancing years. Based on the results of this study, it is difficult to draw a conclusion that breast reconstruction using prosthesis does not lead to good results from long-term follow-up. However, the results of this study will be useful to conduct a future study on comparison with long-term follow-up for breast reconstruction that uses autologous tissue or comparison with breast reconstruction that uses silicone implant that is currently used frequently. Furthermore, the results of this study suggest the need to have preoperative and postoperative consultation sufficiently with patient on various issues that include high rate of infection in breast reconstruction using prosthesis, which was found in this study, complications such as partial necrosis of tissue and possibility of prosthesis removal due to such complications, dissatisfaction with breast shape in the future, and deterioration of asymmetry that may occur in the long term. In addition, the results of this study can be useful as reference when an operator selects a proper surgical method.
Notes
This study was presented in ‘2012 Taipei International Breast Cancer Symposium & International Oncoplastic Breast Surgery Symposium with the 4th Cross Strait conference on Breast Cancer Treatment Consensus’ as Poster presentation.
Fig. 3.
Case 1. A patient aged 44 received breast reconstruction using permanent expander immediately after undergoing modified radical mastectomy due to breast cancer in stage 1. The photograph is seven years postoperative view.
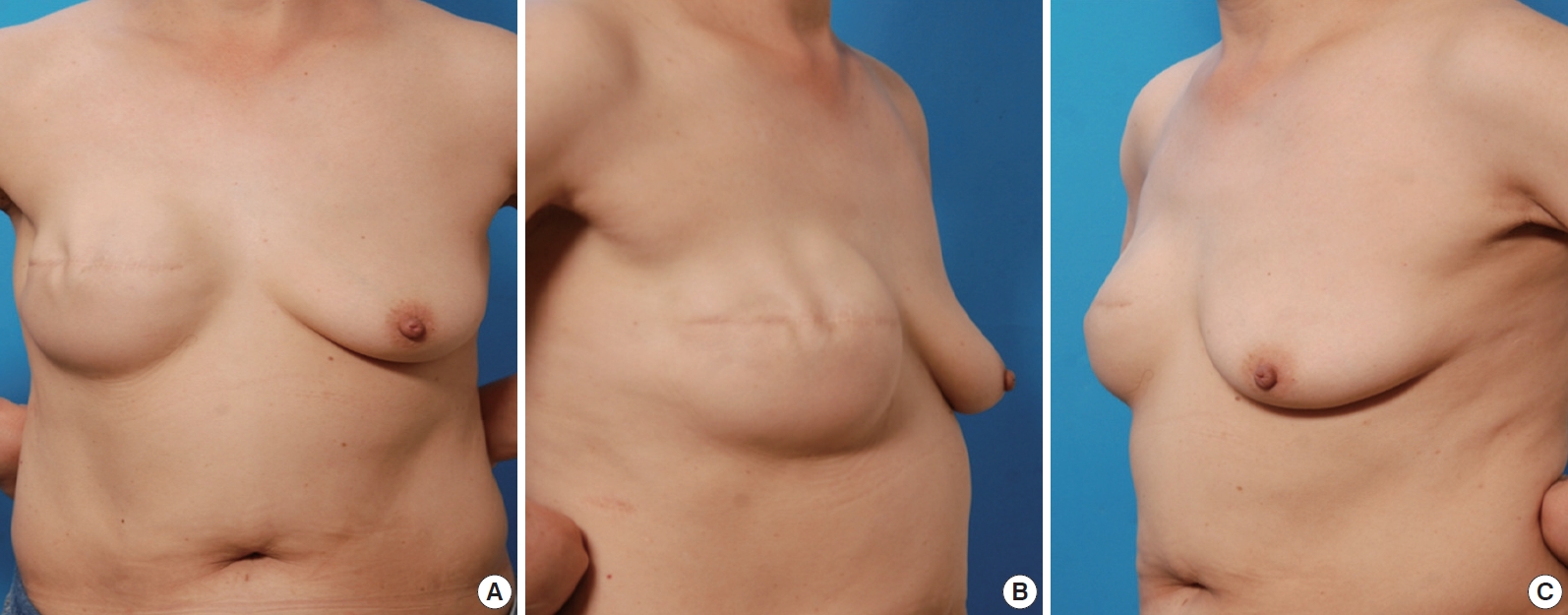
Fig. 4.
Case 2. A patient received breast reconstruction with implant insertion after undergoing modified radical mastectomy due to breast cancer in stage IIa. The photograph is eight years postoperative view.
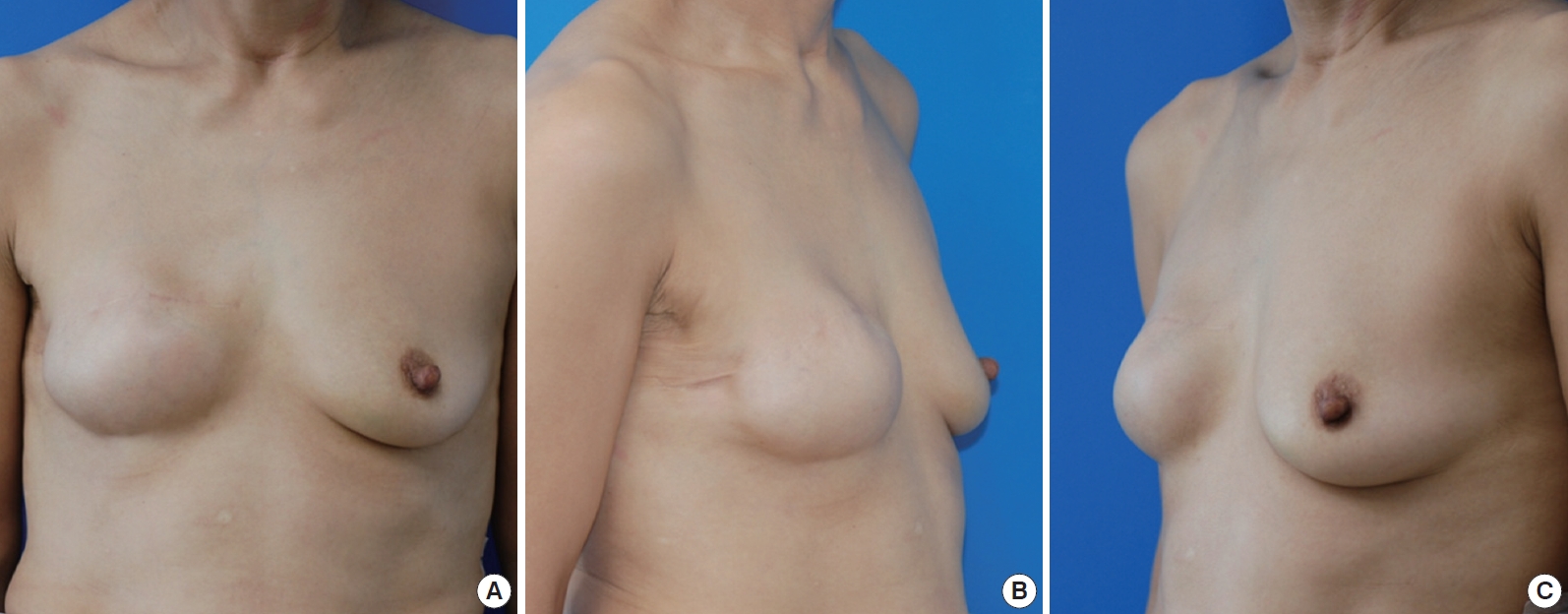
Fig. 5.
Case 3. A patient aged 47 received breast reconstruction with tissue expander insertion after undergoing modified radical mastectomy due to breast cancer in stage IIb. The photograph is preoperative view of tissue expander removal for infection and pain control in postoperative 6 months.

Table 1.
Whole Characteristics of the entire patients
Table 2.
Complication rates separated by risk factors
Table 3.
Complications separated by reconstruction methods
REFERENCES
1. Stephen J. Mathes, Vincent R. Hentz: Mathes Plastic Surgery. 2nd ed. Philadelphia: W.B. Saunders, Elsevier; 2006.4: p. 674.
2. Hwang CH, Kim EK, Eom JS, et al. Immediate Breast Reconstruction Using Saline Implant: Extension of Pectoralis Major Muscle Coverage with Alloderm®. J Korean Soc Plast Reconstr Surg 2009;36:161-6.
3. Kronowitz SJ, Robb GL, Youssef A, et al. Optimizing autologous breast reconstruction in thin patients. Plast Reconstr Surg 2003;112:1768-78.


4. Spear SL, Pelletiere CV. Immediate breast reconstruction in two stages using textured, integrated-valve tissue expanders and breast implants. Plast Reconstr Surg 2004;113:2098-103.


6. Tebbetts JB. A system for breast implant selection based on patient tissue characteristics and implant-soft tissue dynamics. Plast Reconstr Surg 2002;109:1396-409.


8. Kim IK, Lee JH, Kim YH, et al. Clinical Durability and Deflation of Saline-Filled Breast Implant in Breast Reconstruction. J Korean Soc Plast Reconstr Surg 2011;38:808-14.
9. Yanko-Arzi R, Cohen MJ, Braunstein R, et al. Breast Reconstruction: Complication Rate and Tissue Expander Type. Aesth Plast Surg 2009;33:489-96.


10. Han SB, Lee DW, Lew DH. Risk Factors of Tissue-Expander Infection in Breast Reconstruction. J Korean Soc Plast Reconstr Surg 2011;5:621-6.
11. University of Michigan. Michigan Breast Reconstruction Outcome Study. DAMD17-94-J-4044. Ann Arbor, Michigan: United states; 1998. p. 22.
-
METRICS

-
- 1 Crossref
- 3,966 View
- 55 Download
- Related articles in AAPS







