Liposuction with Diode Laser Ablation for Treatment of Axillary Osmidrosis
Article information
Abstract
Background
Liposuction and laser ablation for treatment of osmidrosis are leading treatment methods for osmidrosis and have less complication compare to conventional surgical method. We treated patients with the two methods simultaneously to maximize the efficiency for less complication.
Methods
18 patients with axillary osmidrosis (total 36 axillae) were included in this study. They had been treated by liposuction with diode laser ablation from December 2011 to August 2012. The results of operation was assessed by questionnaire subjectively and microscopic study objectively.
Results
18 patients were followed over 10 months postoperatively (range, 10 to 18 months; mean, 13.8 months). The patients were satisfied with their results in terms of reduced foul odor except one patient. No hematoma, infections, skin necrosis, hair loss or hypertrophic scar occurred. And there was quantitative reduction of apocrine glands in microscopic study.
Conclusions
We suggest that simultaneous apply of liposuction with laser ablation which is clinically and histologically proven method for treatment of axillary osmidrosis could be more effective method than treatment with each method alone, and has same morbidity allowing the patients early exercise.
INTRODUCTION
The main characteristic of axillary osmidrosis is excessive malodor originating from the apocrine glands which is induced by the influence of androgens and thus is often associated with hyperhidrosis [1]. There are many methods of treatment of osmidrosis. In other word, there is no definite treatment of choice. Every treatment method has its own advantages and disadvantages. One of the most common disadvantages is recurrence and dissatisfaction of patient. Conventional surgical interventions such as en bloc resection, dermal shaving, subdermal defatting of axillary hear bearing skin have low recurrent rate but they have high perioperative morbidity have such as hematoma, skin necrosis and massive scar causing limit of motion. And simple methods such as ultrasonic aspiration, liposuction and laser treatment have low perioperative morbidity but they have inconsistent effectiveness and high recurrent rate. There are also nonsurgical procedures such as application of aluminum compounds, iontophoresis, oral medication, injection of botulinum toxin A [2-7].
Nowadays, patients who seek more ideal treatment modality need not only a high success rate, but also fewer complications, less scarring, and faster recovery. Liposuction and laser ablation for treatment of osmidrosis are leading treatment methods for osmidrosis and have less complication compare to conventional surgical method. We treated patients with the two methods simultaneously.
METHODS
Eighteen patients with axillary osmidrosis (total 36 axillae) were included in this study. We included patients who had been treated by liposuction with diode laser ablation from December 2011 to August 2012. We survey the social history of each patient by questionnaire preoperatively.
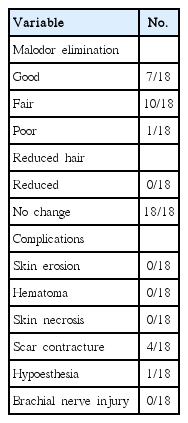
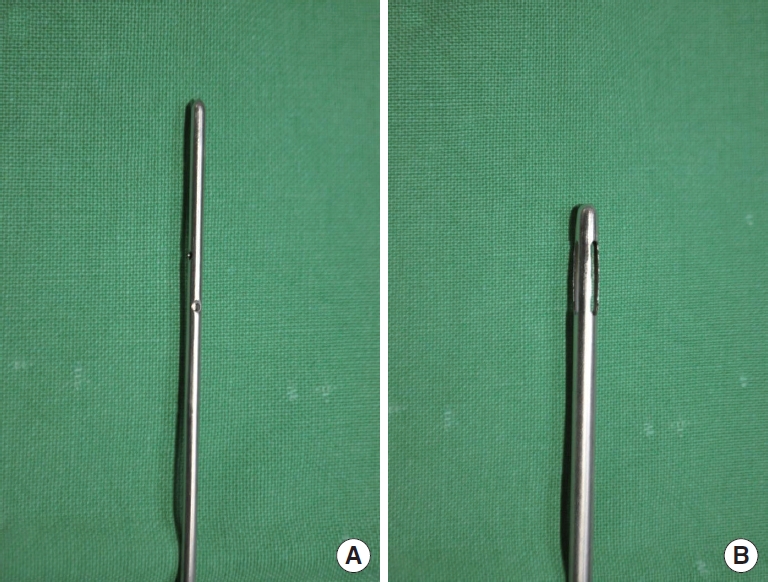
All patients underwent operation under local anesthesia with tumescence. We used blunt cannula with three hole (Fig. 1). And we used DIOMED SURGICAL laser (UK), which is a 810 nm diode laser. The microcannula with a diameter of 1.5 mm within protector is used to protect the normal tissue and make it easy to manipulate the heat source destructing deep dermal apocrine glands (Fig. 2).
The infiltration needle (A) and liposuction cannula (B). We used the cannula with three hole to prevent loading excessive pressure for preserving vessels and nerves.
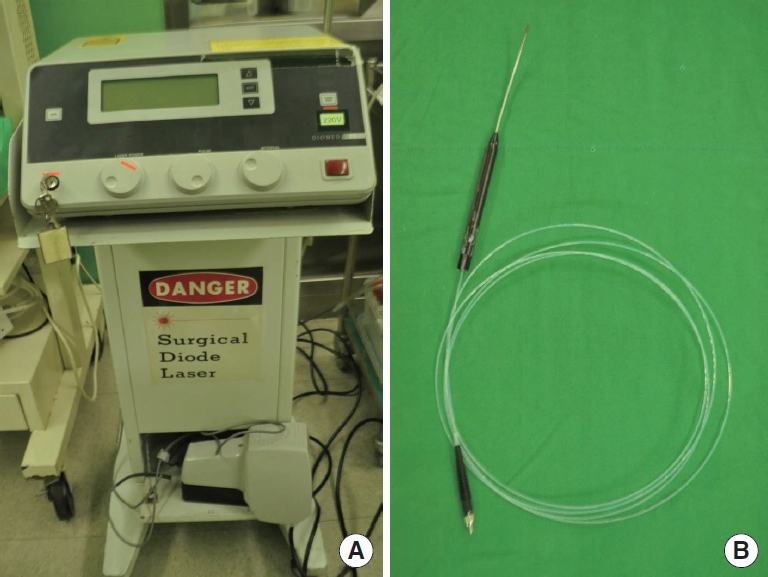
Diode laser (A) and its microcannula (B). We used DIOMED SURGICAL laser (UK), which is a diode laser. The microcannula with a diameter of 1.5 mm within protector is used.
The clinical results were assessed subjectively by patients themselves on outpatient department follow up day or on the telephone on 10 months postoperatively. We carried out preoperative and postoperative biopsy of axillary skin to compare number of apocrine glands between preoperative and postoperative axillary skin. We also checked whether there were apocrine glands in suctioned fat. The biopsy specimens were checked by pathologists and the apocrine and eccrine glands were counted under microscope for quantitative analysis.
Operative Technique
The hair-bearing area of bilateral axillae was marked. We didn’t shave the hairs of axillae. Two stab incision (5 mm) were made at the one fourth and three fourth area of the marked area. And preoperative incisional biopsy was done at the highest portion of axillary fold where is the highest density of apocrine gland in axilla [8]. Marked hair hearing axillary area was infiltrated through the incision with 200 to 300 mL of tumescent solution. The manual syringe liposuction was done with negative suction pressure of 5 cc with 20 cc syringe The aspiration volume was 15 to 20 mL from each axilla (7-10 mL of pure fat). After the liposuction, ablation with diode laser was done. We inserted the microcannula through subcutaneous tunnel first, and the laser was only applied with an extracting motion of approximately 5-15 mm/second scraping the undersurface of skin flap. We repeated this procedure by crisscross pattern. We irrigated cold saline and ice packs were applied to the treated area to prevent thermal injury of the skin during the operation. Totally, each axilla was exposed to thermal energy about 300 J (9 W for about 5-6 minutes) (Fig. 3). After the procedure, we did postoperative punch biopsy at the just medial to the preoperative incisional biopsy area. The wound of incisional biopsy was sutured simply with nylon. And other 2 stab incisions were healed by secondary intension. Light compressive dressing was applied for 24 hours postoperatively. We opened the wound with application of antibiotic ointment, and the patients were allowed to take a shower at postoperative day 2. The stitches were removed at postoperative day 7.

Marking of hear bearing axillary skin. We get the incisional biopsy specimen at the area of highest portion of axilla where the apocrine glands are widely distributed. (A) We performed manual liposuction to avoid excessive pressure loading on subcutaneous tissue. (B) We kept cooling with cold water and ice pack during ablation of subcutaneous tissue with laser. (C) Suctioned fat was collected and studied under microscope for containing glands.
RESULTS
Eighteen patients were followed over 10 months postoperatively (range, 10 to 18 months; mean, 13.8 months). Ten male patients and eight female patients were included. On preoperative survey of social history, 16 patients (88.9%) had familial history. Ten (55.5%) patients complained difficulty of social life due to malodor. Sixteen patients (88.9%) thought about axillary malodor of themselves as moderate to severe, which is the degree of triggering displeasure.
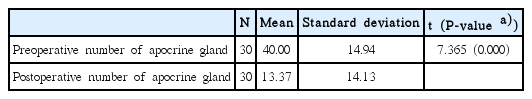
We performed biopsy to the 15 patient. The number of glands in biopsy specimens was counted under × 100 magnification microscopic field by pathologist. The result of biopsy shows reduced the number of apocrine glands of 14 patient. The number of apocrine gland was decreased significantly (P< 0.05) (Tables 1, 2, Fig. 4).
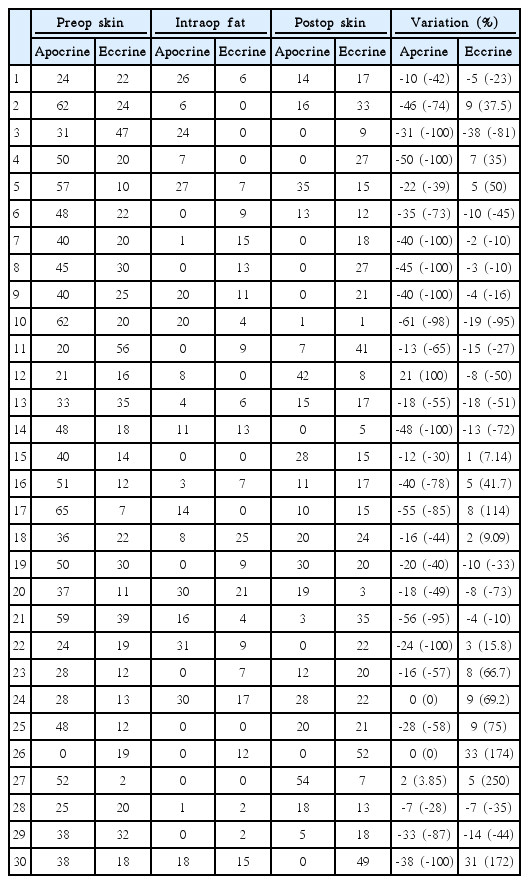
The numbers of apocrine and eccrine gland of preoperative and postoperative skin biopsy and intraoperative fat tissue.

Findings of preoperative biopsy (A) and postoperative biopsy (B) of axillary skin. There are many apocrine glands (AG) and eccrine glands (EG) on the preoperative biopsy. After procedure, the postoperative biopsy shows only few eccrine glands within destructed dermal portion of skin and absence of apocrine gland. H&E staining; magnification × 40.
The patients were satisfied with their results in terms of reduced foul odor except one patient (94.4%). Four patients (3 patient with both axillae, and one patient with one axilla) complained about scar contracture. They got better spontaneously with massage and physical exercise. And one patient complained about hypoesthesia. No hematoma, infections, skin necrosis, hair loss or hypertrophic scar occurred (Table 3). No patient was complained about postoperative pain, discomfort due to compression which is common on patient who get conventional subdermal excision. All patient could be discharged and go back to work on postoperative day 1.
DISCUSSION
Osmidrosis patients are suffered from disturbance of social life more than from its own four odor. Mild cases could be managed by good hygiene and regular use of deodorants and antiperspirants. However, severe cases are not effective at conservative management, resulting in heightened self consciousness and even sometimes social reclusion and exclusion.
Foul odor is caused by secretions from the apocrine and eccrine glands. Bang et al. [9] reported increased the number and size of apocrine glands in osmidrosis patients compare to control groups in histopathologic study. And the treatment goal is aimed at elimination of glands or block secretion from glands. Conventional surgical treatments have effective results but also high morbidity such as hematoma, seroma, skin necrosis and severe scarring [10]. And limit of axillary motion due to contracture, irregular hair loss were frequently seen in long term results. Ant discomfort due to routine bulky compressive dressing for at least 2 weeks was inevitable [5].
To reduce these complications, other surgical options was developed for treatment of osmidrosis. Ou et al. [6] reported superficial liposuction technique for treatment of osmidrosis. They reported improvement of symptom without severe complications. Perng et al. [11] reported comparative study of liposuction and partial excision of axillary skin and subcutaneous tissue. They suggested liposuction as procedure with fewer complication but less effective than conventional surgery. They reported 80.7% of satisfaction rate in patients with liposuction and 91.18% with conventional surgery. Kota et al. reported laser ablation as a effective treatment of osmidrosis. They used carbon dioxide and neodymium yttrium-aluminum-garnet laser. They reported effectiveness of laser treatment with less complication. They reported 100% of satisfaction rate [12]. In this study, 94.4% of the patients were satisfied with reduced foul odor.
In this study, we focused on the location of apocrine glands in the skin. The apocrine glands are located in deep dermis and superficial subcutaneous layer [8]. Conventional liposuction targeted on apocrine glands located in superficial subcutaneous layer, and laser treatment targeted on apocrine glands located in superficial subcutaneous and deep dermal layer. And thermal energy from 810 nm diode laser which was transmitted to dermis destructed the adjacent apocrine glands directly. Lee et al. [13] reported microscopic study of secondary contracture of destructed deep dermis and subcutaneous layer on healing process destruct adjacent remnant glands mechanically after axillary liposuction. We suggest that thermal contracture induced by diode laser accelerates this mechanism.
To reduce the complication, we used blunt liposuction cannula with three holes to prevent loading excessive pressure for preserving vessels and nerves. The range of liposuction was limited to superficial subcutaneous fat for protection of underlying axillary vessels and nerves. During liposuction, we try not to manipulate liposuction tip heading to thoracic wall for prevention of postoperative hemopneumothorax. And we choose diode laser for heat source to cause direct thermal injury to adjacent tissue surrounding fiber tip not to overlying skin. We kept cooling the overlying skin by cold saline irrigation and apply of ice packs for safer procedure. In consequence we could get effective result with less complication.
After surgery we could get the patients discharged immediately and returned to daily life without postoperative pain and bulky dressing as in conventional surgical methods. Most importantly, we could get objective result of quantitative improvement and satisfaction of the patients.
In conclusion, liposuction and laser ablation treatment have less complication compared to conventional surgical treatment of axillary osmidrosis. We suggest that simultaneous apply of liposuction with laser ablation for treatment of axillary osmidrosis could be more effective method than treatment with each method alone with low morbidity allowing the patients return to daily life early.
Notes
No potential conflict of interest relevant to this article was reported.