|
 |
- Search
| Arch Aesthetic Plast Surg > Volume 25(2); 2019 > Article |
|
Abstract
Conventional sub-orbicularis oculi fat (SOOF) lifting during lower blepharoplasty is performed by anchoring the SOOF to the periosteum of the infraorbital rim. This procedure helps to improve the concavity at the central portion of the lower eyelid and the lid-cheek junction. However, over time, the periosteum becomes progressively weaker, diminishing the anchoring effect. This paper introduces a new lower blepharoplasty technique in which the SOOF is fixed to a bony hole to strengthen the holding force and provide sustainability.
Lower blepharoplasty is performed to correct lower eyelid skin loosening and tear trough deformities. Traditional lower blepharoplasty focuses only on removing the excessive skin and on correcting tear trough deformities. However, this traditional method has some limitations. The method cannot correct concavity at the central portion of the lower eyelid and the lid-cheek junction [1]. In particular, elderly patients complain about these limitations. To overcome these problems, attempts have been made to lift the sub-orbicularis oculi fat (SOOF) during lower blepharoplasty [2,3]. The advantage of SOOF lifting is that it has a filling effect at the lid-cheek junction and lower eyelid. In addition, SOOF lifting prevents lengthening of the orbital height caused by age-related sagging of the malar fat pads [2].
To perform SOOF lifting, the SOOF is first dissected and then elevated. The SOOF is then anchored to the periosteum of the infraorbital rim [4]. Using the conventional technique, fixation of the SOOF to the periosteum can be performed easily and quickly. However, over time, the periosteum becomes progressively weaker, diminishing the effect of fixation. In particular, because the periosteum is weaker in the elderly, the bearing capacity of the periosteum is expected to decrease significantly. This paper introduces a new lower blepharoplasty technique in which the SOOF is fixed to a bony hole to strengthen the holding force and provide sustainability.
A routine subciliary incision is made 2 mm below the ciliary line with a lateral extension. The skin flap is then elevated, while preserving the pretarsal orbicularis oculi muscle as much as possible. The septal portion of the orbicularis oculi muscle is then divided using iris scissors. The dissection is then performed up to the arcus marginalis through the preseptal plane. The arcus marginalis is then released by electrocautery, and a subperiosteal dissection is performed below the inferior orbital rim for approximately 1 cm along the medial half of the orbital rim. This subperiosteal dissection is performed on top of the periosteum past the inferior margin of the tear trough deformity. The SOOF is then identified inside the elevated flap.
Next, a bony hole is made at the lateral third of the infraorbital rim to fix the SOOF, using a 1.14-mm Kirschner wire drill to drill an oblique hole through the orbital margin (Fig. 1). A 4-0 nylon suture is then passed through the drill hole with the upper part of the SOOF hanging, and cephalad tension is placed on the suture to elevate the SOOF (Fig. 2). The suture is then tied approximately five times with the appropriate tension.
Generally, two SOOF anchoring sutures are fixed in the bony hole. Depending on the elevation vector required, the SOOF anchoring point is different each time. Nonetheless, anchoring two sutures to the bony hole is essential to obtain sufficient elevation force. Occasionally, the two sutures alone may not achieve the desired elevation, or SOOF lifting may be biased in one direction. In such cases, the two SOOF anchoring sutures are first fixed to the bony hole. One or two SOOF anchoring sutures are then added to the medial side of the infraorbital rim periosteum in accordance with the desired vector to compensate by elevating in the appropriate direction.
From this point, the procedure is similar to that of conventional lower blepharoplasty. In patients with severe orbital fat herniation, fat repositioning is performed to spread the herniated fat downward and sideward, and the orbicularis oculi muscle is then suspended to the lateral orbital rim. Finally, the remaining orbicularis oculi muscle and skin is sutured layer-by-layer, and the operation is completed.
A youthful lower lid is vertically short with concavity over the orbital septum that smoothly transitions to the convexity of the cheek above the infraorbital rim [5]. With aging, the elasticity of the lower eyelid skin decreases and the lower eyelid fat sags. In addition, the orbital retaining ligament depresses the lid-cheek junction, and the orbital fat sags and protrudes to form a tear trough deformity [6]. These aging-related changes in the lower eyelid are the main reason why elderly individuals request lower blepharoplasty. Thus, techniques such as excessive skin excision or fat repositioning are considered for these purposes. In addition, if SOOF lifting is simultaneously performed, the outcomes of surgery can be improved significantly [2,3].
The SOOF extends inferiorly within the zygomaticus muscle system and is continuous with the superficial musculoaponeurotic system. Therefore, SOOF lifting has the effect of producing a younger midface by filling the fat pad to the lid-cheek junction [7]. Fixation of the SOOF to the periosteum has already been introduced, but it is believed that this method cannot provide firm, long-lasting fixation. If considerable time passes with the nylon thread in the periosteum, the periosteum becomes stretched or torn because of the ŌĆ£cheese wire effect.ŌĆØ Therefore, fixation to the bony hole is expected to be firmer and more secure than fixation to the periosteum. In addition, this technique enables durable bony fixation by reducing tension on the lower eyelid, since the SOOF is secured tightly to the bone.
This method may appear invasive and cumbersome because it requires drilling a hole in the bone. However, in the authorsŌĆÖ experience, this procedure can be performed quite easily. In addition, this method only requires 5 minutes longer than conventional periosteal fixation. Furthermore, local anesthesia with intravenous sedation is sufficient for making a drill hole. Yaremchuk [8] introduced the use of titanium screws instead of bony holes in SOOF fixation. He fixed a titanium screw to the lateral third of the infraorbital rim and anchored the SOOF and malar fat pads to this titanium screw. He consequently obtained a satisfactory midface elevation effect. However, the bony hole method proposed herein does not fix the screw to the bone, but instead uses only the drill hole. Therefore, there are no concerns about a foreign body reaction or contact with foreign material. In addition, this method is cheaper, and can be performed more easily in less time than the screw fixation technique.
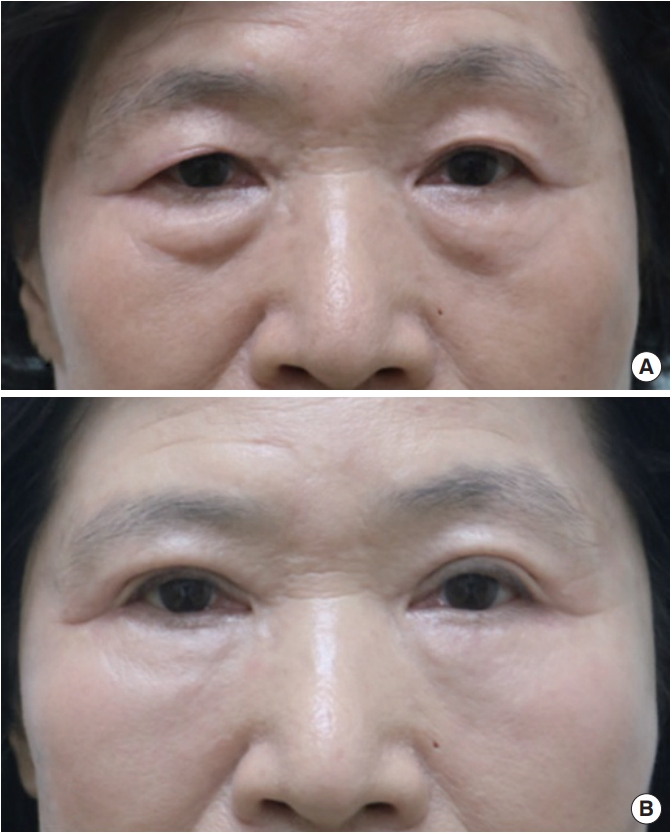
When comparing the preoperative and postoperative clinical photographs of a 60-year-old female patient who underwent this procedure, a soft tissue filling effect of the palpebromalar grooves was clearly observed. The patient had excessive lower eyelid skin loosening and orbital fat bulging prior to surgery. In addition, she had a definite palpebromalar groove due to volume loss on the mid-cheek. An obvious cosmetic improvement was observed at 6 months postoperatively (Fig. 3). The filling effect was particularly prominent around the palpebromalar groove, where SOOF lifting with bone fixation was performed.
Although not previously applied to lower blepharoplasty, the use of a drill hole for midface lifting has been reported [7]. Correa et al. [7] made a transconjunctival incision with an oral mucosa (upper gingivobuccal sulcus) incision and elevated a wide mid-cheek flap. They then anchored the soft tissue of the midface broadly, including the buccal fat pad and buccinator muscle. Finally, midface lifting was performed by fixation to a bony hole in the infraorbital rim. Correa et al. used this technique to reinforce midface lifting, whereas in the method proposed herein, the aim was to improve the results of lower blepharoplasty in elderly patients. Therefore, their method differs from ours in that they used a wide and broad mid-cheek soft tissue flap, whereas in our proposed method, the SOOF is elevated selectively and fixed to the bony hole.
In conclusion, the proposed method is not aimed at overall midface lifting, but is instead intended to improve the results of lower blepharoplasty in the elderly. SOOF lifting via fixation to a bony hole can enhance long-term stability and provide secure fixation. Therefore, this technique can be considered a good and easy option, without concerns regarding severe complications, for lower blepharoplasty in elderly patients.
Notes
Ethical approval
The study was performed in accordance with the principles of the Declaration of Helsinki.
Patient consent
The patient provided written informed consent for the publication and the use of her images.
Fig.┬Ā1.
A bony hole was made in the lateral third of the infraorbital rim with a 1.14-mm Kirschner wire drill.

REFERENCES
1. Aiache AE, Ramirez OH. The suborbicularis oculi fat pads: an anatomic and clinical study. Plast Reconstr Surg 1995;95:37-42.


2. Jeon YR, Rah DK, Lew DH, et al. Pretarsal augmented lower blepharoplasty. Plast Reconstr Surg 2016;138:74-82.


3. Freeman MS. Transconjunctival sub-orbicularis oculi fat (SOOF) pad lift blepharoplasty: a new technique for the effacement of nasojugal deformity. Arch Facial Plast Surg 2000;2:16-21.


5. Mendelson BC. Fat preservation technique of lower-lid blepharoplasty. Aesthet Surg J 2001;21:450-9.



6. Lucarelli MJ, Khwarg SI, Lemke BN, et al. The anatomy of midfacial ptosis. Ophthalmic Plast Reconstr Surg 2000;16:7-22.