Clinical characteristics of and therapeutic approach to complications due to the injection of foreign material in the face: a retrospective study
Article information
Abstract
Background
Soft tissue fillers are increasingly used to rejuvenate and beautify the body and face. Unknown foreign materials that have not always been proven to be safe for human use have been used for injections in the past. Various commercial injectable materials have since been developed and are used; however, the number of complications has increased as soft tissue fillers have increased in use.
Methods
A retrospective study of 39 patients with facial foreign body complications who underwent surgical treatment between March 2012 and February 2021 was conducted. Patient information was analyzed, and patient satisfaction was evaluated using a questionnaire after surgical treatment. A comparative statistical analysis was undertaken.
Results
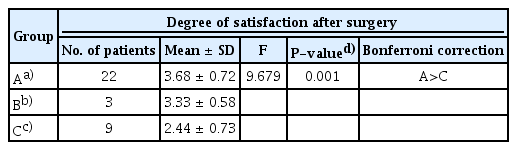
Patients who underwent procedures performed by unlicensed practitioners tended to be older at the time of presenting to the hospital (P=0.004). The degree of satisfaction after surgical repair was significantly lower following the direct approach than after the indirect approach using a bypass incision (P=0.044). The degree of satisfaction significantly decreased (P=0.001) as the number of operations the patient received increased.
Conclusions
When treating complications caused by foreign material injections, surgical removal is a more reliable method than treatment with medication or further injections; however, treatment decisions should be made thoughtfully, and many factors must be considered. Patient satisfaction can be improved by reducing the number of operations and making the appropriate corresponding incisions or excisions to treat the full range of symptoms caused by foreign substances and by indirectly using bypass incisions to mitigate post-surgery scars.
INTRODUCTION
Efforts to improve one’s physical beauty have persisted for centuries. Many people throughout history have attempted to shape the contours of their faces and bodies using various substances, and this phenomenon continues to this day. Fillers are more common than, and are preferable to, other substances since they require a shorter recovery period, are relatively less invasive, and are simple to apply [1]. In recent years, various injectable materials with improved stability have been developed and are increasing in use. However, their introduction for commercial use is very recent, and in the past, unknown or untested foreign materials that had not been approved were used for such injections.
The first filler procedure was reported in 1893 when Neuber [2] performed a transplantation of autologous fat from a patient’s arm to alter a facial defect. In the 1980s, bovine collagen (Zyderm I/II and Zyplast; Inamed Corp., Santa Barbara, CA, USA), which was approved by the U.S. Food and Drug Administration, was developed as the first available version of the cosmetic injectable fillers examined in this study [3].
Various medical fillers with increased stability have been developed in recent years and are now used, but the number of complications, such as foreign body granuloma, has increased due to their more widespread use. If complications occur, conservative treatment can be performed according to the patient’s symptoms. Treatment options may include injection based on the previously injected materials, local or systemic steroid therapy, or surgical resection. In this study, we examined various cases in which patients received foreign material injections at our center, conducted an analysis of the patients’ clinical characteristics based on the therapeutic approach used to treat complications, and conducted a literature review.
METHODS
Ethics statement
This study was approved by the local institutional review board and was performed in accordance with the principles of the Declaration of Helsinki. The informed consent was waived because this design is a retrospective study.
Study design and patients
This retrospective study was designed to include patients who received surgical treatment from a single surgeon and who visited our plastic surgery clinic between March 2012 and February 2021 with complications after injection with foreign material in the face. Patients who received injections with substances into non-facial areas, did not undergo surgery, or had no records concerning postoperative follow-up were excluded from the study. All patients underwent preoperative and postoperative evaluations with a follow-up time of approximately 6 months after the operation.
Data collection
During a visit, patients were given a printed questionnaire survey to evaluate their overall satisfaction. Patient information was also collected and reviewed, including age, sex, symptoms at the time of admission, duration between foreign material injection and surgery, site of occurrence, type of material injected, practitioner type, and injection site.
Therapeutic methods
Based on their symptoms, patients with severe deformities and inflammation were treated conservatively using antibiotics and steroids, followed by surgical resection. The surgical approach was selected based on the site of occurrence, and the method of wound coverage after resection was selected based on the severity and extent of symptoms.
Satisfaction questionnaire
After surgical treatment, patients were either hospitalized or discharged as outpatients, and wound management and follow-up evaluations were performed. The satisfaction questionnaire was completed by patients who agreed to participate. All patients voluntarily and anonymously participated in the survey.
A 5-point scale was used to evaluate the degree of patient satisfaction after surgery based on an overall satisfaction rating of 1 (very unsatisfied) to 5 (very satisfied). Specific criteria, such as facial contouring, foreign body sensation, and inflammation, were used to examine satisfaction or dissatisfaction. The sample questionnaire was as follows: (1) satisfaction after surgery (1=very unsatisfied, 2=unsatisfied, 3=neutral, 4=satisfied, 5=very satisfied); (2) if you are satisfied, which item are you satisfied with? (facial contouring, foreign body sensation, inflammation, other); (3) if you are unsatisfied, which item are you unsatisfied with? (facial contouring, foreign body sensation, inflammation, other).
Statistical analysis
Statistical analysis was performed using SPSS Statistics for Windows, version 27 (IBM Corp., Armonk, NY, USA). The independent t-test was used to analyze the association between the type of practitioner and the patient’s age. Postoperative satisfaction according to the surgical method was also compared using the same method. The Fisher exact test was used to evaluate the relationship between the type of practitioner, the period from the injection to hospitalization, and the injected materials. Moreover, the Fisher exact test was also used to undertake a comparative analysis of the period until hospital visitation based on the number of affected sites due to complications. The number of operations and post-surgical satisfaction were compared using one-way analysis of variance, and the Bonferroni correction was used for post-hoc analysis. Statistical significance was set at P<0.05.
RESULTS
Demographics
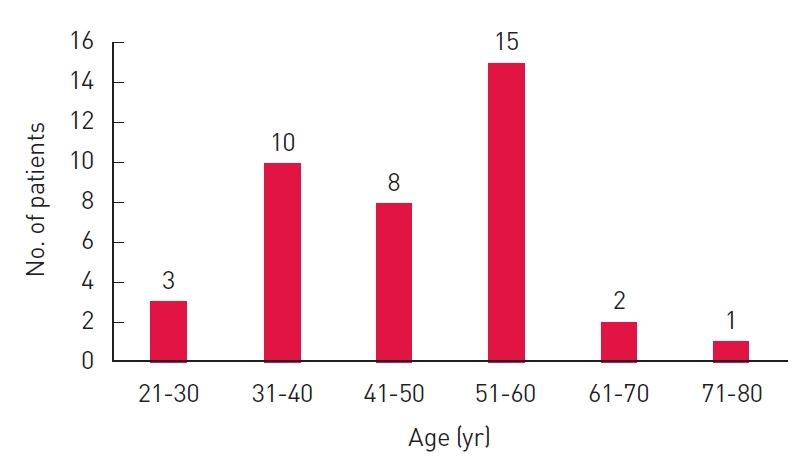
Between March 2012 and February 2021, 39 patients (38 women, 1 man) who had foreign materials injected into their faces underwent surgical resection. The most common age ranges at the time of admission were 51 to 60 years (15 patients, 38%) and 31 to 40 years (10 patients, 26%). The average age of patients was 47 years (Fig. 1).
The primary symptoms reported by patients included inflammation, such as swelling, redness, and pus-like discharge (21 patients, 54%); masses (11 patients, 28%); discomfort, such as a pulling sensation (5 patients, 13%); facial contour deformation (1 patient, 2%); and skin pigmentation (1 patient, 3%) (Fig. 2).

Photographs of the primary symptoms reported by the patients. (A) A 57-year-old woman with signs of infection, such as fever, pain, and puslike discharge on the face. (B) A 34-year-old woman with palpable lumps on the lower lip. (C) A 65-year-old woman with discomfort, including a pulling sensation on the glabella. (D) A 53-year-old woman with a facial contour deformity on the glabella. (E) A 50-year-old woman with pigmentation on the tip of the nose.
The duration from the onset of symptoms to the hospital visit differed for each patient. The average period from the injection of foreign material to treatment was 8 years. Nineteen patients visited a hospital after more than 10 years, 17 waited more than 1 year but less than 10 years, and four waited less than 1 year (Fig. 3). At the time of foreign material injection, 27 patients (69%) received injections from unlicensed practitioners and 12 (31%) received injections from physicians.

Period from the injection of foreign materials to the first hospital visit. Groups were defined as follows: A (period, <1 year), B (period, 1–9 years), and C (period, ≥10 years).
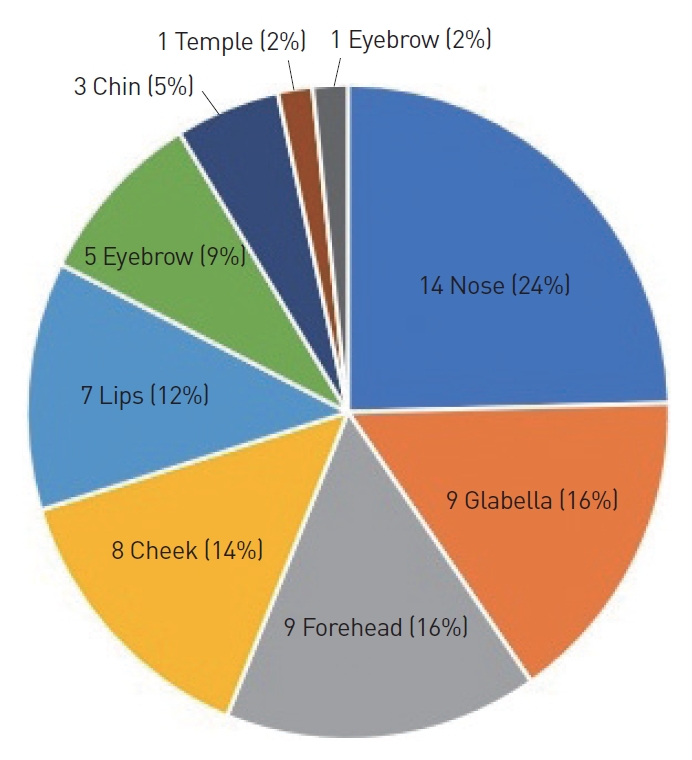
The most common symptom site was the nose, which affected 14 patients (24%), followed by the glabella (9 patients, 26%), forehead (9 patients, 16%), cheek (8 patients, 14%), lips (7 patients, 2%), eyelid (5 patients, 9%), chin (3 patients, 5%), temple (1 patient, 2%), and eyebrow (1 patient, 2%). Ten patients had symptoms at complex sites (Fig. 4).
Most patients (32/39, 85%) did not know what the injected material was, while seven patients recalled that the injected substance was collagen.
Surgical treatment
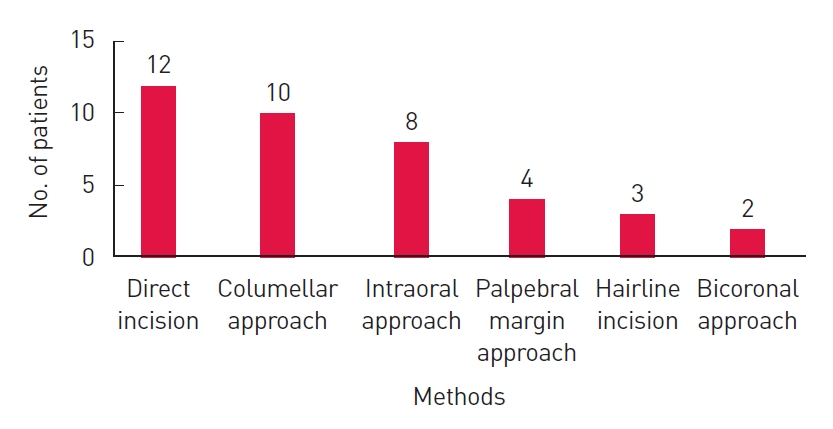
Each patient was treated with antibiotics or steroids if their symptoms, such as inflammation, were severe. After the patients’ symptoms were managed, surgical removal was performed. The surgical approach was selected based on the site of symptom occurrence and severity and was either (1) a direct approach through a direct incision or (2) an indirect approach through the area around the site where the symptoms developed. The direct approach was used for 12 patients (31%). Among the patients who underwent the indirect approach, the mid-columellar approach was used for 10 (26%), the intraoral approach for eight (20%), the palpebral margin approach for four (10%), the hairline approach for three (8%), and the bicoronal approach for two (5%) (Fig. 5).
The coverage method was chosen based on the extent of the wound after surgical resection. The most common method used was simple sutures after removal in 19 patients (49%). When wide defects developed after excision, flap coverage was performed in 16 patients (41%), and simultaneous flap coverage and skin grafting were performed in four patients (10%) (Fig. 6).

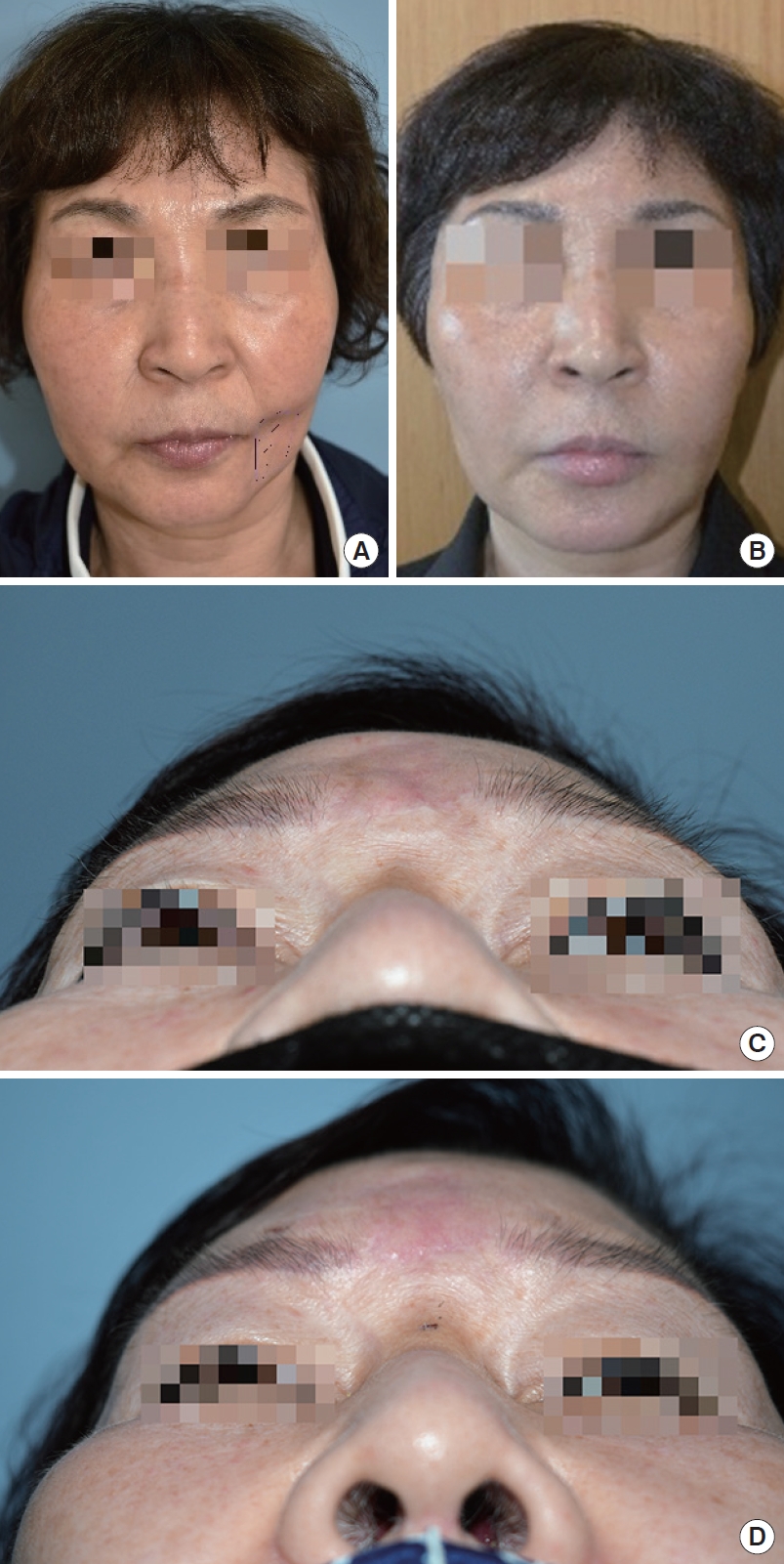
A 57-year-old woman with complications. The symptoms caused by injected foreign materials are more severe and wide; therefore, it was necessary to sufficiently remove the skin and surrounding tissues of the granulomas through the direct approach. Flap coverage and skin grafting were then performed. (A) Preoperative photograph of patient. Infection signs were observed on the face, such as fever, pain, and pus-like discharge. (B) Resected scar tissue and foreign bodies observed during the operation. (C) Three-day postoperative photograph of patient. (D) Postoperative condition at 6 months. The inflammatory symptoms improved, but a facial contour deformity occurred due to scar formation after a wide excision was performed.
Of the 39 patients, 27 (69%) showed improved symptoms after only one operation. However, 12 patients (31%) required additional resection. Among them, nine (23%) underwent three or more operations and three (8%) underwent two operations (Fig. 7).
When comparing the period from the initial injection to hospitalization between the patient groups, the duration of time before hospitalization was found to be significantly longer for patients who received illegal treatment by unlicensed practitioners than for those who did not (P=0.016) (Table 1).
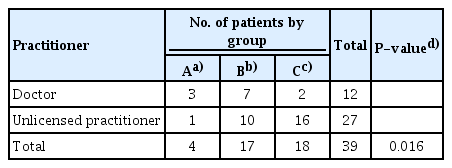
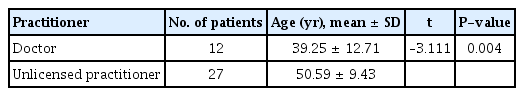
Period from injection of foreign materials to the first hospital visit according to practitioner type
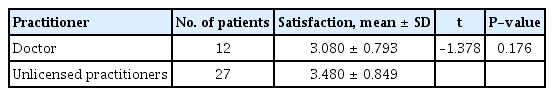
Patients who underwent procedures performed by unlicensed practitioners tended to be older at the time of presenting to the hospital (Table 2). The degree of satisfaction after surgery was significantly lower with the direct approach than with the indirect approach through a bypass incision (P=0.044) (Table 3). As the number of operations increased, the degree of satisfaction significantly decreased (Table 4). When comparing patient satisfaction based on the wound coverage method after surgical resection, the degree of satisfaction was significantly higher when primary closure was performed than when flap coverage and skin grafting were performed simultaneously (P<0.001) (Table 5). However, whether the surgeon was a licensed practitioner did not significantly affect the patient’s degree of satisfaction after surgery (P=0.176) (Table 6).
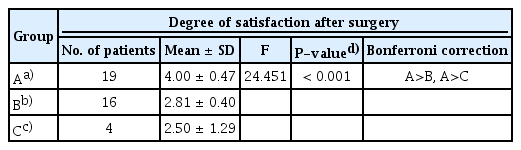
Degree of satisfaction after surgery according to the method of wound coverage after surgical resection
Postoperative satisfaction
Overall, 34 of the 39 patients (87%) completed the questionnaire. The average postoperative satisfaction score was 3.32±0.88.
Six patients (15%) were satisfied with the management of facial contouring deformities, 11 with foreign body sensation (28%), 17 with inflammation (44%), and none with “other.” Thus, the highest degree of satisfaction was observed with regard to inflammation. Conversely, 11 patients (28%) were dissatisfied with the management of facial contouring deformities, 20 (51%) with foreign body sensation, three (8%) with inflammation, and none with “other.” Thus, the highest degree of dissatisfaction was observed with regard to the management of foreign body sensation.
Progress
Of the 39 patients, four (10%) were outpatients with depressed scars at the surgical site and were treated with autologous fat grafts or filler injections (Fig. 8).
Depressed scars that occurred after surgical removal were treated with autologous fat grafts or filler injections. (A) Depressed scar on the left cheek area. (B) Improved facial contouring after fat grafting. (C) Depressed scar on the glabella. (D) Improved facial contouring after hyaluronic acid filler injection.
DISCUSSION
For most of the time during which they have been used, injections using foreign materials that have never been verified as safe for human use have been administered for cosmetic purposes and to treat body deformities, including those of the face. Soft tissue fillers are a simple and easy method for achieving pleasing cosmetic results compared to other methods [4,5]. Currently, many soft tissue fillers are marketed for human use. In general, these fillers fall into one of four major categories: autologous implants, collagens, hyaluronic acids, and biosynthetic polymers [3]. In the past, many illegal procedures have been undertaken due to a lack of awareness about soft tissue fillers. However, in recent years, foreign material injections undertaken at illegal centers have decreased. Nevertheless, many patients complain of discomfort caused by foreign bodies, as injected materials persist in the body and can cause various complications [6].
Complications caused by foreign material injections can be categorized based on the time at which they appear. Symptoms such as temporary swelling, bruising, and redness at the filler injection site that occur immediately after injection are common and self-limiting. However, other complications such as granulomatous reactions, tissue necrosis, and recurrent cellulitis are severe [4,7]. Granulomatous inflammatory reactions can occur several months to several decades after a procedure. In severe cases, a granulomatous reaction can cause the formation of nodules or cellulitis. There are no known factors to predict the occurrence of granulomatous reactions, and the mechanisms or courses of occurrence have yet to be clearly identified [4,5].
Unlike cases of foreign body granulomas caused by filler injections with known materials, conservative management may not be sufficient in cases of granulomas caused by injections with unknown materials. Therefore, surgical resection often must be performed after symptoms are managed with antibiotics and/or steroids if inflammation is suspected [3]. Among the patients included in this study, 39 underwent surgical resection.
There are concerns that sufficient resection in cases of severe symptoms caused by foreign materials may not be achieved if insufficient or bypass incisions are made to correct cosmetic aspects, such as to relax skin tension or beauty lines. Therefore, when there are areas with severe foreign body granulomas, sufficient removal of the skin and surrounding tissue of the granulomas is most effective for correcting contours and reducing inflammation [5].
In our study, among the 39 patients who visited the hospital with facial foreign bodies, 27 had received illegal injections, which was more than twice the number of patients who had received injections from a physician. Moreover, the period from the initial injection to hospitalization was significantly longer for patients who received illegal injections from unlicensed practitioners. Many cases of illegal treatment by unlicensed practitioners have been reported. A lack of awareness of possible side effects from these procedures and a lack of access to medical treatment may contribute to this phenomenon. Therefore, many patients treated by unlicensed practitioners may not have been aware of the injected material or the side effects that could occur after the procedure. Patients may have been unable to manage their symptoms in a timely manner due to their hesitation to visit a hospital because of the illegal nature of the injections. For this reason, many of these patients endured discomfort and visited the hospital only after the symptoms had increased in severity.
The areas where symptoms appeared on the face were divided into nine areas: the forehead, eyelid, temple, brow, eyebrow, nose, cheek, lips, and chin. There were 29 patients with a single symptom site and 10 patients with symptoms at two or more sites. When comparing the period from the onset of symptoms to the time of the hospital visit for each patient, we observed that a more complex symptom site corresponded to a shorter amount of time before visiting the hospital. In these cases, the patients visited a medical institution sooner since the discomfort from symptoms and their severity were found to increase with the number of sites.
Depending on the location and severity of symptoms at the time of surgical treatment, a surgical approach involving either a direct incision or bypass incision was chosen. In the postoperative questionnaire, the satisfaction scores from the postoperative questionnaire were compared according to the surgical approach. When the direct incision approach was used, the degree of satisfaction after surgery was lower than when the indirect approach through a bypass incision was used. When the symptoms caused by the injected foreign materials were more severe or wide, the skin and surrounding tissue of the granulomas needed to be removed through the direct approach, and postoperative scarring caused by this method may have lowered patient satisfaction. In addition, it is impossible to completely remove the foreign body if it penetrates the surrounding tissue. For this reason, reoperation was performed when the symptoms caused by a foreign body persisted or when the results were unsatisfactory even after surgical treatment. As the number of operations increased, the degree of satisfaction decreased.
If the defect was wider after resection, flap coverage and/or skin grafting had to be performed instead of primary closure, as the coverage method was chosen based on the severity of the wound after surgical resection. Postoperative satisfaction was confirmed to be lower when flap coverage and/or skin grafts were performed rather than simple sutures (Table 5). However, careful interpretation of the results is required, since the difference in satisfaction may still be caused by surgical complications, such as facial contour deformity, rather than simply differences in surgical methods.
If a patient who experiences complications due to the injection of foreign materials in the face requires treatment, the treatment period may last for a long time depending on the range or severity of their symptoms, and the symptoms may not improve after a single surgical treatment. Thus, an explanation must be provided to the patient so he or she can give consent before an operation.
This study highlights the importance of establishing suitable indications for determining surgical treatment. One suitable indication for surgical treatment may be the repeated failure of conservative treatment due to severe symptoms, such as deformation and inflammation, if the boundaries of the lesion site are relatively clear or if the patient reports psychological issues due to facial contour deformity or other severe symptoms.
Our study had several limitations, however. First, the results may be specific to this study, and general conclusions should be drawn with caution. This study cannot be generalized to a broader population due to the relatively small sample size and targeted patient group composed of patients who visited the authors’ hospital. Second, 34 out of 39 patients completed the satisfaction questionnaire, which may have caused non-response bias. In addition, this study was conducted to identify the characteristics of patients with various facial foreign body injections, evaluate their subjective satisfaction after surgery, and conduct a comparative statistical analysis. Therefore, objective evaluations based on surgical results could not be made. Therefore, additional studies are required to evaluate surgical success according to postoperative outcomes.
In recent years, the number of patients requiring simple procedures, such as filler injection, rather than cosmetic surgery has been increasing. However, the occurrence of complications, such as foreign body granuloma, has increased as foreign body injections have increased in popularity. Moreover, the number of complications such as granulomas has increased not just because of injections administered by unlicensed practitioners but also because of injections administered by licensed physicians. Depending on the severity of inflammatory symptoms, such as pain, contracture, fever, and tenderness, complications can be treated with medication, injection therapy, or surgical removal. Among these treatments, surgical removal is a more reliable method for improvement than medication and injections, but the treatment should be decided with caution given various factors such as the severity of symptoms, cosmetic factors, patient psychology, and other factors related to patient satisfaction. Patient satisfaction can be improved by reducing the number of operations and performing only the necessary incisions or excisions corresponding to the range of symptoms caused by foreign substances and by indirectly using bypass incisions to avoid scarring that may occur after surgery.
Additionally, awareness about the indiscriminate application of fillers in patients and an emphasis on the careful use of fillers by medical practitioners is required. This information will also help to raise awareness about treatments provided by unlicensed practitioners and suggest appropriate treatment strategies for foreign body granulomas.
Notes
No potential conflict of interest relevant to this article was reported.
Ethical approval
The study was approved by the Institutional Review Board of Chosun University Hospital (IRB No. 2020-12-033-002) and performed in accordance with the principles of the Declaration of Helsinki.
Patient consent
The patients provided written informed consent for the publication and use of their images.