A prospective comparison of prepectoral and subpectoral methods for immediate breast reconstruction with acellular dermal matrix: the cogwheel-shaped anterior wrapping method
Article information
Abstract
Background
Prepectoral breast reconstruction has recently gained wide recognition for its advantages, such as rapid recovery and less pain. This study compared the effectiveness of and differences between the prepectoral and subpectoral breast reconstruction techniques.
Methods
Eighty-three patients (90 breasts) who underwent prepectoral or subpectoral breast reconstruction surgery between January 2019 and December 2020 were prospectively recruited. Patient demographics, comorbidities, oncological treatment, and intraoperative and postoperative data were evaluated to investigate the validity and stability of each surgical technique. The follow-up period was a minimum of 18 months.
Results
The surgical cohorts (22 prepectoral and 68 subpectoral) had comparable demographics. No significant differences in postoperative complications were observed between the two groups. The prepectoral group showed shorter operation times than the subpectoral group (mean: 97.27 and 127.63 minutes, respectively; P<0.001). Fewer days elapsed until drain removal and the total amount of drainage was less in the prepectoral group than in the subpectoral group (mean: postoperative day [POD] 8.95 and 10.06, respectively; P=0.048) and (501.72 mL and 671.19 mL, respectively; P=0.009). The numeric pain rating scale (NPRS) scores at POD 7 were significantly lower in the prepectoral group than in the subpectoral group (mean: 0.41 and 1.82, respectively; P=0.029). There were no statistically significant differences in the NPRS scores at POD 1 or the BREAST-Q questionnaire scores at 3 months.
Conclusions
Prepectoral breast reconstruction using acellular dermal matrix can feasibly replace the conventional subpectoral breast reconstruction technique and has the advantages of reducing operation time, length of hospitalization, and long-term postoperative pain.
INTRODUCTION
The number of patients undergoing breast reconstruction surgery after mastectomy has gradually increased. According to the American Society of Plastic Surgery, the number of patients who underwent breast reconstruction increased from 78,832 in 2000 to 137,808 in 2020, a 75% increase [1]. Approximately 77% of these patients underwent immediate breast reconstruction after mastectomy, most with silicone implants (93%). Compared to a flap operation using autologous tissue, implant-based breast reconstruction has the advantage of a shorter surgical time, faster recovery, and less donor-site morbidity [2].
There have been many developments in the technique of breast reconstruction with implants. The initial approach was to insert the implant into the prepectoral pocket, directly under the mastectomy skin flap. However, the incidence of capsular contracture was high [3]. To compensate for this problem, a method was developed that dissected the pectoralis major muscle to cover the implant and position it in the subpectoral plane. If the implant could not be completely covered with the pectoralis muscle, delayed two-stage breast reconstruction was introduced, gradually inflating the subpectoral space using a tissue expander. However, this was uncomfortable for the patient and lacked the advantages of immediate breast reconstruction [4]. The dual-plane method was later developed, but over time developed an aesthetic defect (“bottoming out”) caused by excessive lower pole expansion.
With the introduction of the acellular dermal matrix (ADM) in the early 2000s, the modified dual-plane method became popular for securing an adequate submuscular pocket, while preventing bottoming out and enabling one-staged reconstruction [3,5]. However, this method inevitably damaged the pectoralis muscle, resulting in shoulder dysfunction and animation deformity [6]. Prepectoral breast reconstruction is a novel technique that avoids damage to the pectoralis muscle and fixes the muscle anteriorly using only ADM and an implant. The use of ADM technology has spread rapidly because of its proven biological stability, rapid host revascularization, and lack of adverse effects caused by damage to the pectoralis muscle.
A disadvantage of the prepectoral breast reconstruction technique is a higher incidence of rippling [7]. Moreover, research comparing the long-term outcomes of the prepectoral breast reconstruction and the subpectoral method is lacking, and there are few reviews of patient-reported outcomes. In this study, we hypothesized that postoperative pain in the prepectoral group would be less than that of the subpectoral group, and that the hospitalization periods needed to manage surgery site drainage would be shorter due to smaller amounts of drainage. Additionally, we discuss whether the prepectoral breast reconstruction method is safe and effective and should replace the subpectoral breast reconstruction method.
METHODS
Patients
This prospective cohort study was approved by the Institutional Review Board of Gachon University Gil Medical Center (No. GCI RB2019-085). The patients included in the study were prospectively recruited for direct-to-implant breast reconstruction from January 2019 to December 2020. The patients were randomly assigned to either the prepectoral or the subpectoral groups with written consent. The patients’ demographic details included age, body mass index, past medical history (hypertension, diabetes mellitus, and cardiac disease), smoking history, and treatment with radiotherapy and/or chemotherapy. Intraoperative comparisons were made, including the resection mass (g), implant size (mL), and operation time. To compare postoperative complication risks between the two groups, skin necrosis and infection were investigated (divided into minor and major). The presence or absence of red breast syndrome, seroma, hematoma, and capsular contracture was also investigated prospectively up to 18 months after surgery. In this study, minor skin necrosis was defined as partial-thickness skin necrosis that did not require surgical management, and major skin necrosis was defined as full-thickness skin necrosis requiring surgical management such as debridement and revision. A minor infection was defined as an infection or inflammation that could be managed with oral antibiotics, and a major infection was defined as an infection necessitating hospitalization for intravenous antibiotics. Patients were assessed for capsular contracture at 3 months and 18 months postoperatively. Factors related to the patients’ quality of life were compared, including drain removal day (postoperative day [POD]) and total drainage amounts, which were directly related to hospitalization duration. Furthermore, pain scores were assessed on POD 1 and POD 7 using the numeric pain rating scale (NPRS), and BREAST-Q scores were collected at 3 months postoperatively. Both scores were used to make comparisons between the two groups. Patients were provided with a patient-reported outcome questionnaire, the BREAST-Q version 2.0 Reconstruction Module (Memorial Sloan Kettering Cancer Center, New York, NY, USA). Patients who failed to answer more than half of the items within each domain were excluded from the analysis.
Surgical technique
All patients underwent breast reconstruction using a MemoryGel silicone implant (Mentor Corp., Santa Barbara, CA, USA), which was washed with triple irrigation (betadine, antibiotics, and normal saline) before insertion. Prepectoral implant insertion was performed by irrigating the ADM (16×16 cm; MegaDerm, L&C Bio, Seoul, Korea) with sterile 0.9% saline. After placing the selected sizer or implant on the tray and covering it with the ADM, the tab to be fixed was designed in a cogwheel shape and then cut using a sharp Metzenbaum scissor (Fig. 1A). On top of the pectoralis major muscle, the implant was covered anteriorly only with the ADM and fixed with Vicryl no. 3 at intervals of 5 cm on all sides (Fig. 1B). Subpectoral implant insertion was performed by dissecting the muscle, cutting the inferolateral border, and then creating a dual-plane pocket connecting the pectoralis fascia and the chest wall with ADM (8×16 cm; MegaDerm, L&C Bio). Similarly, the implant was fixed with Vicryl no. 3; one hemovac drain was mounted on the axillary side and another on the inframammary fold. For wound closure, the subcutaneous, subdermal, and skin layers were sutured with Vicryl no. 3, Surgifit no. 4, and nylon no. 5, respectively. A mild compressive dressing with an antibiotic ointment was applied.

Prepectoral acellular dermal matrix (ADM) coverage method (cogwheel-shaped anterior wrapping method). (A) The sizer or implant on the surgical tray was covered anteriorly by a cogwheel-shaped ADM (16×16 cm), which was designed using a gentian violet marker with 8 to 10 tabs to be fixed. This method could help reduce surgery time. (B) After inserting a predicted implant sizer, the ADM was sutured by Vicryl no. 3 except at the lateral margin. After replacing the sizer with an implant, the lateral border was fixed. It was successfully fixed without folding.
Statistical analysis
Statistical analysis was conducted using SPSS version 20.0 (IBM Corp., Armonk, NY, USA). Representative data were presented as the mean±standard deviation. A value of P<0.05 indicated statistical significance. The Kolmogorov-Smirnov test was used to verify the normality of the data, and the Mann-Whitney test was used for non-parametric tests. The Pearson chi-square test and the two-tailed Fisher exact test were used for cross-tabulation analysis comparing the demographics and postoperative complication rates of the two groups. The NPRS scores (0–10) were used to compare pain levels, and the BREAST-Q version 2.0 scores (35–143) were used to compare patient satisfaction with breasts, implants, outcomes, and psychosocial well-being. Other questionnaire items (e.g., sexual well-being, satisfaction with the information provided) were excluded because of poor response rates.
RESULTS
Cohort demographics
Ninety breasts and 83 patients were included in this study (Table 1). In the prepectoral group, 21 patients (22 breasts) underwent immediate prepectoral implant insertion, of whom one patient underwent bilateral reconstruction (Fig. 2). In the subpectoral group, 62 patients (68 breasts) were treated with the subpectoral implant insertion method, of whom six underwent bilateral reconstruction (Fig. 3). There were no statistically significant differences in age, body mass index, resected mass, and implant size between the two groups (P=0.554, P=0.101, P=0.662, and P=0.354, respectively). In addition, there were no significant differences in the proportion of patients with hypertension, diabetes mellitus, and cardiac disease between the two groups (P=0.955, P=0.728, and P=0.592, respectively). The proportion of patients with a history of smoking, postoperative radiotherapy, and chemotherapy did not differ significantly between the two groups (P=1.000, P=0.752, and P=0.218, respectively). Therefore, the two groups in this cohort study were considered comparable.
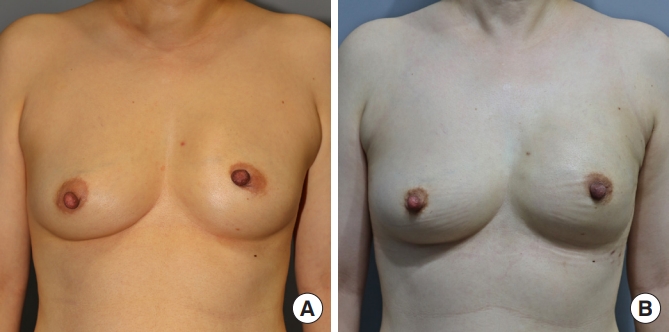
Preoperative and postoperative images of prepectoral breast reconstruction. (A) Preoperative image. (B) Image at 3 months postoperatively. Typical perioperative appearances of a patient that has undergone unilateral (left) mastectomy and reconstruction with prepectoral implants anteriorly covered with the cogwheel-shaped acellular dermal matrix.
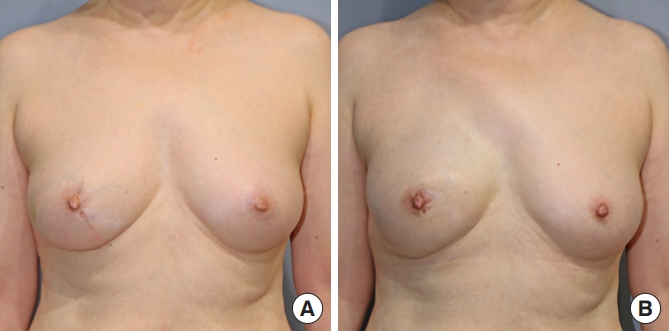
Preoperative and postoperative images of subpectoral breast reconstruction. (A) Preoperative image. (B) Image at 3 months postoperatively. Typical perioperative appearance of a patient that has undergone unilateral (right) mastectomy and reconstruction with subpectoral implants covered with dual-plane pectoralis major muscle and acellular dermal matrix.
Postoperative complications
One breast in the prepectoral group and 17 breasts in the subpectoral group had minor skin necrosis (partial-thickness necrosis) that did not require surgical management, and there was no significant difference between the two groups (P=0.062) (Table 2). One breast in the prepectoral group and 9 breasts in the subpectoral group had major skin necrosis (full-thickness necrosis) requiring surgical intervention, and there was no significant difference between the two groups (P=0.441). The number of breasts with minor infections not requiring hospitalization and treated with oral antibiotics included one in the prepectoral group and three in the subpectoral group, with no significant difference between the two groups (P=1.000). Furthermore, the proportion of patients with a major infection requiring intravenous antibiotics, red breast syndrome, seroma, hematoma, or capsular contracture showed no significant differences between the two groups (P=1.000); no such complications were found in the prepectoral group.
Quality of life
The quality of life for patients undergoing immediate breast reconstruction after mastectomy is determined by various factors. Operation time or, more specifically, the time during which the patient is under general anesthesia, is one such factor and is directly related to the rate of complications that may occur after a general anesthesia operation. In this study, the mean surgical time of the prepectoral group (97.27±25.62 minutes) was significantly less than that of the subpectoral group (127.63±24.67 minutes) (P<0.001) (Table 3). In addition, the drain removal date impacts how quickly most patients can return to their daily lives. The time to drain removal in the prepectoral group (POD, 8.95±2.59 days) was significantly shorter than that of the subpectoral group (POD, 10.06±2.73 days; P=0.048). The total amount of drainage was also significantly less in the prepectoral group (501.72±264.59 mL) than in the subpectoral group (671.19±298.00 mL; P=0.009). Furthermore, analysis of subjective postoperative pain as reported by the patients, based on NPRS scores, showed that there was no significant difference between the two groups (P=0.949) on POD 1. However, the pain score of the prepectoral group (0.41±1.05) on POD 7 was significantly lower than that of the subpectoral group (1.82±2.60; P=0.029). Finally, to evaluate the patients’ satisfaction with their surgery, the BREAST-Q scores were compared at 3 months postoperatively, and showed no significant difference between the prepectoral and subpectoral groups (mean, 105.00 vs. 113.94; P=0.218).
DISCUSSION
Recent studies have focused on the results of patient-reported outcomes to assess direct-to-implant prepectoral breast reconstruction. This is because new perspectives have emerged, according to which prepectoral breast reconstruction is less painful, has less capsular contracture, and has better aesthetic results [4,8,9], in addition to causing less injury to the pectoralis major muscle (a disadvantage of subpectoral breast reconstruction), which can lead to animation deformity and shoulder movement impediments. However, there is still no consensus on prepectoral breast reconstruction, owing to the lack of large-scale, multicenter research. Although no significant differences in complication rate or patient satisfaction were observed between the two groups in this prospective cohort study, the results are significant because they showed that the prepectoral technique can reduce surgery time, speed up discharge, and reduce long-term pain after surgery.
The prepectoral breast reconstruction technique saves the time and effort needed to dissect the pectoralis major muscle from the chest wall, and possibly prevents unnecessary bleeding caused by muscle bed damage, thus omitting the time needed to regain hemostasis and thereby shortening the surgery time. Shortened operation time is cost-effective and reduces the time of general anesthesia. A prolonged period of general anesthesia can adversely affect the respiratory and cardiovascular systems, as well as the liver and kidneys [10]. Although the risk varies depending on the patient’s age and underlying diseases, it is generally assumed that shorter general anesthesia time lessens the burden on the patient’s body immediately after surgery. Therefore, it can be interpreted that prepectoral breast reconstruction is simpler and less risky than subpectoral breast reconstruction.
In this study, prepectoral breast reconstruction was performed with the cogwheel-shaped anterior wrapping method rather than the full wrapping method. In most prepectoral breast reconstruction studies, the full wrapping method was described [11-13]. Although there are various shapes, sizes, and brands of ADM, most are flat and rectangular or square-shaped. To cover the entire prosthesis, cutting the ADM to fit the shape of the implant takes more time and increases the cost by using more ADM. In addition, when the full wrapping method is used, dead space may occur in the folded portion of the ADM. Moreover, if the suture tab is not made separately, slight damage to the implant may occur during the fixation process. There are still no studies that have shown statistically significant advantages to covering the posterior side of the implant with ADM. The cogwheel-shaped design facilitated suture tab fixation on the chest wall and reduced the surgical time. By creating a suture tab with the implant and ADM on the surgical tray, it could be fixed with predictable tension and minimize dead space (Fig. 1B).
In this study, the amount of drainage in the prepectoral group was less than that of the subpectoral group, which decreased the number of days before the drain could be removed and quickened the patient’s return to daily life. The differences in drainage amounts were likely due to the inevitable tissue damage caused by electrocautery heat during dissection of the pectoralis major muscle in the subpectoral group, and to the high risk of spontaneous bleeding as the deep layer of tissue was exposed [14]. A clinical study reported that the duration of drainage was determined by the volume of serous fluid, which was consistent with our results [15]. A shorter period of drainage can reduce the duration of antibiotic use, the risk of infection, and the length of hospitalization. Prepectoral breast reconstruction can be costly because it uses 1.5 to 2 times more ADM than the subpectoral technique. However, since the hospitalization period is shorter and the patient can resume economic activities sooner, some of that cost can be offset [16].
There is still disagreement about whether patients undergoing prepectoral reconstruction have less pain. One clinical study comparing the short-term outcomes between the two groups found no significant difference in pain levels because pain was primarily caused by the mastectomy [17]. Although there was no difference in our study between the two groups at POD 1, the difference between the two groups at POD 7 was significant. A possible reason for this was that most of the pain caused by the mastectomy dissipates approximately 7 days after surgery, and the pain and discomfort caused by injury to the pectoralis major muscle occurs slightly later or lasts longer [18,19]. In addition, several recent studies have shown consistent results for relatively less pain in prepectoral breast reconstruction [20].
With the recent emphasis on patient-centered clinical results, many studies have used BREAST-Q scores to categorize patient satisfaction after breast reconstruction [21]. Although there are studies emphasizing a better aesthetic outcome in the prepectoral group, there are also studies reporting the contrary [7,22,23]. In this study, there was no significant difference in patient satisfaction between the two groups. A suggested reason for this is that the patients viewed this as reconstructive surgery rather than cosmetic surgery, even though they are essentially the same procedure. When obtaining consent from the patients in our study, it was explained that this was reconstructive surgery, and not a cosmetic procedure, and that the purpose of the surgery was to construct a breast similar in size to the normal breast, rather than focusing on the appearance of the breast. Furthermore, because the scores were based on the patients’ self-reports, the results were subjective. Differences in scores would also be likely across hospitals, regions, and countries.
Capsular contracture is the most common long-term complication in direct-to-implant reconstruction [24,25]. A retrospective clinical study showed that the prepectoral technique was relatively more resistant to capsular contracture than subpectoral breast reconstruction in patients who had postmastectomy radiotherapy [9]. In this study, although there was no significant difference in the incidence of capsular contracture, we did not compare subgroups such as patients who received postmastectomy radiotherapy.
This study had several limitations. First, because it was designed to investigate a prospective cohort, the study period was short and there may be differences between the two groups in terms of complications or patient satisfaction that might have occurred over a longer timeframe. In addition, because the patients were grouped based on patient preference over a short period, it was difficult to more closely match the number of patients in the two groups, which may have resulted in a statistical error. Finally, many of the older adult patients grew up influenced by Confucian ideas and were uncomfortable answering many items in the BREAST-Q questionnaire such as questions about sexual well-being. Those patients could not be accurately evaluated and many patients were lost to follow-up after 3 months. We recommend future multicenter studies using standardized evaluation methods and long-term follow-up to verify results. In addition, collaboration with the department of rehabilitation medicine to objectively evaluate any complications that result in limited shoulder range of motion would be valuable to future research.
In conclusion, this study showed that prepectoral breast reconstruction using ADM could feasibly replace the conventional technique of subpectoral breast reconstruction and has the notable advantages of reduced operation time, hospitalization time, and long-term postoperative pain.
Notes
No potential conflict of interest relevant to this article was reported.
Ethical approval
The study was approved by the Institutional Review Board of Gachon University Gil Medical Center (IRB No. GCIRB2019-085) and performed in accordance with the principles of the Declaration of Helsinki.
Patient consent
The patients provided written informed consent for the publication and use of their images.



