|
 |
- Search
| Arch Aesthetic Plast Surg > Volume 22(1); 2016 > Article |
Abstract
Laser treatment for scars has improved over the past three decades. Autologous platelet-rich plasma (PRP) derived from whole blood is immunologically inert and contains a proper ratio of growth factors and cytokines. Here we describe the case of a 29-year-old female patient with a hypertrophic scar on her right shoulder caused by an operation performed in 2012. The patient underwent 11 laser therapy sessions with a fractional carbon dioxide (CO2) ablative laser system (LineXel) and two PRP injections. Her scar was evaluated with the Vancouver Scar Scale (VSS), and the baseline and post-treatment scores were 11 and 3, respectively. After treatment, the dimensions and volume of the scar were diminished, and contour, texture, and pigmentation had also improved compared to baseline. The patient reported less pain, swelling, and pigmentation following PRP combination ablative laser therapy. This case provides further evidence of the potential benefits of PRP as an adjuvant to fractional laser in reducing hypertrophic scars.
Scar formation following surgery or trauma is common, and some scars gradually become reddish, hard, or hypertrophic. Scars are classified as hypertrophic, keloid, atrophic, or acne scars. Hypertrophic scars are firm and protrude due to increased collagen expression, but unlike keloid scars they do not extend beyond the margin of the original wound [1].
Laser treatment for scars has improved over the past three decades and provides a less invasive, less painful treatment option [1]. The most recent cutaneous laser technique is fractional photothermolysis, which thermally alters a “fraction” of the skin, leaving untouched areas of normal skin that rapidly repopulate the ablated columns of tissue. To date, there are few studies regarding the effectiveness of ablative fractional carbon dioxide (CO2) laser for treating hypertrophic scars.
Platelets contain numerous granules and vast number of bioactive molecules that can facilitate homeostasis and wound healing. For these reasons, platelet-rich plasma (PRP) is increasingly being applied to clinical cases [1]. PRP is concentrated by centrifuging whole blood and then extracting a small volume of residual plasma. Autologous PRP is immunologically inert and contains the proper ratio of growth factors and cytokines [2]. Furthermore, additional equipment is not required to store PRP, and the processing cost is relatively low. Here we describe the outcomes of combining fractional CO2 laser therapy in combination with PRP to reduce a hypertrophic scar.
The patient was a 29-year-old female with a hypertrophic scar on her right shoulder from an orthopedic operation (open reduction and internal fixation of a humeral head fracture) performed in October 2012. Prior to the initial, the patient’s medical history was unremarkable. The patient’s scar was elevated and reddish. The length, width, and height were 15 cm, 1.8 cm, and 0.5 cm, respectively. The patient felt stiffness and irritation that felt like a stretching sensation on the operation site. She also experienced pain when moving shoulder.
We digitally photographed the hypertrophic scar beginning in December 2012. The patient has undergone 11 laser therapy sessions including two where PRP was injected immediately afterward. Each laser treatment was administered at regular interval monthly. In general, scars caused by operation or trauma are improved by laser resurfacing 6 to 8 weeks after injury because collagen is remodeled at that time [3]. Autologous PRP was injected into the scar in May and September 2012. PRP was injected after the fourth and eighth laser therapy sessions. After the PRP injection, an additional three laser therapies were performed progressively, with the final laser treatment administered in January 2014.
To extract PRP from whole blood, we used the SmartPReP system (Harvest Technologies, Plymouth, MA, USA). Prior to the procedure, we drew 54 mL whole blood from the patient and centrifuged the sample at 2,160 to 2,650 rpm for 14 minutes to yield 10 mL PRP [4]. Two-thirds of the plasma was platelet poor and was removed. The remaining one-third was mixed with a calcium chloride/thrombin mixture to activate the PRP, which was then injected into the patient’s scar.
The Vancouver Scar Scale (VSS) is widely used to score scars. This scale assesses pigmentation (0=normal, 1=hypopigmented, 2=mixed pigmentation, and 3=hyperpigmented), pliability (0=normal, 1=supple, 2=yielding, 3=firm, 4=ropes, and 5=contracture), height (0=flat, 1= <2 mm, 2=2–5 mm, 3= ≥5 mm), and vascularity (0=normal, 1=pink, 2=red, and 3=purple) [5]. The score of each parameter was measured, and total score is the sum of each score. We measured the pliability score and the height by observing clinical photographs and medical records.
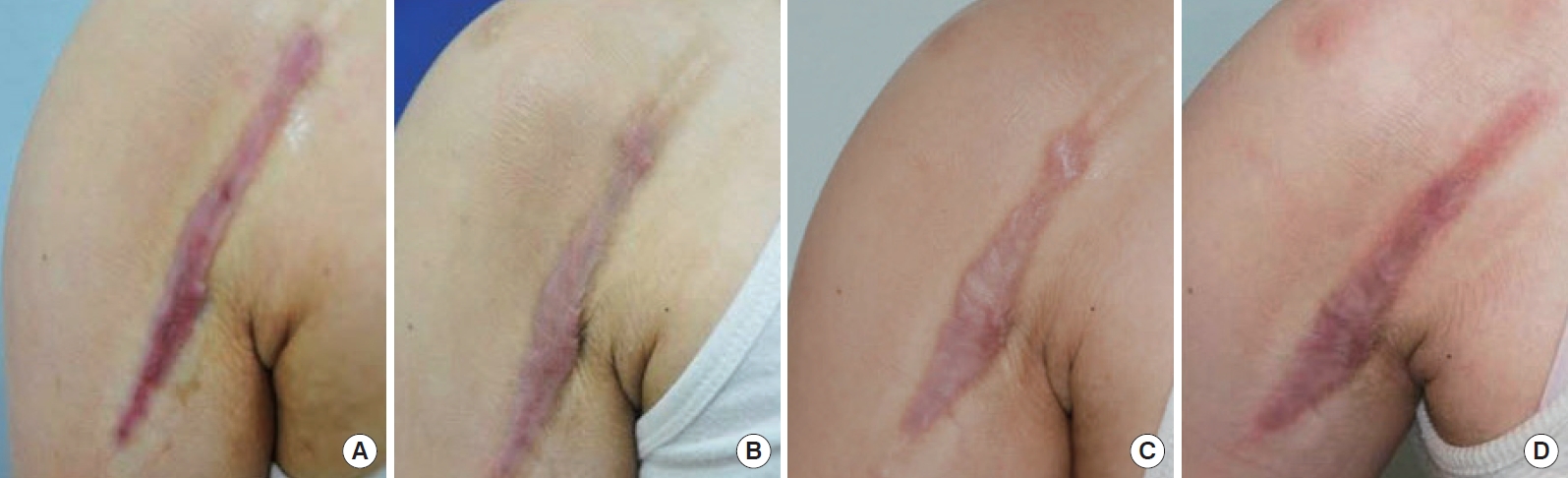
After two PRP injections, the pliability, pigmentation, and height of the scar were considerably improved. When comparing pre- with post-PRP photographs, we observed that PRP combination laser treatment resulted in better outcomes in pigmentation, vascularity, and pliability than laser treatment alone (Fig. 1 and 2). We also noted fewer side effects of ablative laser with PRP, including less erythema, edema, and postinflammatory hyperpigmentation. Moreover the total healing time was shorter for combination treatments than with ablative laser alone.
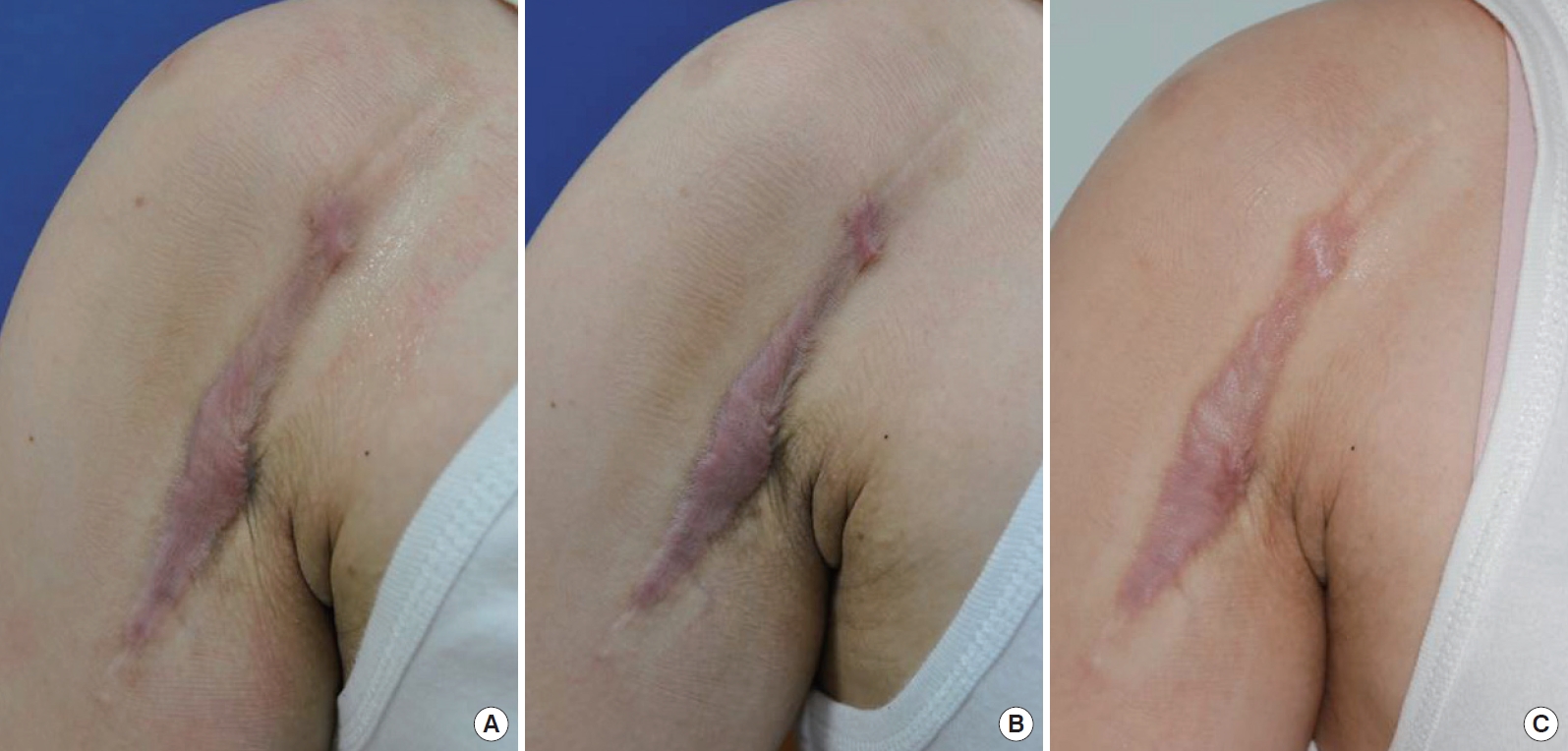
After 2 years, the length and width of the scar have shrunk even more. The scar volume has diminished, and texture and pigmentation have also improved compared to baseline (Fig. 3). Although irritation on the cutaneous scar has not completely resolved, the patient’s satisfaction regarding scar treatment is increased. Side effects such as wound disruption, ulceration, and dyspigmentation have not been reported.
The VSS score was 11 (pigmentation 3, pliability 4, height 2, vascularity 2) before treatment and had decreased to 3 (pigmentation 2, pliability 0, height 0, vascularity 1) after the final treatment. The patient was objectively and subjectively satisfied with the results.
Scar treatment has evolved over time. In the past, surgical excision was the most common treatment for hypertrophic scars, but more than half of these cases relapsed. Furthermore, this invasive procedure was unpleasant and painful.
Fractional ablative CO2 laser improves rhytides, dyschromia, and textural irregularities and inhibits early stage scar progression. In addition, it was recently reported that ablative fractional CO2 laser can resurface mature burn scars to correct abnormal texture, thickness, and stiffness [6]. Compared to the previous ablative resurfacing technique, this procedure is less invasive and allows more rapid recovery.
Ablative CO2 laser devices deliver more intense power to the scar tissue than non-ablative fractionated devices. It can ablate both the epidermis and dermis with significant heating of the adjacent dermal collagen. These thermal alterations change the collagen’s helical structure [7]. Swelling, erythema, and other significant adverse effects can limit ablative laser use. While non-ablative lasers have described as safer, the outcomes can be unsatisfactory, and the total treatment takes longer [5]. Compared to non-ablative fractional laser devices, ablative fractional CO2 laser resurfacing can leave tiny holes made by tissue vaporization and tighten adjacent tissue by collapsing the small vaporized columns [8]. These holes made with a fractional CO2 ablative laser can also be used as a PRP delivery route. The fractional laser technique characteristically spares the tissue surrounding each column, facilitating rapid epidermal regeneration [9]. Mechanistically, this is thought to be due to the rapid migration of viable keratinocyte present at the peripheral wound edges [10,11]. It induces collagen regeneration and remodeling in the dermal layer while epidermal stems cells in surrounding residual skin islands proliferate until the wound is healed. As a result, treatment with fractional CO2 lasers minimizes patient inconvenience and post-treatment complications. It also improves scar contour and patient tolerability compared to previous ablative CO2 and Er:YAG lasers. The LineXel fractional CO2 laser (UTI Co., Ltd, Seoul, Korea) was used for all 11 laser treatments. In this case, we used an average pulse duration of 500 ms in the central area of wound and 200 to 250 ms in the marginal area (maximum duration: 1,400 ms), with a distance of 0.8 to 0.9 mm [12].
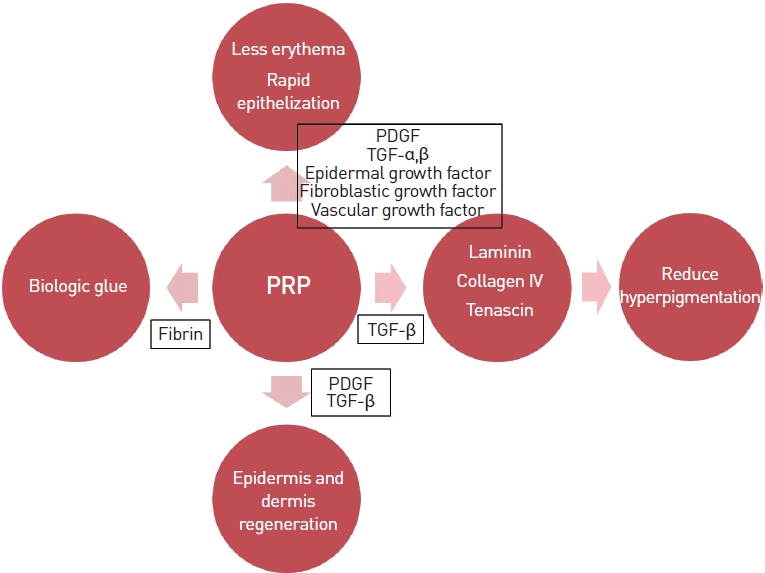
PRP has been reported to aid the healing of different tissues, likely due to the number of bioactive molecules released and the stimulation of cell proliferation. Activated platelets secrete intracellular granules that contain platelet-derived growth factor (PDGF), transforming growth factor alpha (TGF-α) and beta (TGF-β), epidermal growth factor, basic fibroblastic growth factor, and vascular endothelial growth factor. These factors are known to regulate processes including cell migration, attachment, proliferation, and differentiation [9]. They stimulate epidermal cell proliferation, promote angiogenesis, and induce collagen synthesis, all of which decrease erythema. Platelets have various molecules related to angiogenesis and vascular modeling. PRP seems to induce the appropriate level of angiogenesis without causing unnecessary vessel formation. PRP also reduces transient pigmentation caused when the fractional laser destroys the basal cell layer. TGF-β in PRP is known to stimulate the secretion of basement membrane proteins such as laminin, collagen IV, and tenascin. Those molecules can hasten repair of the basement membrane and might reduce post-inflammatory hyperpigmentation, resulting in less pigmentation. Also, thicker collagen bundles were observed in specimens from the PRP-treated side [10]. This enhanced collagen tissue facilitates the remodeling effect of PRP. PDGF is a potent mitogen of mesenchymal stem cells. PDGF and TGF-β in PRP also promote the synthesis of collagen and other extracellular matrix proteins, which helps regenerate the epidermis and dermis damaged by ablative laser treatment. Finally, activated PRP becomes a gel-like material containing fibrin, which can be used as biologic glue [10]. All these reactions are depicted in Fig. 4. According to a previous study on PRP, it is effective and safe treatment for atrophic scars with short downtime and good tolerability [11]. Based on the findings in that report, we hypothesized that the laser/PRP combination therapy could be applied to hypertrophic scars. Indeed, the patient reported less pain, swelling, edema, erythema, and pigmentation and a shorter epithelization period.
The shoulder is the joint most frequently affected by trauma or burn injury, and this can lead to significant functional limitations [13]. As we did not expect spontaneous resolution in this patient, laser management was performed to prevent functional loss.
Our study has two limitations. First, the photographer did not take pictures with the same light brightness at the same location, so result interpretation is subjective. Second, there was no decrease in irritation, and the length and width of the scar did not change. To clarify the clinical outcome and the mechanism of synergistic effects, additional studies using PRP injection and fractional CO2 laser should be performed.
In summary, the volume, contour, and pigmentation of the scar improved after combined therapy with 1 PRP injections and 11 fractional CO2 laser treatments. This case provides evidence of the potential benefits of using PRP as an adjuvant to fractional laser in the treatment of hypertrophic scars. The superiority of the combination was clearly evident in several aspects, including the rapidity and degree of scar improvement, fewer side effects, and shorter downtime.
Fig. 1.
Pre- and post-platelet-rich plasma (PRP) injection photographic findings of 1st PRP injection. (A) is 3rd laser treatment, (B) is 4th laser treatment (Just before 1st PRP injection) and (C) is 5th laser treatment (Next follow up time after 1st PRP injection).

Fig. 2.
Pre- and post-platelet-rich plasma (PRP) injection photographic findings of 2nd PRP injection. (A) is 7th laser treatment, (B) is 8th laser treatment (Just before 2nd PRP injection) and (C) is 9th laser treatment (Next follow up time after 2nd PRP injection).
REFERENCES
1. Khatri KA, Mahoney DL, McCartney MJ. Laser scar revision: a review. J Cosmet Laser Ther 2011;13:54-62.


2. Scrimali L, Lomeo G, Nolfo C, et al. Treatment of hypertrophic scars and keloids with a fractional CO2 laser: a personal experience. J Cosmet Laser Ther 2010;12:218-21.


3. Longo C, Galimberti M, De Pace B, et al. Laser skin rejuvenation: epidermal changes and collagen remodeling evaluated by in vivo confocal microscopy. Lasers Med Sci 2013;28:769-76.


4. Barrett SL. A new approach to using growth factors in wound healing. Podiatry Today 2003;16:44-50.
5. Hong SC, Park ES, Kim YB, et al. Effects of minimizing scar formation by early fractional CO2 laser resurfacing. Arch Aesthetic Plast Surg 2014;20:109-13.

6. Hultman CS, Edkins RE, Wu C, et al. Prospective, before-after cohort study to assess the efficacy of laser therapy on hypertrophic burn scars. Ann Plast Surg 2013;70:521-6.


7. Hantash BM, Bedi VP, Chan KF, et al. Ex vivo histological characterization of a novel ablative fractional resurfacing device. Lasers Surg Med 2007;39:87-95.


8. Hantash BM, Bedi VP, Kapadia B, et al. In vivo histological evaluation of a novel ablative fractional resurfacing device. Lasers Surg Med 2007;39:96-107.


9. Lee JW, Kim BJ, Kim MN, et al. The efficacy of autologous platelet rich plasma combined with ablative carbon dioxide fractional resurfacing for acne scars: a simultaneous split-face trial. Dermatol Surg 2011;37:931-8.


10. Na JI, Choi JW, Choi HR, et al. Rapid healing and reduced erythema after ablative fractional carbon dioxide laser resurfacing combined with the application of autologous platelet-rich plasma. Dermatol Surg 2011;37:463-8.


11. Gawdat HI, Hegazy RA, Fawzy MM, et al. Autologous platelet rich plasma: topical versus intradermal after fractional ablative carbon dioxide laser treatment of atrophic acne scars. Dermatol Surg 2014;40:152-61.


-
METRICS

-
- 2 Crossref
- 3,979 View
- 69 Download
- Related articles in AAPS