Efficacy of a long-pulsed 1064-nm Nd:YAG laser in acute scar redness
Article information
Abstract
Background
The initial redness of the scar on a postoperative suture site is a natural phenomenon that fades over time. However, with a long period of redness, patients complain about cosmetic discomfort, and the possibility of pigmentation changes is induced. We investigated the use of a long-pulsed 1064 nm Nd:YAG laser as a noninvasive treatment for improving the redness of these scars.
Methods
A retrospective chart review was conducted on 36 patients who underwent excision of a nevus on the face. Fourteen patients received laser treatment and another 22 patients used only scar management ointment. Patients were followed up 1 week after the sutures were removed. The photographic images taken at the time of suture removal and 2 months later were reviewed. The evaluation was performed on a 7-point scale by adding the Japan Scar Workshop (JSW) scar scale’s redness and erythema scores.
Results
The average initial JSW scar scale score of the treatment group was 4.6, and that of the nontreatment group was 4.2. When the re-evaluation was performed 2 months later, the score of the treatment group decreased to 2.2 and that of the nontreatment group decreased to 3.1. The difference in the JSW scar scale between the treatment group and the nontreatment group according to laser performance was statistically significant (P=0.03).
Conclusions
The treatment method with a long-pulsed 1064 nm Nd:YAG laser that is less invasive and has a quick effect can be a good alternative for improving this initial scar redness.
INTRODUCTION
During the scar maturation process in wound healing, acute redness of the scar area is observed in wounds [1]. In general, the redness can be caused by the inflammatory response, blood vessel vasodilation, or an increase in permeability. The characteristic of the early period of a wound with redness is that neutrophils, activated macrophages, and T lymphocytes accumulate in the wound to secrete matrix metalloproteinases and specific cytokines, which include the transforming growth factor family. Macrophages and lymphocytes remain in the wound for approximately 7 days from the early inflammatory period and then decrease in number. After that, re-epithelization and revascularization begin over a period of 2 to 4 weeks. In this process, myofibroblast-mediated contraction and collagen synthesis can occur, which can worsen the redness [1-3].
According to studies, it takes an average of approximately 7 months from the occurrence of redness to improvement and for the lesion’s gross appearance to fade [1]. As interest in appearance and beauty increases, there is a growing demand when using treatments to pay more attention to details even if these treatments cost more. Increasingly, an increasing number of patients are not satisfied with the 6-month or longer follow-up results in the alleviation of the redness. Accordingly, a study was conducted on a method for faster improvement of scar redness. It was thought that it could be helpful to apply a laser using a wavelength of 1064 nm, which is noninvasive but easily accessible to patients and helps recover the skin layer with a short recovery period [3]. A long-pulsed 1064 nm Nd:YAG laser is nonablative and is known to be a safe and effective laser technique commonly used in skin rejuvenation by inducing heating of the skin [3].
In general, for scarring, an ablative fractural laser mainly with a medium of CO2 or erbium is commonly used, and in some cases, a pulsed-dye laser (PDL) of 595 nm is used [4]. A long-pulsed 1064 nm Nd:YAG laser is not commonly used for acute scars. For this reason, there has been no research on the improvement of the redness of the initial scar using a long-pulsed 1064 nm Nd:YAG laser. In this study, through the analysis of the process of change in early scars, the effectiveness of a long-pulsed 1064 nm Nd:YAG laser was studied.
METHODS
From March 2021 to March 2022, a retrospective chart review was conducted on 36 patients who underwent surgical excision of a nevus on the facial area. Of the 36 patients, 14 underwent laser treatment after surgery, and the remaining 22 did not undergo laser treatment. Patient data were obtained while following a protocol approved by the Inje University Ilsan Paik Hospital (IRB No. 2023-02-021).
A single surgeon (CHK) performed the surgeries and laser treatments at the same institution, and a study was conducted on patients who underwent primary closure after nevus excision. An elliptical skin excision was made during surgery, and linear line scars occurred.
With the inclusion criteria, only patients aged 19 or older and under 69 years old were included, and the location of the nevus included the forehead, cheek, nose, philtrum, chin, and other areas. The patients with a linear scar with a size of 1 cm or more and a size less than 5 cm were included. Patients who underwent surgical excision of multiple nevi were excluded from the chart review.
A group of 14 patients who received laser treatment was followed up 1 week after the sutures were removed, and three stacked shots were performed with parameters of 7.0 J, 8 mm spot, 8 Hz, and 0.3 ms using a long-pulsed 1064 nm Nd:YAG laser (Clarity laser, Lutronic) applied to the redness area near the linear suture line as the target area. The laser energy parameters used as above are commonly referred to as the “Genesis technique,” which is mainly used in skin rejuvenation. It was performed without anesthesia or skin cooling, and four procedures were performed every 2 weeks. Except on the day of the procedure, scar management ointment containing cyclopentasiloxane was used during the follow-up period. This group of 14 patients was named the treatment group. The remaining 22 patients without laser treatment used only scar management ointment. The group of 22 patients was named the nontreatment group.
The data were analyzed according to sex, age, Fitzpatrick skin type, location of the scar, and postoperative scar size. The photographic images taken at the time of suture removal and 2 months later were reviewed. The evaluation was performed on a 7-point scale of 0 to 6 points by adding the Japan Scar Workshop (JSW) scar scale’s redness (0: non, 1: weak, 2: mild, 3: strong) and erythema (0: non, 1: weak, 2: mild, 3: strong) scores.
Statistical analysis
A Mann-Whitney U test was performed on the JSW scar scale before and after the procedure in the two patient groups. In order to analyze the relationship between the difference value of the JSW scar scale and age, skin type, and scar size before and after the procedure, Spearman rank correlation coefficient was calculated and significance tested. And the relationship between sex and scar location was analyzed using the chi-square test. Statistical analysis was performed using SPSS ver.26.0 (IBM Corp.). A P-value < 0.05 was considered significant.
RESULTS
The patients’ ages ranged from 19 to 69 years old (mean: 38.5 years), 19.4% of the patients were males (n = 7) and 80.6% of the patients were females (n = 29). The Fitzpatrick skin type was 10 for type 2, 22 for type 3, and four for type 4. Scar locations were cheek (n = 13), philtrum (n = 7), chin (n = 7), forehead (n = 4), and nose (n = 5). The average scar size was 2.9 cm (Table 1).
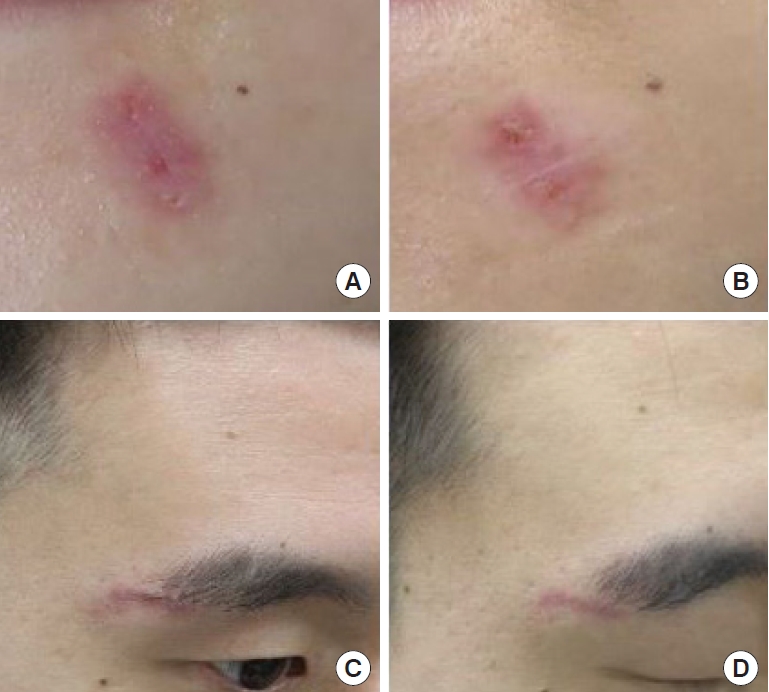
The average initial JSW scar scale score of the treatment group was 4.6, and that of the nontreatment group was 4.2. When the re-evaluation was performed 2 months later, the score of the treatment group decreased to 2.2 and that of the nontreatment group to 3.1 (Fig. 1). Even in the picture, the treatment group showed a significant improvement in redness 2 months later (Fig. 2). No other side effects occurred during the follow-up period, and there were no patients who had increased scores.

The Japan Scar Workshop (JSW) scar scale scores of the treatment and nontreatment groups at baseline and 2 months later (P=0.03).

Photographs of the treatment group. (A, C, E) Initial photos of the treatment group after suture removal. (B, D, F) Photographs of the treatment group at 2 months after three laser treatments.
The difference in the JSW scar scale between the treatment group and the nontreatment group according to the laser performance was statistically significant (P = 0.042). There was no significant difference in the JSW scar scale between age (P = 0.378), skin type (P = 0.160), scar size (P = 0.288), sex (P = 0.579), and scar location (P = 0.210).
DISCUSSION
Wound healing goes through three interrelated phases that overlap in time [1]. Based on the morphological differences in the wound tissue during healing, these three phases are defined as inflammation, proliferation (with granulation tissue development) and reepithelialization, and the remodeling phase, including maturation and remodeling of the scar. Scar formation is the third stage of the wound healing process, and during this phase, granulation tissue is remodeled progressively. At this stage, cellular structures are reduced through apoptosis. Decreased cellularity, especially between 3 and 8 weeks after injury, leads to flattening of the scar and resolution of the initial redness [2-4]. Collagen remodeling of scar formation, in which thicker fibers replace the haphazard array of fine fibers and align themselves parallel to the lines of skin tension, takes at least 6 months. Early scars show histologically diffuse capillaries and abnormally excessive arranged collagen fibers, which appear as redness of scars; late scars show vascular occlusion and excessive fiber deposition; and, therefore, the scars show normal or faded color with eminence, flattened or atrophy in morphology [5]. Redness is observed immediately after all types of injuries, including surgery, trauma, and burns. It is unclear when normal scar redness subsides, but some clinical observations suggest that it may take from 3 months to a year or more [2-4]. In one study, the majority of scars disappeared at or approximately 7 months after injury [6]. It has been suggested that redness after the first month of wounding is related to the total number of blood vessels and not due to ongoing inflammation or infection in the scar. The comparatively normal size of the vessels within the scar suggests that this is not the consequence of exceptional vasomotor tone of the vessel wall [6,7]. The conventional clinical treatments for scar tissue erythema primarily include anti-inflammatory and antiproliferative agents such as topical glucocorticoids and compression methods. Other topical anti-inflammatory treatments, such as silicone gel sheets that increase the elasticity scar tissue caused by burns, have also shown to result in reduced erythema, pruritus, and scar thickness [8].
Recently, interest in scar management has increased significantly as patients’ concerns about beauty and appearance have increased. As the global scar treatment market size is expected to reach approximately $32 billion by 2027, perceptions of the aesthetic impact of scars have changed, with patients wanting aggressive scar treatment in the early stages [9]. Laser therapy is one of the most commonly used methods to treat scar erythema due to its effectiveness and minimal invasiveness [10]. Various types of laser treatments are currently used for scar treatment, including fractional lasers, PDL, and Q-switched Nd:YAG lasers. Fractional lasers create columns of vaporized tissue along with encircling eschar and coagulated tissue, which can improve various characteristics of burn scars, including erythema. Kawecki et al. [11] found that 31% of patients with hypertrophic burn scars showed improvement of erythema tone after ablative fractional laser treatment. The PDL uses 595 nm wavelengths at which microvessels are coagulated (without damaging epidermal structures) by selective photothermolysis. PDL reduces inflammation and edema in scars with erythema and has shown satisfactory results in color restoration.
In contrast, the 1064 nm Nd:YAG laser penetrates deeper than the PDL. Consequently, it is increasingly used to treat hypertrophic scars and keloids [12]. It suppresses dilation of blood vessels and neovascularization. The inhibitory effect of a 1064 nm Nd:YAG laser on dermal collagen formation has been described in the literature [13]. A Q-switched Nd:YAG laser with a 1064 nm wavelength through very short pulses is a promising solution for reducing superficial angiogenesis and the prominence of vessels in postinflammatory erythema [14]. Q-switched Nd:YAG lasers with low fluence have produced helpful changes in photoaged skin and can induce unwanted fibrosis in the papillary dermis [15]. To circumvent this, the “Genesis technique,” which uses a Nd:YAG laser with quasi longpulse or micropulse mode, using pulse widths in the microsecond range, may be the treatment of choice to complement laser toning. It has the advantages of skin rejuvenation utilizing multipass lasers and short patient downtime [16]. The Nd:YAG laser can be used in the noncontact mode (this method is named Genesis) and contact mode. The contact mode is believed to penetrate to a depth that is twice the depth of Genesis [17]. Additionally, Genesis is less painful than the contact mode [18]. The Genesis technique minimizes downtime and erythema, maximizes skin rejuvenation effects and is reported to result in increased neocollagen formation and dermal remodeling and prolonged angiogenesis [19]. The long-pulsed 1064 nm Nd:YAG laser can treat keloids and hypertrophic scars effectively as it reduces vascularity. This decreased vascularity reduces the levels of cytokines and growth factors in the tissue and promotes the deposition of collagen. Thus, a long-pulsed 1064 nm Nd:YAG laser (non-Q-switched) was used for the treatment of vascular diseases involving inflammatory scars that show neovascularization [12]. According to the comparison of the JSW scar scale score that was used in this study, there was a statistically significant result in redness improvement with or without the use of a longpulsed 1064 nm Nd:YAG laser (Genesis technique). The redness observed in the early stage of scar formation after suture removal is usually observed within 2 weeks. Based on the above, it is highly likely that the inflammatory reaction by cytokines remains or that the color of hemoglobin due to neovascularization is projected onto the skin. Because the dermal layer is penetrated when using the long-pulsed 1064 nm Nd:YAG laser (Genesis technique), this technique accelerates the transition to the wound healing phase where collagen production occurs. Additionally, as is well known, appropriate heat energy penetrates to a sufficient depth of the dermis when using the long-pulsed laser, which helps dermal remodeling and vascularity, and these effects are thought to help recover the skin color more quickly. In addition, when compared with existing scar lasers such as PDL, there may be a disadvantage in that the procedure time is longer because the number of laser shots is relatively increased. However, it is almost painless in comparison and can be started at an earlier postoperative period than other lasers. The main mechanism of PDL is selective photothermolysis. It generates heat that damages the blood vessels, leading to their coagulation and subsequent closure. By targeting the blood vessels within the scar tissue, PDL helps to reduce the redness and vascularity associated with scars [18]. Compared to PDL, the Genesis technique of Nd:YAG laser is different in that heat is used for the purpose of providing appropriate stimulation necessary for recovery, rather than causing damage to tissues or blood vessels [12].
A limitation of this study is that by limiting the patient group, additional research on the utilization of the research effect on the redness of scars that occur after a wide scratch wound may be required. In addition, there is a possibility that some bias may exist in the research using retrospective chart review.
It is clear that the number of patients who want active treatment for certain symptoms rather than simply having follow-up time is increasing according to recent changes in aesthetic interest and trends. Therefore, the use of a laser can be a good option, and there has been no study that applied a long-pulsed 1064 nm Nd:YAG laser (Genesis technique) to initial scar redness. In this study, the laser and its parameters, which were partially used only for skin rejuvenation and pigmentation treatment, were used. As a result of systematic analysis, these parameters are helpful in improving scar redness, and the recovery is fast (Figs. 2, 3). The treatment method, which has evidence in being less invasive and having a quick effect, can be a good alternative for improving this initial scar redness.
Notes
No potential conflict of interest relevant to this article was reported.
Ethical approval
The study was approved by the the Inje University Ilsan Paik Hospital (IRB No. 2023-02-021) and performed in accordance with the principles of the Declaration of Helsinki.
Patient consent
The patients provided written informed consent for the publication and use of their images.