Scar folding for the treatment of nostril stenosis after open rhinoplasty: a case report
Article information
Abstract
A 25-year-old woman was referred for discomfort when breathing through her left nose. The patient had undergone augmentation rhinoplasty 5 years ago, after which hypertrophic scarring occurred in the left nostril. Several corticosteroid injections were administered as the first line of treatment, but with no symptom improvement. Therefore, we proceeded with surgical scar removal, with the use of a nasal conformer. However, scarring in the left nostril recurred. Accordingly, we proceeded with further surgical treatment using the scar folding technique. After scar folding, neither scarring nor nostril stenosis recurred during 1 year of postoperative follow-up. To summarize, herein, we report a case of hypertrophic scarring in the nostril that was successfully treated with the scar folding technique.
INTRODUCTION
Complications after rhinoplasty can result from hemorrhagic, infectious, traumatic, functional, and esthetic causes [1]. Scarring is another complication after open rhinoplasty, and the columellar incision is the most common site of scarring [2]. However, scarring at the inter-cartilaginous incision site is relatively rare, and deformation of the nostril is the most common related complication. Herein, we describe a case of mucosal hypertrophic scarring (HTS) that resulted in stenosis and blockage of the left nostril and was treated using the scar-folding technique, with good surgical results.
CASE REPORT
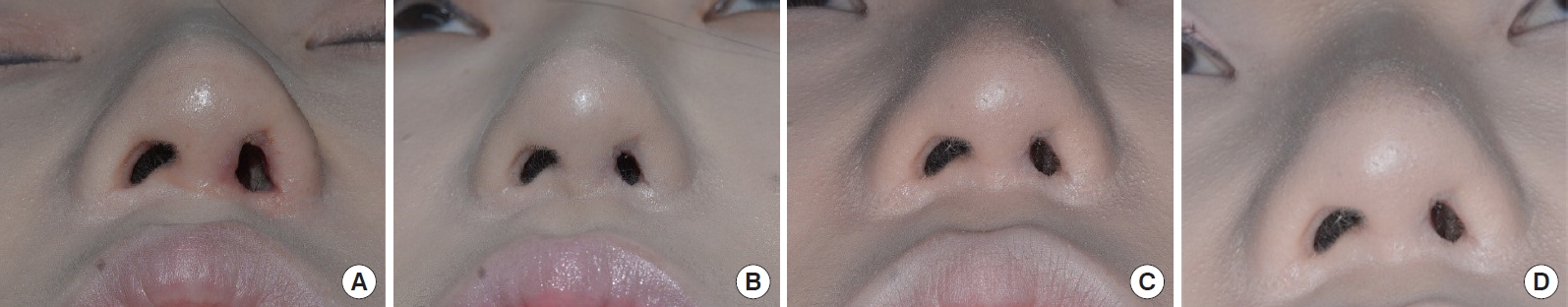
A 25-year-old woman was admitted to our hospital with a chief complaint of breathing discomfort due to stenosis of the left nostril after open rhinoplasty (Fig. 1). Five years prior, the patient had undergone augmentation rhinoplasty, tip plasty, and alar base reduction, using silicone implants. The patient’s past medical history was unremarkable. HTS in the left nostril was observed, with no significant scarring of the columellar incision. Several corticosteroid injections were administered as the first line of treatment, but with no symptom improvement. We then proceeded with surgical scar removal, using a nasal conformer. However, scarring in the left nostril recurred. Accordingly, we proceeded with further surgical treatment using the scar folding technique, as described below. On facial computed tomography, a silicone implant in the nasal dorsum and traces of tip plasty were observed, but with no exposure of the implant and no signs of inflammation. After local anesthesia, incisions were made at the 11 o’clock and 5 o’clock positions of the scar in the left nostril. The posterior portion of the scar was removed and folded back to close the raw surface created, which was sutured using 5/0 Vicryl. To compress the surgical site, Vaseline gauze was applied to the inner mucosa and outer skin of the left nostril and sutured using 4/0 nylon (Fig. 2). The nylon suture was removed at postoperative week 1 to prevent the recurrence of HTS. A silicone sheet was folded and placed inside the nostril to maintain the opening of the nostril. Three corticosteroid injections were administered at intervals of 3 to 4 weeks. At a 1-year follow-up, there was no recurrence of scarring, and the shape of the nostril was well maintained (Fig. 3).
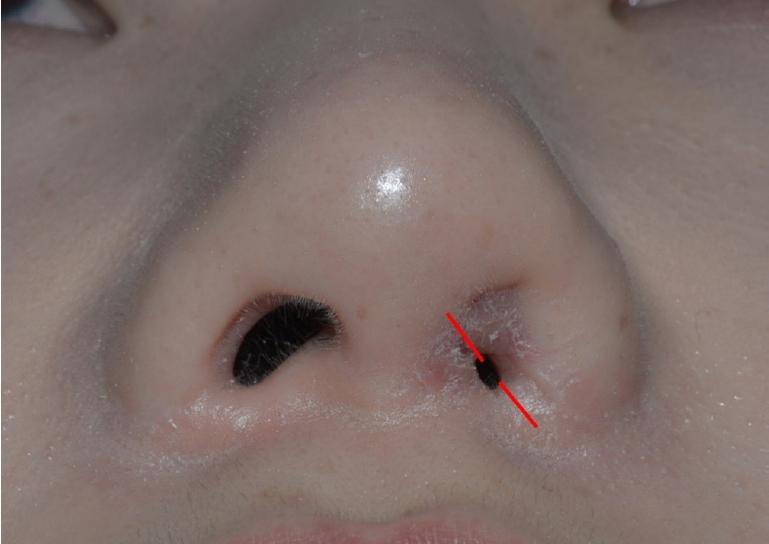
Preoperative photograph. The skin over the left nostril was thickened, with 93.7% stenosis of the left nostril, compared to the right side, due to scarring. Overgrowth of the inter-cartilaginous incision scar was also observed on the right side. Scarring from alar base reduction was also observed (red line, incision line).

Schematic representation of the scar folding method. (A) Removal of the posterior part of the scar, (B) folding of the remaining scar tissue to close the raw surface.
DISCUSSION
Esthetic rhinoplasty was initially performed using a closed technique or intranasal incision [2]. Since then, different open approaches using external incisions have been developed and described [3]. Scarring is a cause of complications after open rhinoplasty, and the columellar incision is the most common site. Various incision types and locations have been introduced to make scarring less visible [4]. In patients with a cleft palate, deformation of the nostrils may occur after rhinoplasty due to insufficient tissue or scarring [5]. A case of severe nostril stenosis after repeated rhinoplasty has been reported; that case was treated using a skin graft [6]. However, there has been no previous report of post-rhinoplasty nostril stenosis in the absence of alar deformation.
In the case presented herein, we used the scar folding technique, which involved removing the posterior aspect of the scar and subsequently folding back the tissue to close the raw surface created. Different surgical techniques reusing scars to improve symptoms have been described. Among these, a representative method is to reinforce the volume of the tissue by folding an existing scar into a depressed scar [7]. In our approach, the aim was to prevent recurrence of nostril stenosis; therefore, a substantial proportion of the scar was removed, the remaining scar was folded onto the raw surface created, and suturing was performed. Skin graft after removing the entire scar may be another surgical option. However, we thought that this would pose a high risk of recurrence of nostril stenosis, and the patient did not want a skin graft procedure.
The pathogenesis of HTS and keloid formation is not completely understood [8]. Mechanical force, infection, and genetic predisposition have been identified as possible causes of HTS and keloid formation [9]. The role of inflammation in modulating collagen synthesis has been described, and the intensity of inflammation has been shown to be positively correlated with the extent of scarring [8]. In our case, no evidence of inflammation on the inside of the nose was observed during surgery, with neither exudate nor exposure of the implant. Therefore, we did not proceed with re-incision and the implant was not removed. As healing progressed, the shape of the left nostril changed to a slightly more vertical shape than initially intended. To correct this issue and to ensure that the shape of the left nostril was similar to that of the right nostril, we used incisions at 11 o’clock and 5 o’clock for the scar folding technique. Based on the outcome, we believe that it would have been better to use a slightly more tilted incision line. The shape of the nostrils was well maintained for 1-year post-surgery, but a longer follow-up period is required to confirm the outcomes. If symptoms recur, it would be necessary to remove any source of inflammation, such as the implant.
In conclusion, we describe our successful use of scar folding to treat mucosal HTS and resultant left nostril stenosis after open rhinoplasty. In light of the outcomes at 1-year post-surgery, we emphasize the importance of controlling inflammation, as well as the possible use of a more tilted incision line, which might further improve the postoperative shape of the nostrils.
Notes
No potential conflict of interest relevant to this article was reported.
Ethical approval
The study was approved by the Institutional Review Board of Chungnam National University Sejong Hospital (IRB No. 2023-01-005).
Patient consent
The patient provided written informed consent for the publication and use of her images.