|
 |
- Search
| Arch Aesthetic Plast Surg > Volume 29(3); 2023 > Article |
|
Abstract
Advances in plastic surgery have included a shift toward less invasive procedures. To improve outcomes and avoid incisional surgery, numerous noninvasive face-lifting techniques have been studied. This includes thread-lifting, a technique that promises to correct facial aging with limited scarring, rapid recovery, and minimal complications. As the population ages, an increasing number of ordinary people in South Korea are undergoing thread lifting procedures for the purpose of rejuvenation. The procedure involves insertion of a thread under the skin into the subcutaneous tissue, using a long needle as a guide. Dents or barbs prevent the thread from slipping and provide uniform aggregation of soft tissue to create a new volume contour when the thread is lifted. This procedure has gained worldwide popularity and is frequently performed. However, some minor complications have been reported. In this paper, we report an unusual complication: an obstructive stone in the parotid (Stensen) duct after a thread-lifting procedure using nonabsorbable anchoring threads.
The thread-lifting procedure using Aptos thread was introduced by Dr. Sulamanidze in the late 1990s. Compared to general incisional surgery, thread lifting is a minimally invasive procedure for facial rejuvenation [1,2]. It became more popular after it was approved by the U.S. Food and Drug Administration in 2005 [3,4]. Since then, various techniques have been developed. Some authors have reported delayed complications, including foreign body granuloma and great auricular nerve neuropathy after thread-lifting procedures using nonabsorbable polypropylene thread. As a result, many doctors adopted the use of absorbable suture materials, assuming this would be a better option for improving skin texture and addressing safety concerns. In South Korea, however, even general practitioners who have not received plastic surgery education can perform this procedure for members of the public. Unfortunately, there have been several reports of acute and delayed complications. Complications can include mild facial asymmetry, erythema, hematoma, swelling, discomfort, eczema, thread exposure, and scarring. We present the case of a 70-year-old man who experienced an unusual complication after undergoing thread lifting with a nonabsorbable anchoring thread.
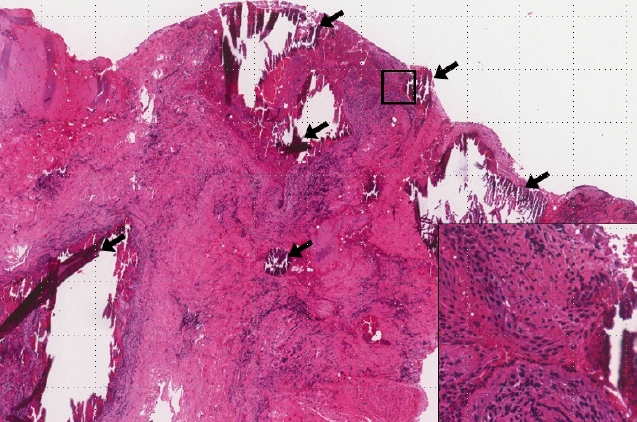
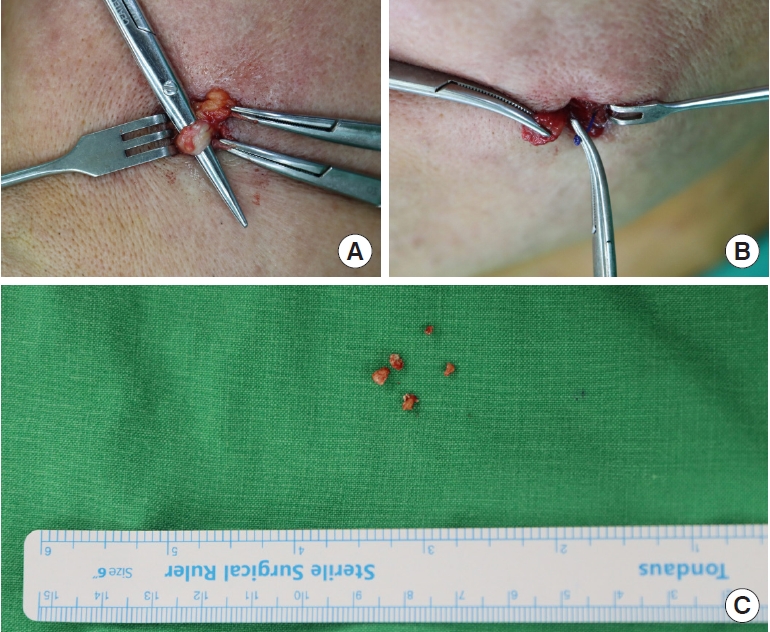
A 70-year-old male patient with an unremarkable medical history presented to our outpatient department with a palpable mass on his left cheek that had been present for 2 to 3 weeks. On physical examination, there was swelling, erythema, and warmth on the left cheek with a hard palpable mass (Fig. 1). The patient reported no history of trauma, surgery, or procedures in the affected area. A computed tomography scan revealed a benign-appearing calcification in the subcutaneous layer of the left cheek (Fig. 2). Accordingly, surgical removal and biopsy of the lesion were performed under local anesthesia. An incision was made in the affected area and, after careful dissection, it was confirmed that the parotid duct had been anchored with a suture and was dilated and obstructed by calcified stones (Fig. 3). Detailed examination of the patient in the operating room found that the patient had undergone thread lifting 2 years ago. Since the parotid duct remained obstructed after removal of the stones and anchoring suture, proximal ligation of the Parotid duct was performed. Postoperatively, the patient was advised to have further surgery to remove the remaining anchoring suture material under general anesthesia to reduce inflammation and prevent recurrence. However, the patient refused and requested conservative treatment. The biopsy results confirmed calcified keratin material (Fig. 4). Although general disinfection and antibiotic treatments were maintained, serous fluid leakage and slight erythema were noted at the surgical site. An amylase test and sialography were ordered since we were considering botulinum toxin treatment if salivary leakage was confirmed by the tests. However, the amylase test result was normal, and complete obstruction of the parotid duct was found by sialography (Fig. 5). As a result of conservative treatment (facial bandage with antibiotic and antiseptic treatments), the leakage volume gradually decreased, and the symptoms subsided. The patient fully recovered within 2 weeks, and no recurrence or delayed side effects were seen at a 3-month follow-up examination.
Since the late 1990s, when Dr. Sulamanidze developed the first thread-lifting technique using barbed sutures, the use of thread lifting has steadily increased. The use of threads for face lifting has the advantage of a short recovery time, minimal scarring, effective lifting, and patient satisfaction. However, there are also some complications related to thread lifting. One study reported adverse events in 20 of 29 patients who underwent face lifting with polypropylene threads. The most common side effect was intractable pain, followed by dimpling, palpable threads, thread extrusion, and paresthesia [5]. In a 2004 study by Wu [6], nine of 102 patients experienced palpable thread ends with pain, eight patients had thread migration, five patients developed an infection or granuloma, and five patients experienced skin dimpling or irregularities. According to a report by Kaminer et al. [7], 12 of 20 patients reported swelling, bruising, pinching, visibility of threads, and ear numbness. Fortunately, these complications were usually mild to moderate and could be corrected with relatively simple procedures without permanent sequelae.
In 2017, Yeo et al. [8] investigated early complications in thread-lifting procedures that used absorbable anchoring sutures. In that study, minor complications such as pain, numbness, discomfort, and mild bleeding were excluded. Of the 144 patients, three had dimples, five had thread exposure, three had alopecia, three had incomplete correction, one had asymmetry, and one had an injury that improved with conservative treatment (antibiotic and anti-inflammatory medication).
The procedure of thread lifting is performed as follows. Initially, the patient is positioned upright. The design is made about 2 to 3 cm away from the corner of the mouth. The threadsŌĆÖ exit point is located between two lines. One extends to the mandibular angle from the lateral canthus and the other is a vertical line from the lateral canthus. The spacing distance of each thread is 1 cm. An anchoring site is established 2 cm above the upper part of the ear, and a 3 ├Ś 2 cm area nearby is shaved. Threads are introduced with curved needles into the temporal anchoring site, and the threads are fixed to the deep temporal fascia. A long needle thread is inserted into the hole, passes under the subcutaneous layer, and penetrates the skin of the designed exit point. After repeating this step, extra thread is cut from the exit point and gently pulled out. Next, the thread is pushed slightly and buried under the skin. After this process, the dimple effect is removed by applying manual pressure. Since this procedure is repeated without direct visual guidance, it rarely results in parotid duct injection. This study presents a rare case, in which an obstructive stone in the parotid duct was found after a thread-lifting procedure using nonabsorbable anchoring threads (Fig. 6).
The most serious complications of thread lifting are parotid duct and parotid gland injuries. Therefore, the surgeon should be familiar with the anatomical structure of the parotid duct. The parotid duct (also referred to as the Stensen duct, after the Danish neuroanatomist Niels Stensen), is formed in the deep lobe of the parotid gland and emerges from the anterior border of the parotid after receiving ductules from both lobes. It travels anteriorly across the cheek surface to the masseter muscle, angles along the anterior border of the masseter muscle, penetrates the buccinator, and opens to the mucous membrane of the opposing cheek at the upper second molar tooth [9]. Facial lacerations can lead to duct amputation, and there is also a risk of iatrogenic injury during facial rejuvenation surgery and injections of botulinum toxin into the masseter muscle. The surface mark of the duct generally exists on the line between the tragus or intertragic notch of the auricle and the midpoint of the philtrum. Recent papers report that a better guide for location of the duct is within 1.5 cm of the midpoint of the line between the lower border of the tragus and the mouth angle [10]. Signs and symptoms of parotid duct injury include edema, swelling, or serous drainage from the incision or wound. Traumatic duct injuries present similar signs and symptoms (swelling or leakage of salivary fluid from the wound) and can often be more easily diagnosed because of the injury site or open wound. Patients may also experience swelling and changes in drainage in the presence of food. A sialocele is often misdiagnosed as a hematoma or a soft-tissue infection and may also accompany a soft-tissue infection.
As confirmed in previous studies, parotid duct injury caused by thread lifting is a rare complication. An obstructive stone in the parotid duct, as found in this case, is especially rare [11]. To prevent this complication, it is important for the surgeon to have an accurate understanding of the anatomy of the parotid duct and to mark it on the skin surface prior to surgery. If parotid duct damage is rapidly diagnosed, with or without the aid of sialography, primary repair is generally recommended unless a more urgent treatment priority exists. Although some authors advocated conservative treatment in the past, it is not currently recommended. If a parotid duct injury is missed, a sialocele, salivary fistula, or salivary duct cyst may occur and can be further complicated by infection. Under such circumstances, Parotid duct repair becomes impossible due to inflammation and scar tissue, so botulinum toxin injection may be considered. Proximal ligation of the duct, superficial parotidectomy, tympanic neurectomy, and radiotherapy can also be considered, but recent studies favor botulinum toxin injection [12,13].
Thread-lifting procedures are performed frequently in South Korea. Although the use of absorbable threads is increasing, permanent lifting threads are still on the market. As a result, we expect that problems like the one presented in this report will continue to appear, albeit infrequently. Early diagnosis and appropriate treatment are essential to properly manage this complication. Both nonsurgical and surgical treatments can be successful. Botulinum toxin injection may help avoid more invasive treatments by providing an additional treatment option in these cases [14]. In particular, practitioners must be trained to thoroughly understand the anatomical structure of the facial surface and to accurately evaluate and treat side effects when they occur. Consistent and long-term follow-up evaluation is also important to determine whether thread lifting provides long-lasting and satisfactory results.
Notes
Ethical approval
The study was approved for exemption by the Institutional Review Board of Jeonbuk National University Hospital (IRB exemption No. CUH 2022-12-035).
Patient consent
The patient provided written informed consent for the publication and use of his images.
Fig.┬Ā2.
A computed tomography scan revealed a benign-appearing calcification (arrow) in the subcutaneous layer of the left cheek.
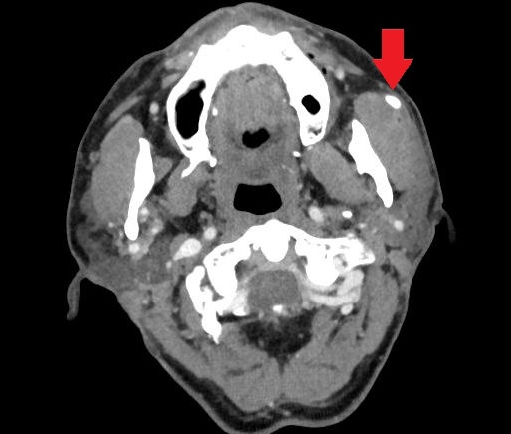
Fig.┬Ā3.
Intraoperative photographs. (A) The parotid duct was dilated and obstructed. (B) The parotid duct was anchored by thread lift sutures. (C) Calcified stones.
REFERENCES
1. Sulamanidze MA, Fournier PF, Paikidze TG, et al. Removal of facial soft tissue ptosis with special threads. Dermatol Surg 2002;28:367-71.


2. Sulamanidze MA, Paikidze TG, Sulamanidze GM, et al. Facial lifting with ŌĆ£APTOSŌĆØ threads: featherlift. Otolaryngol Clin North Am 2005;38:1109-17.


3. Horne DF, Kaminer MS. Reduction of face and neck laxity with anchored, barbed polypropylene sutures (Contour Threads). Skin Therapy Lett 2006;11:5-7.
4. Rashid RM, Sartori M, White LE, et al. Breaking strength of barbed polypropylene sutures: rater-blinded, controlled comparison with non-barbed sutures of various calibers. Arch Dermatol 2007;143:869-72.

5. Rachel JD, Lack EB, Larson B. Incidence of complications and early recurrence in 29 patients after facial rejuvenation with barbed suture lifting. Dermatol Surg 2010;36:348-54.


7. Kaminer MS, Bogart M, Choi C, et al. Long-term efficacy of anchored barbed sutures in the face and neck. Dermatol Surg 2008;34:1041-7.


8. Yeo SH, Lee YB, Han DG. Early complications from absorbable anchoring suture following thread-lift for facial rejuvenation. Arch Aesthetic Plast Surg 2017;23:11-6.


10. Stringer MD, Mirjalili SA, Meredith SJ, et al. Redefining the surface anatomy of the parotid duct: an in vivo ultrasound study. Plast Reconstr Surg 2012;130:1032-7.

11. Winkler E, Goldan O, Regev E, et al. Stensen duct rupture (sialocele) and other complications of the Aptos thread technique. Plast Reconstr Surg 2006;118:1468-71.