 |
 |
- Search
| Arch Aesthetic Plast Surg > Volume 29(4); 2023 > Article |
|
Abstract
The cheek, a highly visible and significant aspect of an individual’s appearance, is situated adjacent to several structures involved in facial expressions, including the eye, mouth, and surrounding facial muscles. Consequently, aesthetic reconstruction for large cutaneous defects of the cheek remains a challenge for plastic surgeons. We experienced a case of an 83-year-old woman with a large (7×10 cm) facial defect following the removal of squamous cell carcinoma. We elevated a cervicofacial skin flap containing the superficial layer of the superficial musculoaponeurotic system and a blood supply via the dermal plexus in a random pattern. Through this method, we achieved aesthetically favorable reconstruction of a large facial defect using a cervicofacial transposition skin flap. By avoiding extensive dissection, we achieved adequate coverage for even a quite sizable facial defect, with a short recovery time. This method prevented facial nerve injury and made it possible to simultaneously obtain an aesthetically favorable outcome.
The structure of facial skin varies due to factors such as creases, wrinkles, and skin thickness, making the preservation of facial harmony and functional reconstruction of large defects in the facial area a challenging task for surgeons [1]. Facial defects can be reconstructed using a variety of methods, including primary closure, local flaps, distant flaps, or free flaps, depending on factors such as the size and location of the defects and the condition of adjacent tissues. Skin grafts are one option for addressing large facial defects, but they have limitations, such as postoperative deformation, contractive scars, differences in skin height, and variations in color and texture [2]. Therefore, many surgeons opt for flap coverage when dealing with large facial defects.
One type of a local flap is a cheek flap, which can be an advancement or rotation-fashioned flap, this type of flap was first described by Beare in 1969 and later fine-tuned and popularized by Mustarde and Schrudde. The length of the flap should be about four times the width of the defect. The point of greatest wound tension is at the apex of the flap. Rotation of the flap causes a standing cutaneous deformity at the base of the flap, which can be corrected by additional excision of a Burrow’s triangle [3].
The use of a cervicofacial or cervicothoracic advancement flap in head and neck surgery was first described in 1918 by Esser [4]. The conventional cervicofacial flap is an advancement flap that involves a wide dissection range, which can be expanded to the thorax under the clavicle [4]. Since its initial description, numerous technical variations have been reported and extensively documented in the literature for the effective reconstruction of large skin defects. Bokhari and Wang [5] published a case where they designed a rotational cervicofacial flap, carried out dissection just under the superficial musculoaponeurotic system (SMAS), performed wide-undermining down to but not inferior to the clavicle and the platysma, and reconstructed the defect in a tension-free manner with the rotational form.
In this report, we present an aesthetically effective reconstruction of a very large facial defect following the removal of squamous cell carcinoma. We describe our experience utilizing a modified approach to the modified cervicofacial transposition skin flap for large cheek defects, which resulted in minimal tension during defect closure. We also avoided dissection below the peri-clavicle area, as is done with standard cervicothoracic and cervicofacial flaps. By avoiding extensive dissection, we achieved adequate coverage for even a quite sizable facial defect, preventing facial nerve injury and simultaneously obtaining an aesthetically favorable outcome.
An 83-year-old woman was admitted to our hospital due to a potentially cancerous mass on the left cheek region, which had exhibited rapid growth over the course of 1 year. She engaged in farm work in her youth and was exposed to intense sunlight. She was concerned that her face would lose its original symmetry and that she would be left with significant scarring and skin discoloration following surgery. Upon physical examination, the mass appeared to have micro-bleeding and was soft in consistency without any tenderness. It measured 5.5 × 6.5 × 4.0 cm (Fig. 1). Squamous cell carcinoma was diagnosed based on a punch biopsy. Additionally, a computed tomography image was obtained to assess the extent of tumor invasion (Fig. 2). Although we explained that an additional assessment of the likelihood of carcinoma could be conducted, due to her old age, she did not want an additional assessment. Therefore, we focused on removing the mass, which was her main request, and making her face aesthetically symmetrical.
With the patient under general anesthesia, tumor excision was performed with a 1-cm safety margin, following the principles of oncological safety, and a full-thickness specimen was obtained. The surgical defect measured 70 cm2 (7 × 10 cm) (Fig. 3). After the tumor was resected, the defect base was the SMAS layer. After the tumor was removed, it was observed that the bottom (base) of the defect did not invade the SMAS layer. After confirming that the entire margin, including the tumor base, was negative for tumor cells through a frozen-section biopsy, the transposition flap was designed to have a rotation angle of less than 90° for the defect (Fig. 4).
In addition, around McKinney’s point, special efforts were made to separate the dissection plane above the SMAS and platysma to prevent damage to the anterior and posterior branches of the greater auricular nerve. Additionally, to avoid damage to the lobular branch, which may travel to a more superficial layer, the flap was designed at a location approximately 2 to 3 cm away from the ear lobule [6,7].
We elevated an 8 × 12 cm skin flap with Metzenbaum scissors rather than an electrocautery device. We approached the superficial SMAS layer on the cheek site above the mandibular angle, performed dissection above the platysma muscle to prevent damaging the marginal mandibular nerve and the facial artery, and designed a random-pattern skin flap where the dermal plexus circulation was maintained. We continuously sprayed warm saline over the flap during flap elevation to maintain flap circulation (Fig. 5).
Defect reconstruction was performed through transposition and advancement, and the dermal vascular plexus was maintained. A 5-point quilting suture was performed between the flap subcutaneous tissue and defect base to prevent flap drooping or ectropion due to gravity and flap tension. Once the flap was positioned on the defect, meticulous hemostasis was performed via electrocautery to prevent hematoma formation. Additionally, Penrose drain tube was inserted along the flap’s lower surface, and a mild compression dressing with floppy wet gauze was applied.
The large cheek defect after tumor resection fully recovered without wound dehiscence, ectropion, or scar contraction that could affect facial symmetry. The patient recovered without complications, such as allodynia in the involved skin area, otalgia, or discomfort on cold exposure. The patient’s hospital stay was only 2 days. Eighteen months after the operation, she expressed satisfaction with the symmetric appearance and minimal scar formation, and no recurrence of the skin lesion was noted (Fig. 6).
The cheek is an especially prominent and significant aspect of an individual’s appearance [8]. Cook et al. [9] stressed the importance of considering skin color, texture, and the tissue’s pliability and flexibility when selecting a surgical technique for cheek reconstruction.
A skin graft can be an effective option for treating large facial defects; however, scarring may still occur due to variations in thickness or texture. While a free flap procedure offers greater flexibility in size selection and design, it may be less suitable for elderly patients or those in poor general health, as it necessitates a lengthy surgery and involves consideration of donor site morbidity.
The cheek and neck can be viewed as a single anatomical location due to their similar skin vascularity, texture, and thickness. As a result, the cervicofacial flap has been identified as the preferred treatment for cheek defects, given its excellent mobility and outstanding cosmetic outcomes.
The cervicofacial rotation-advancement flap is a variation of cervicofacial flaps that was first implemented by Mustarde [10]. Cervicofacial flaps are a frequently used method for reconstructing soft tissue defects on the cheek. These flaps can be divided into two categories: anterior-based flaps introduced by Juri and Juri [11], into which blood flows from the submental or facial arteries, and posterior-based flaps, into which blood flows from the preauricular or superficial temporal arteries.
In this study, our cervicofacial transposition flap surgery approach was based on a random-pattern skin flap, which offers a favorable rotation arc following the transposition design, rather than the conventional cervicofacial rotation and cheek advancement flap. This advantage allows for dissection of only the size of the defect. By utilizing the plane above the SMAS, the platysma muscle and marginal mandibular nerve can be preserved. In addition, if the surgeon closely keeps to the dissection plan, damage to the greater auricular nerve during surgery can be prevented. Consequently, the area of dissection is smaller than that of the cheek rotation or advancement flap. The cervicofacial transposition skin flap procedure is relatively simple, requiring less anesthesia and surgical time compared to other flaps, resulting in cost savings and making it more suitable for unfit patients. Additionally, it consistently provides an excellent color and texture match with the patient’s facial skin.
This flap, however, has some limitations. If the neck skin is nonredundant due to insufficient wrinkles on the neck, there can be limitations in the flap design. Therefore, additional studies should investigate the size of defects that can be reconstructed based on an increased number of cases. Moreover, since blood circulation is expected in the dermal plexus, there is an increased likelihood of marginal necrosis. Finally, this method is also unsuitable for the treatment of deep defects because it is a thin flap [12].
In conclusion, this modified cervicofacial transposition skin flap can be a reliable option for cheek reconstruction in cases of large defects. This method is expected to be used as a reconstruction technique for cheek defects of various causes, as well as post-tumor reconstruction. This case demonstrated that the modified cervicofacial transposition skin flap can adequately address both cosmetic and reconstructive aspects.
Notes
Ethical approval
The study was approved by the Human Ethics Committee of the Chosun University IRB (IRB No. CHOSUN 2022-11-019).
Patient consent
The patient provided written informed consent for the publication and the use of her images.
Fig. 2.
Computed tomography evaluation. A 5.5×6.5×4.0 cm tumor is identified in the (A) coronal view and (B) transverse view.
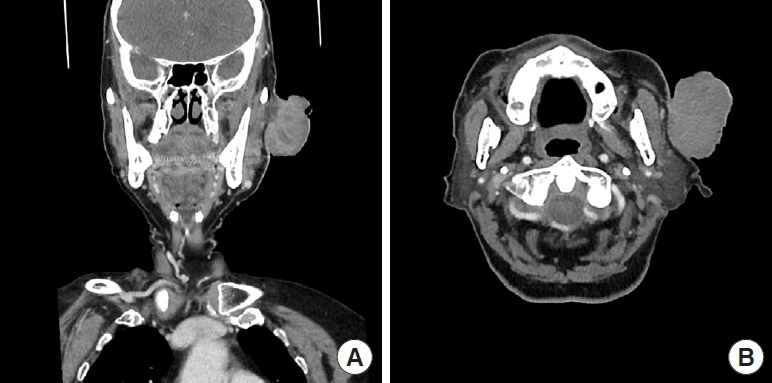
Fig. 3.
Intraoperative view. (A) The tumor was diagnosed as squamous cell carcinoma, (B) and during the operation, the size of the defect was measured to be 7×10 cm.

Fig. 4.
Design of the incision line for the cervicofacial transposition flap (point A, B, C). The gray area represents the defect following tumor resection (defect size: 7×10 cm). The transposition angle for the defect portion is less than 90° (indicated by the blue dotted line). Point P is the pivot point, point X is the quilting suture area; the quilting suture had five points, including the central part of the flap. Excessive dissection toward the ear lobe was avoided to prevent damage to the greater auricular nerve and a shape deformity after donor site closure.
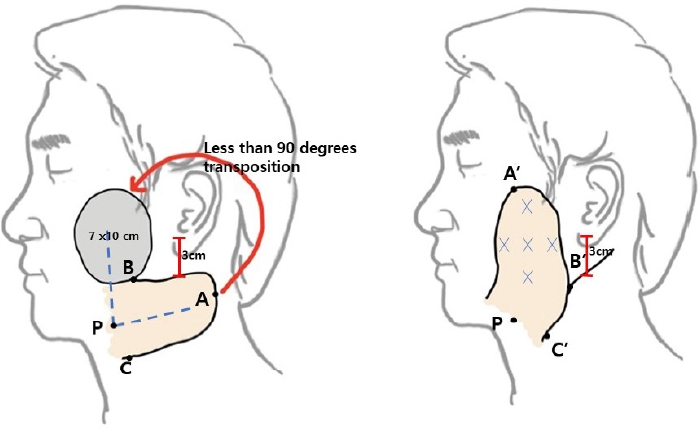
Fig. 5.
Layer of flap dissection in the cheek area and mandibular angle area (red box: dermis, subcutaneous tissue). Since the flap only contained skin and subcutaneous tissue above the superficial musculoaponeurotic system, it can preserve the nerve and main vessels. The donor site was undermined to a relatively minimal extent until primary closure was possible.

REFERENCES
1. Russo F, Linares M, Iglesias ME, et al. Reconstruction techniques of choice for the facial cosmetic units. Actas Dermosifiliogr 2017;108:729-37.


2. Rieck B, Giesler T. A medially based cervical transposition flap for soft tissue coverage of the cheek. Eur J Plast Surg 2004;27:20-3.


3. van Onna MA, Haj M, Smit JM, et al. Long-term outcome of the cheek advancement flap, a report of 41 cases. J Plast Surg Hand Surg 2016;50:354-8.



4. Esser JFS. Die Rotation der Wange: und Allgemeine Bemerkungen Bei Chirurgischer Gesichtsplastik. FVC Vogel Verlag;; 1918.
5. Bokhari WA, Wang SJ. Modified approach to the cervicofacial rotation flap in head and neck reconstruction. Open Otorhinolaryngol J 2011;5:18-24.

6. Sharma VS, Stephens RE, Wright BW, et al. What is the lobular branch of the great auricular nerve? Anatomical description and significance in rhytidectomy. Plast Reconstr Surg 2017;139:371e-8e.


7. Yang HM, Kim HJ, Hu KS. Anatomic and histological study of great auricular nerve and its clinical implication. J Plast Reconstr Aesthet Surg 2015;68:230-6.


9. Cook TA, Israel JM, Wang TD, et al. Cervical rotation flaps for midface resurfacing. Arch Otolaryngol Head Neck Surg 1991;117:77-82.











