Feasibility of ultrasonic surgical system in breast total capsulectomy
Article information
Abstract
Background
Capsulectomy is a crucial procedure in cosmetic breast surgery, and there is demand for an efficient and convenient tool to perform it. This study analyzed the postoperative outcomes of total capsulectomy by comparing an ultrasonic system to conventional electrosurgery.
Methods
This retrospective cohort study included patients who underwent total capsulectomy and implant removal from 2012 to 2020. The ultrasonic surgery group underwent this procedure using the Harmonic scalpel, while the electrosurgery group underwent the same surgery using conventional electrocautery. A statistical analysis of the two groups was performed using multivariate linear regression analysis to determine the unbiased effect of ultrasonic surgery on operative efficiency and outcomes.
Results
A total of 89 patients were included in the study. The operative time was significantly shorter in the ultrasonic surgery group (60 minutes vs. 70 minutes, P=0.002). After adjusting for other independent variables that might also be related to the outcomes, shorter operative time (P=0.014) and faster drain removal (P=0.003) were associated with the use of ultrasonic surgery.
Conclusions
The use of an ultrasonic system (Harmonic scalpel) for total capsulectomy and explantation in cosmetic breast revision surgery was associated with shorter operative times and faster drain removal than conventional electrosurgery.
INTRODUCTION
Increased operative efficiency and reduced postoperative discomfort in cosmetic breast revision surgery are important factors in patient satisfaction and anesthetic cost. Complete capsulectomy is a time-consuming and tedious procedure due to the narrow surgical field and awkward positioning for the surgeon. Therefore, it is worthwhile to search for a more convenient and efficient means of performing capsulectomy.
Capsulectomy is a core procedure in cosmetic breast surgery. In revisional breast surgery involving an implant, manipulation of the capsule is always needed to some extent. The number of cases requiring capsule manipulation and implant removal or exchange continues to rise. Thus, there is a need for an efficient and convenient tool to perform capsulectomy successfully [1]. Currently, most surgeons use the classic scalpel or electrocautery for breast capsulectomy. Monopolar cautery uses a high-frequency electrical current from a single electrode [2]. Although most surgeons are familiar with using this older system, it has a high collateral heat dispersion and produces unwanted tissue damage [3]. Consequently, drainage volume and the risk of seroma formation may increase due to the inefficient sealing of lymphatic vessels [3-5].
There has been significant progress in other fields of surgery to develop better tools that facilitate surgical practice [3,6]. Specifically, energy-based devices have been developed to aid in dissection and hemostasis that enable cleaner, safer, and faster surgery [7]. One well-known ultrasonic surgical system is the Harmonic scalpel (Ethicon). This device uses a high-power, high-frequency (55.5 kHz) ultrasonic system for dissecting tissue and sealing blood vessels [8]. It is a multifunctional instrument, combining vascular sealing and tissue dissection to facilitate surgical procedures. An important advantage of this device is that it produces less thermal injury than electrocautery. Various studies have shown a notably reduced rate of postoperative complications with this system [9,10].
However, no study has investigated the benefits of using the ultrasonic system for cosmetic breast revision procedures. Therefore, we compared the postoperative outcomes of total capsulectomy and explantation using the ultrasonic system to the outcomes obtained using only the conventional electrosurgery system. We also share our detailed surgical procedure for total capsulectomy using the ultrasonic system.
METHODS
Ethics statement and patient selection
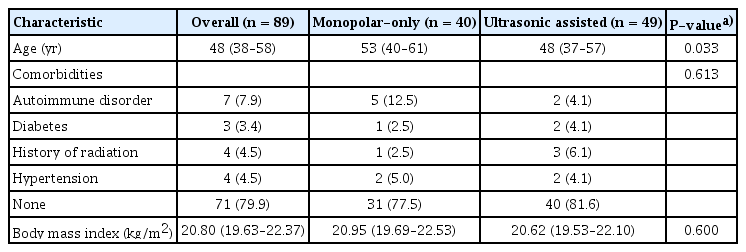
The study design was approved by the institutional review board of our medical institution (IRB No. KC20RASI0354). The requirement for informed consent was waived due to the retrospective nature of the study. The study was conducted in compliance with the Declaration of Helsinki. This was a retrospective cohort study including patients who underwent total capsulectomy and implant removal for various reasons from 2012 to 2020. Through retrospective chart review, we collected data on patients who had undergone complete capsulectomy and implant removal, using either conventional electrosurgery or ultrasonic surgery. The patient demographics are summarized in Table 1.
Study design
A retrospective chart review was performed to analyze demographics, implant-related parameters, and operative outcomes. The ultrasonic surgery group included patients who had undergone total capsulectomy and implant removal with the Harmonic scalpel. The electrosurgery group included patients who had undergone surgery with the conventional electrocautery system. The implant-related parameters included implant type, Baker grade, implant volume, laterality, number of previous revisions, reason for explantation, and time to explantation. Operative outcomes included operative time, total drainage volume, interval until drain removal, any complications, any reoperation, and implant condition at explantation. All operations were performed by the same team (DYO).
Statistical analysis
Data analyses were performed using R statistical software [11]. Continuous variables were analyzed using the Mann-Whitney U test. Discrete variables were analyzed using the chi-square test or Fisher exact test to determine the significance of differences between the two groups. Multiple linear regression analysis and tabular production were performed using the gtsummary package in R [12].
Surgical technique and perioperative management
A detailed explanation of the procedure can be found in the Supplementary Video 1. Incision and exposure of the capsule were done uniformly with scalpel and electrocautery. In the ultrasonic surgery group, an ultrasonic scalpel device measuring 20 cm in length was used (HD 1000i Shears handpiece, curved tip, and GEN11 generator; Ethicon) (Fig. 1A). In the electrosurgery group, the Valleylab FT10, a conventional pencil-type electrocautery system, was used (Medtronic). The power of the ultrasonic system was set to level 5 (comparable to 25 W in the electrocautery system), and the electrocautery system was set to 30 W. Regardless of the surgical device used, total capsulectomy with implant removal was performed in a uniform manner. The previously placed inframammary fold incision was selected for the surgical approach (Fig. 1B). After the skin incision, dissection was completed down to the subcutaneous plane until the capsule was exposed, and the capsulectomy was initiated. First, dissection along the pre-capsular plane in a caudal to cranial direction was performed (Fig. 1C). The right amount of exposure with long-lighted retractors was crucial for adequate dissection. After reaching the uppermost cranial portion of the implant capsule, the resultant dissection pocket was gradually widened in the medial and lateral directions. This completely released the capsule and implant from the overlying muscle and the subcutaneous tissues. Subsequently, the basal portion of the capsule was approached. The capsule-implant complex was lifted from the chest wall, and the dissection was performed in the post-capsular plane. This was also done in a caudal-to-cranial and medial-to-lateral progression. This systematic sequence entirely separated the capsule and implant from the surrounding native tissue (Fig. 1D). After dissection, curettage was judiciously performed for the small amount of remnant capsule that densely adhered over the rib perichondrium. After manually removing the capsule-implant construct through the incision, routine bleeding control, irrigation, drain insertion, and closure were performed.

Overall surgical sequence and resultant capsulectomy specimen. (A) Ultrasonic surgical device used in this study; a 20-cm-long shaft aids in the efficient manipulation of tissue in the cranial portion of the breast pocket. (B) Preoperative design utilizing the previous incision line. (C) Intraoperative photo during capsulectomy with an ultrasonic device. The plane of dissection (white line) between the capsule (asterisk) and the muscle is denoted. (D) The removed capsule and implant with complete continuity.
The patients were discharged the day after surgery. During outpatient follow-up, the negative suction drains were removed when the drainage volume was <30 mL per 24 hours.
RESULTS
Demographics
In total, 89 patients were included in the study. Forty patients received total capsulectomy using electrosurgery. Forty nine patients received total capsulectomy with the ultrasonic device. There was no statistical difference in comorbidities (autoimmune disorder, diabetes, radiation history, and hypertension) or body mass index (BMI) between the two groups. The mean age of the ultrasonic surgery group was younger than the electrosurgery group (48 years vs. 53 years, P=0.033) (Table 1).
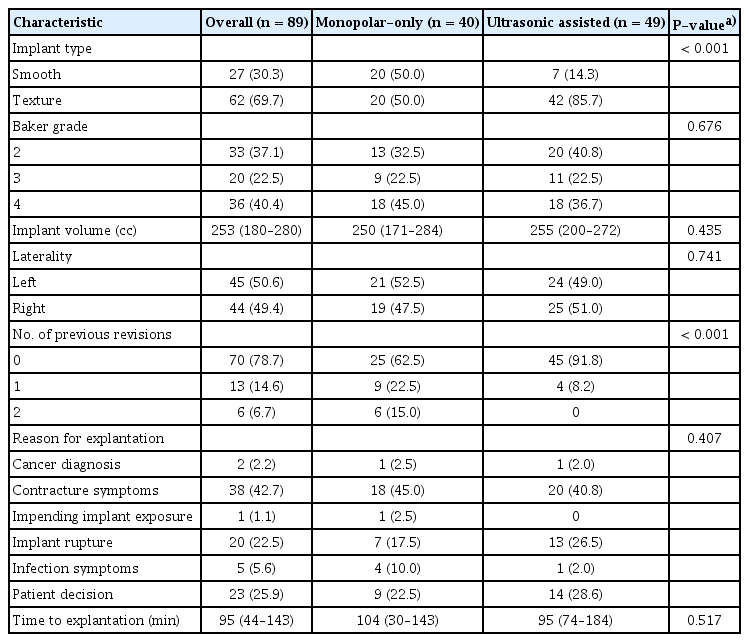
Implant-related parameters
Most of the cohort had textured implants (70%). The Baker grades did not differ between the two groups (P=0.676). The mean implant volumes were 250 cc and 255 cc in the electrosurgery group and ultrasonic surgery group, respectively, reflecting a statistically nonsignificant difference (P=0.435). In addition, laterality did not show significance (P=0.741). Regarding the number of previous revisions for each group, 15% of the electrosurgery cohort had tertiary revisions (P=0.001; statistically significant). Contracture symptoms were the primary reason for explantation (45% in the electrosurgery group and 41% in the ultrasonic surgery group), and the distribution of reasons for explantation was broadly similar between the two groups (Table 2).
Operative outcomes
The operative time was 15% shorter in the ultrasonic surgery group (60 minutes vs. 70 minutes, P=0.002). The mean total drainage volume was 97 cc and 72 cc in the electrosurgery and ultrasonic surgery groups, respectively (P=0.364). The interval until drain removal was slightly longer in the electrosurgery group, but without statistical significance (5.5 days vs. 5.0 days, P=0.100). Although three patients developed postoperative seromas in the electrosurgery group, this was not statistically significant (P=0.087). No return to the operating room was necessary in either group. The proportion of grossly damaged implants, whether infected or ruptured, did not differ between the two groups (P=0.481) (Table 3).
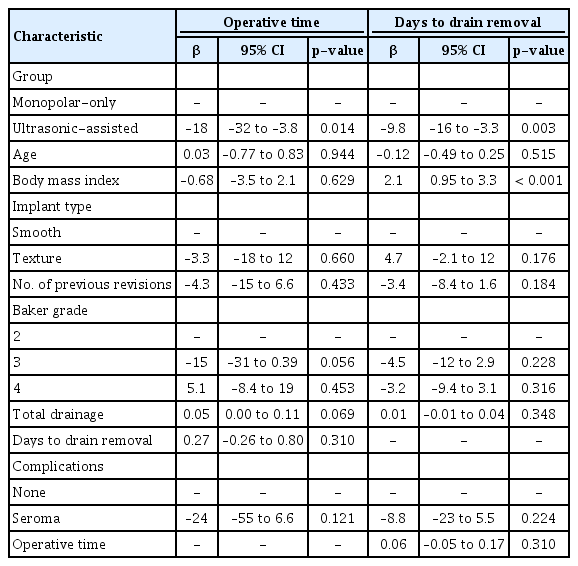
Multivariate regression analysis
By directly comparing the demographic, implant-related, and perioperative outcomes of the two groups, we explored whether use of the Harmonic scalpel was independently associated with improved operative outcomes (shorter operative time and interval until drain removal). Thus, we performed multivariate linear regression analysis, using the factors that showed statistically significant differences to confirm that ultrasonic surgery reduced operative time and time to drain removal. After adjusting for other independent variables that might also be related to the outcome, shorter operative time (P=0.014) and faster drain removal (P=0.003) were again associated with the use of ultrasonic surgery (Table 4).
DISCUSSION
Numerous studies have reported that ultrasonic surgery is a useful tool for optimizing patient outcomes and reducing operative time, and its use has also been advocated for reconstructive breast surgery [13,14]. Despite the well-known efficiency of using an ultrasonic device in various surgical procedures, it remains outside the armamentarium of plastic surgeons in the field of cosmetic breast surgery. Therefore, we sought to objectively compare the operative times and duration of drain placement between patients who underwent surgery using an ultrasonic device and those who underwent surgery using a conventional electrocautery device. Multiple regression analysis showed that, after adjusting for other confounding variables, use of the ultrasonic device and lower BMI were the only factors correlated with a shorter operative time and quicker drain removal. This is in accordance with multiple previous studies suggesting the benefits of an ultrasonic system in other fields of breast surgery [3,5,7,8,14,15].
Exploratory analysis of the demographic and implant-related features of the two groups showed two significant differences. First, more patients had textured implants than smooth implants. This may seem counterintuitive because it has been shown that patients with smooth-surface implants are more likely to experience capsular contracture [16]. We think that the abrupt rise in concerns about breast implant-associated anaplastic large cell lymphoma (ALCL) in recent years has encouraged patients with textured implants to seek medical examinations, leading to mechanical failures of their prosthesis to be identified earlier. Moreover, due to concerns about ALCL, they may have chosen explantation and complete capsulectomy rather than partial capsulectomy and implant exchange, despite an unbiased consultation. Another difference between the two cohorts was their mean age, which may have been affected by the reluctance of the older age group to agree to the additional cost of the newer device. However, regression analysis showed that neither surface texture nor age were factors significantly associated with a shorter operative time or drain duration.
The primary hypothesis of our study is that the operative time would be shorter in the ultrasonic group. Upon analysis, the use of the ultrasonic device was correlated with a 15% shorter operative time (Table 3), and regression analysis showed that this was statistically significant after adjusting for confounders (Table 4).
In the ultrasonic surgery group, the mean total drainage volume was reduced 22% (97 cc vs. 72 cc), but this difference did not show statistical significance in a direct comparison with the electrocautery surgery group (P=0.364). The interval until drain removal was also slightly shorter (5.5 days vs. 5.0 days), but this difference was also not significant. However, after adjusting for confounders, drain duration was significantly shorter in the ultrasonic surgery group (P=0.003). The finding of no reoperations in either group may be explained by the expedient soft tissue healing and effective lymphatic closure with the ultrasonic system. We recommend additional studies to further investigate the temporal trend in drain volume.
Complete capsulectomy is not always needed in routine implant exchange or removal [9,17]. However, it is our practice to attempt as complete a capsulectomy as possible in all cases. Total capsulectomy is always performed when explantation without reinsertion of a new implant is performed. This is done to proactively eliminate the long-term fibrotic burden and reduce confusion in future cancer screenings. Total capsulectomy is related to increased blood loss and higher postoperative drain volumes. This drawback can be actively managed by using the ultrasonic system, which closes off the lymphatic and blood vessels by effectively forming a protein coagulum, thus creating a tight seal. It has also been suggested that decreasing the drain volume and duration decreases the risk of surgical site infection [10].
A technical advantage of the ultrasonic device is the availability of a gun-type handpiece with a 20-cm shaft, which provides much more freedom and ease of use when manipulating the capsule through a small and remote incision in the upper pole. Although incisions at the inframammary fold are preferred to visualize the whole breast pocket, the cranial regions are the farthest and the most difficult regions to dissect. A device with sufficient length and jaw-type curved tips provides easier and bloodless pericapsular tissue manipulation.
Two drawbacks to using ultrasonic surgery must be noted. First, collateral heat arising from the shaft of the device must be actively cooled using a wet pad or frequent saline irrigation. If the shaft portion meets the skin, thermal injury may occur. Care must be taken to avoid contact with the inframammary incision area, which has the highest risk of contact. Second, the high cost of this device is a hurdle. Because insurance usually does not cover revision surgery for the breast, the addition of an ultrasonic device for surgery can be a significant burden to the patient.
Some limitations of this study must be acknowledged. First, the small cohort and retrospective design of the study may yielded a biased analysis. In particular, the higher rate of previous revisions in the monopolar cautery group may have acted as a confounder in the operative time. Second, subjective patient satisfaction was not measured because of the retrospective nature of the study design. Future studies are also needed to compare histologic specimens of the capsules from each group to further investigate the benefits of using the ultrasonic system.
In conclusion, the ultrasonic surgery system may be a useful adjunct in cosmetic breast surgery especially in total capsulectomy. Compared to the conventional electrosurgery system, the Harmonic system showed shorter operative times and smaller drain volumes. Statistical analysis showed that use of the Harmonic system was the main contributing factor to the shorter operating time and lower drain volume after adjusting for confounders. However, overcoming the cost barrier and preventing iatrogenic thermal damage from the device shaft are drawbacks that must be addressed.
Notes
No potential conflict of interest relevant to this article was reported.
Ethical approval
The study was approved by the Institutional Review Board of Seoul St. Mary’s Hospital (IRB No. KC20RASI0354) and performed in accordance with the principles of the Declaration of Helsinki.
Patient consent
The patient provided written informed consent for the publication and use of her images.
Supplemental material
Supplementary materials can be found via https://doi.org/10.14730/aaps.2023.00969.
Intraoperative video of total capsulectomy using the ultrasonic scalpel.