INTRODUCTION
In severe blepharoptosis, surgical options can usually be divided depending upon the severity and extent of levator muscle function. In cases of poor levator muscle function, surgery with contraction of the frontalis is needed directly via the muscle itself or indirectly via an artificial material between the frontalis muscle and the tarsal plate. The frontalis sling technique has been considered the main procedure to treat patients with severe eyelid ptosis for decades [
1-
6]. Blepharoptosis correction under local anesthesia via frontalis transfer (local FT) can be an effective, but aggressive treatment [
7]. However, if the patient is young or afraid of undergoing surgery, then surgery can be performed under general anesthesia (general FT). Silicone rod suspension surgery, a less invasive but effective treatment option, could be also performed under either general (general SS) or local anesthesia (local SS) [
8,
9].
The intraoperative eyelid level was adjusted until the eyelid margin covered 1.5 mm below the superior limbus of the cornea. Because the same surgeon performed all the procedures examined in this study, the effectiveness in correcting severe blepharoptosis was examined to assess whether the two operative options could be substituted for each other. In addition, the authors compare the effectiveness of the surgical options under both local and general anesthesia.
METHODS
We retrospectively compared the effectiveness of these surgical options in a non-randomized study. In the present study, we reviewed the medical records and photographs of 76 patients who had visited our clinic between 2006 and 2013 because of severe blepharoptosis and in whom a single senior doctor had performed the surgeries. Marginal reflex distance 1 (MRD
1) was measured as the vertical distance from the corneal light reflex during primary gaze to the upper eyelid margin. The levator function is the difference in height of the upper lid margin between the highest and lowest points of vision after the surgeon presses the patients’ eyebrow to block frontalis muscle function [
10]. A postoperative result was considered sufficiently symmetrical if the calculated difference between the postoperative MRD
1 (PostMRD
1) values of both eyes was 1 mm or less [
11].
Surgical procedure
Silicone rod frontalis suspension surgeries were performed under general (general SS) or local (local SS) anesthesia with minimal sedation using the pentagon modified technique [
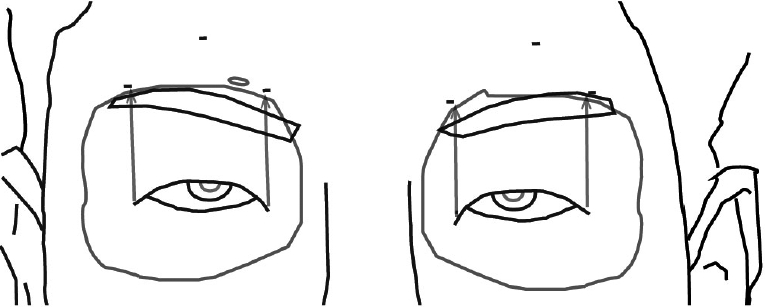
12]. One BD Visitec™ 20-gauge, 2-1/2 inch stainless steel, double straight needle (0.8 mm×40 cm solid silicone rod; Becton Dickinson and Company, Franklin Lakes, NJ, USA) was used. The eyelid skin was marked on the medial and lateral parts, and two stab incisions were made on the upper eyelid. Temporal and nasal horizontal incisions were made on the fold line of the upper eyelid, extending within 3 mm of the lateral and medial corneal limbus. In addition, the lateral, medial, and forehead incisions were made above the eyebrow. Lateral and medial eyebrow incisions were made approximately 3 mm above the orbital rim vertical to the lateral and medial canthal lines toward the temporal and nasal regions, respectively (
Fig. 1). In addition, a 5-mm forehead skin incision was made 7 mm above the central eyebrow around the orbital rim centrally. A lid guard was inserted for ocular protection. At first, 1:100,000 epinephrine mixed with 1% lidocaine was administered. After the incision and dissection of the five incision windows, one end of the straight needle was passed from the lateral eyelid incision window to the medial brow incision between the eyelid skin and orbicularis oculi muscle. Moreover, both a silicone rod and the superior margin of the tarsal plate were tied and fixed together with 7-0 nylon at two points through the eyelid windows, just after withdrawing the silicone rod back along the needle track. That end of the needle was passed through the medial eyelid incision window to the medial brow incision, and the other end of the needle was directed through the lateral eyelid window to the lateral brow window. The eyelid level was adjusted until the eyelid margin was elevated to cover 1.5 mm below the superior limbus of the cornea. Finally, both ends of the needles were passed through the central forehead incision window. Both parts of the extracted silicone rods were passed through the additional silicone tube and secured with 6-0 nylon to prevent loosening of the knots, and located under the frontalis muscle of the forehead. The skin brow incisions were closed with 5-0 vicryl and 6-0 nylon, and the eyelid incisions were sutured using 7-0 nylon.
FTs were also performed under general (general FT) or local (local FT) anesthesia. Two incision lines were designed just below the ipsilateral eyebrow and eyelid fold line, and 1:100,000 epinephrine mixed with 1% lidocaine was then administered. After the brow incision was made using a beveling approach to avoid the hair follicle, the L-shaped frontalis muscle flap was elevated to avoid injury to the facial nerve. Then, via the eyelid incision, the tarsal plate was exposed, and a tunnel from the tarsal plate to the brow window between the skin and orbicularis oculi muscle was created. The harvested muscle flap was transposed and attached to the anterior border of the tarsal plate via a temporary PDS suture. The eyelid level was also adjusted until the eyelid margin was elevated to cover 1.5 mm below the superior limbus of the cornea. After the corrected target level was checked, two PDS sutures were used to maintain the frontalis muscle and tarsal plate. The brow and eyelid skin sutures were secured using 7-0 nylon after the insertion of silastic drainage [
7].
Statistical analysis
Data analysis for MRD1 was performed using SPSS statistical software (version 16; SPSS Inc., Chicago, IL, USA). Data are expressed as the mean±standard deviation (SD). An independent sample t-test was used to compare preoperative MRD1 (PreMRD1), PostMRD1, and differences between PostMRD1 and PreMRD1 (DiffMRD1). PostMRD1 in the study groups was compared using the independent sample t-test after assuming equal variances or the Mann-Whitney test without assuming equal variances. The correlations in several variables such as age, surgical options, type of anesthesia, PreMRD1, PostMRD1, and DiffMRD1 were analyzed. In addition, improvements in the degree of ptosis were defined as the difference between PostMRD1 and PreMRD1. A two-sided P-value less than 0.05 was considered statistically significant.
DISCUSSION
In cases of poor levator function, the frontalis sling technique has been considered the main procedure for treating patients with severe blepharoptosis [
13]. The typical method is to sling the upper eyelid tarsus with the frontalis muscle itself; there are many different alternative methods such as levator resection, Müller-aponeurosis composite flap advancement, and the frontalis suspension procedure. The latter is commonly performed using bridge materials such as preserved fascia lata (PFL) or synthetic materials like polyester, polytetrafluoroethylene, nylon, polypropylene, and silicone rods, although there is no general agreement on which material is superior when compared to the others [
14,
15]. In the case of autologous materials, there have been concerns about donor site scarring. In the PFL group, later recurrence is known to be related to absorption of the fascia [
8,
16]. Fascia lata is not always a feasible option for all patients, as the patient needs to be at least 3 years old in order to have sufficient length to provide suitable fascia lata [
17]. Some studies have recommended using silicone rods [
18,
19]. Therefore, we focused on increases in the MRD
1 using these techniques in a retrospective, non-randomized study that compared FT and silicone rod frontalis suspension surgery under general or local anesthesia in our institution, including at least 6 months of follow up. If the patient had an early complication, details of the first postoperative MRD
1 was used instead of the postoperative MRD
1 of the repeat surgery after 6 months.
A lower PreMRD1 value indicates a greater severity of ptosis. In this study, the mean PreMRD1 of all 104 eyelids was -0.34±1.371 mm; the PreMRD1 values in the local FT group (0.01±1.391 mm), the general FT group (-0.39±1.195 mm), the local SS group (-0.91 ±1.623 mm) and general SS group (-0.41±1.281 mm) were not significantly different from one another. Based on this finding, we compared PostMRD1 and MRD1 differences between the two procedures under general or local anesthesia.
To assess symmetry and determine whether the eyelid level was adjusted to a good position, intraoperative direct decisions can be more simply and reliably made under local anesthesia. Therefore, such direct prediction is believed to be more suitable to correct ptosis and determine the degree of correction under local anesthesia. However, hematoma can be caused by muscle contraction and pain under local anesthesia (
Table 4). Nevertheless, because some patients had extreme anxiety about the surgery or were too young to be cooperative, they were given general anesthesia.
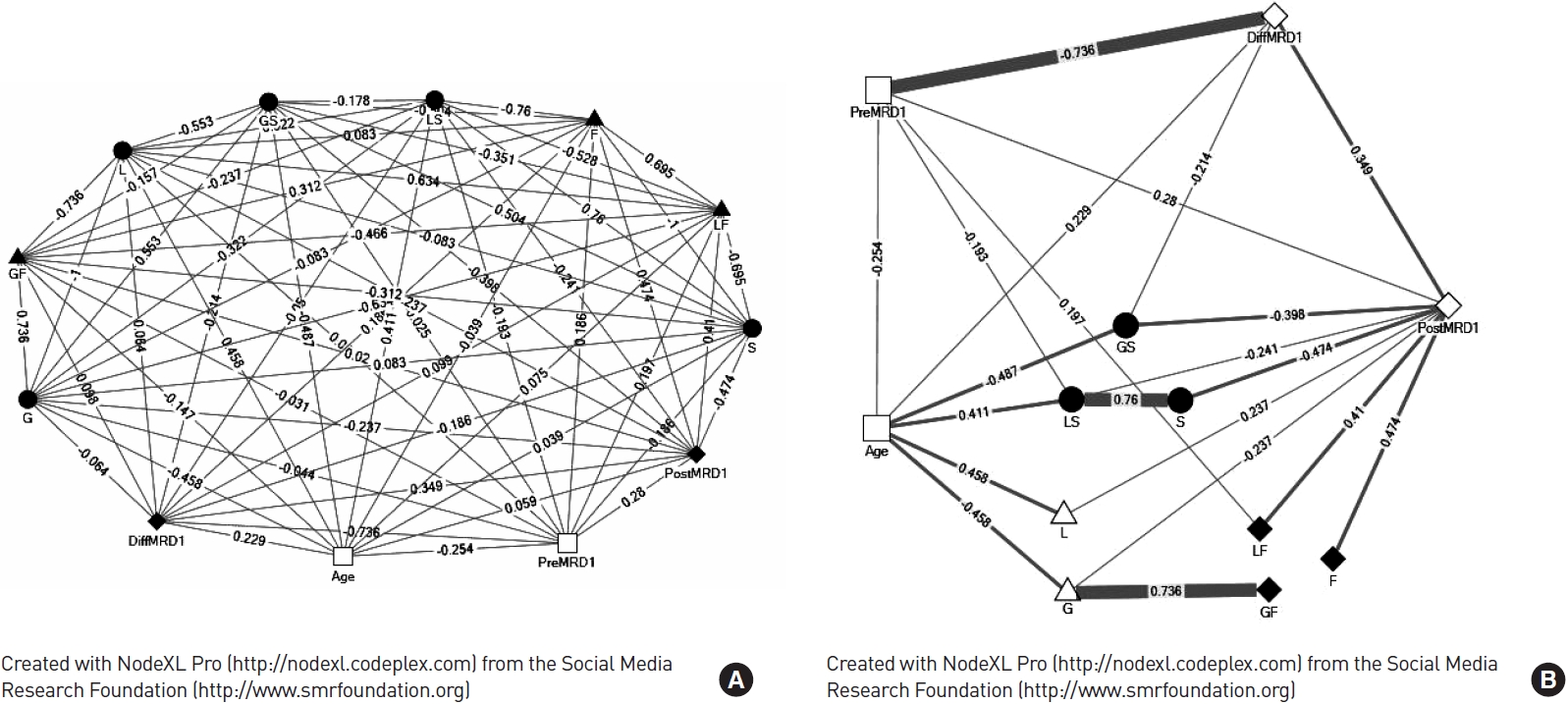
In a previous study, postoperative ptosis showed no relationship to preoperative ptosis severity, similar to the results of our data in most groups in this study [
13]. However, FT performed under local anesthesia was positively correlated with PostMRD
1, and weakly positive correlated with DiffMRD
1 and PreMRD
1 (
Fig. 2). A coefficient of 21.3% was found in the statistical causal relationship between PreMRD
1 and PostMRD
1 as observed from the following: PostMRD
1=2.041+0.235 ×(PreMRD
1) in the local FT group as determined by linear regression analysis (P=0.000 in one-way ANOVA), unlike other groups of our institute.
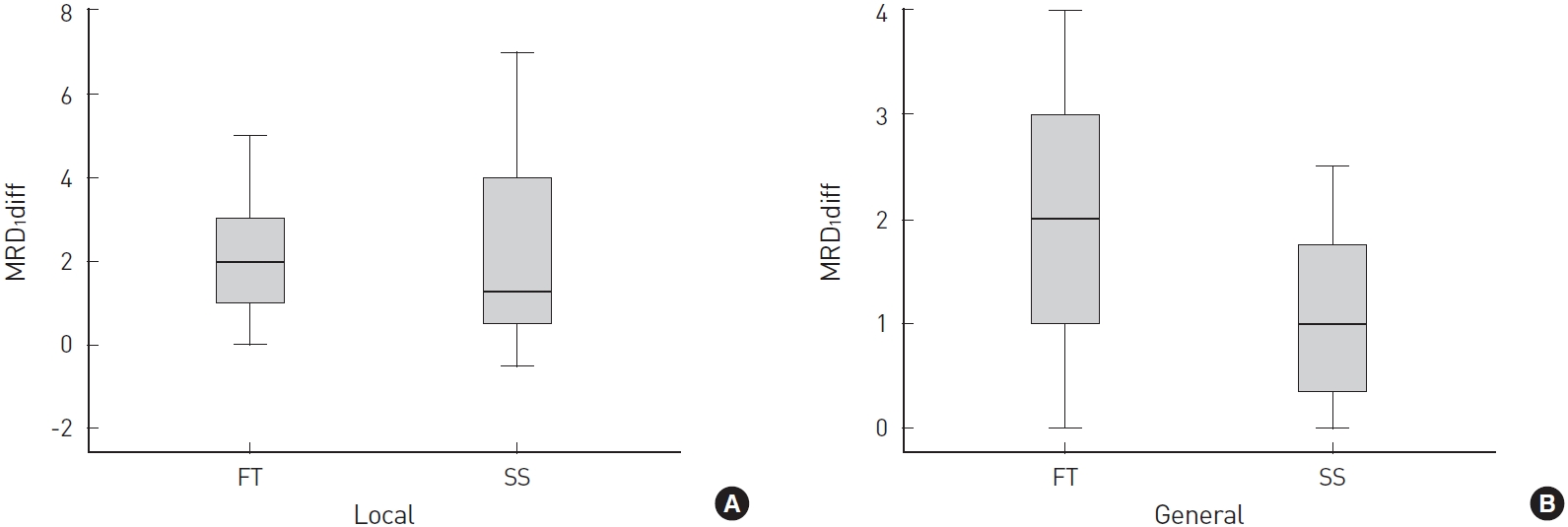
Few studies have mentioned the results of blepharoptosis after surgery under different anesthetic conditions, and the present study showed that both the general FT and local FT groups showed an average 2-mm MRD
1 increase, and the general SS group showed an average 1-mm MRD
1 increase. The mean MRD
1 differences in the local FT and general SS groups were 2.04±1.224 mm and 1.11 ±0.848 mm, respectively, and the MRD
1 difference in the general FT (2.17 ±1.339 mm) and general SS (1.11 ±0.848 mm) groups were statistically significant (
Table 3). The mean MRD
1 difference in the local SS group was not significant from those in the other three groups, and the PreMRD
1 and PostMRD
1 values in the local SS group were significantly different from those in the local FT group. Therefore, the calculated MRD
1 difference (2.01 ±1.921 mm) in the local SS group was expected to be similar to the MRD
1 difference in the local FT and general FT groups. In other words, the general FT, local FT, and local SS groups had an average of 2 mm or greater MRD
1 increase. Specifically, the local FT group had a definite positive correlation with PostMRD
1 unlike other variables. The group under local anesthesia had a weak correlation with PostMRD
1, and the group under general anesthesia had no correlation with PostMRD
1.
From the intergroup analysis (P=0.032 by ANOVA) of the eight age groups with regard to MRD
1 differences, the difference was higher for the age group of 61 to 70 years, followed by 41 to 50, 11 to 20, and 0 to 10 years. Further, in this study, most of the patients in the general SS groups were 10 years or younger, and these differences were thought to result from children’s inadequate frontalis muscle contraction [
20]. From this study, we believe a higher target tension level of the SS should be employed during surgery under general anesthesia compared to local anesthesia. Under general anesthesia, FT results in few complications and revision surgeries. Silicone rods are readily available and the tension can be adjusted in a relatively easier manner even under postoperative conditions. Further, even if the MRD
1 increase after general SS is relatively small, the frontalis suspension sling surgery using silicon rods seems to be a better option under local anesthesia; however, this procedure may be associated with recurrence (
Table 4). In the future, a prospective study is needed to determine the optimal increase in target tension level needed for improved effectiveness of the procedure under general anesthesia, because an increase in silicone tension could cause a longer period with incomplete eyelid closure during sleep and lagophthalmos in the downward gaze [
13].