Correction of the Sunken Upper Eyelid Depending on the Dermatochalasis or Blepharoptosis Using the Autologous Fat Grafting
Article information
Abstract
Background
To date, many methods have been proposed to resolve the sunken eyelid. We treated our clinical cases of sunken upper eyelid based on whether there is a concurrent presence of the dermatochalasis or blepharoptosis and then performed the autologous fat grafting using either closed or open technique.
Methods
According to the classification of the patients, we used the following injection techniques: First, we solely performed the autologous fat grafting using the closed technique in the sunken upper eyelid only group, for which we did the injection using a micro-injector cannula on the suborbicularis plane. Second, we performed such procedures as skin excision, orbicularis oculi muscle strip excision and levator aponeurosis advancement to manage each symptom in the sunken upper eyelid with dermatochalasis or blepharoptosis group. Simultaneously, we also made a small window in the lateral portion of the orbital septum using the open technique with metzenbaum scissors. Thus, we performed the intraseptal injection of the autologous fat.
Results
During a period ranging from January of 2012 to April of 2014, we treated a total of 53 patients. The patients were followed up during a mean period of four months. Thus, we obtained satisfactory treatment outcomes without notable complications.
Conclusions
In conclusion, our results indicate not only that surgeons should consider the fat grafting as one of eyelid-surgery procedures but also that they should perform it concurrently with blepharoplasty or blepharoptosis correction for the purposes of obtaining good treatment outcomes.
INTRODUCTION
The youthful brow-upper eyelid complex is characterized by soft tissue fullness; which extends from the orbital sulcus to the hairbearing portion of the brow [1]. This is accompanied by the presence of a sharp, pretarsal show in the youthful upper eyelidcrease. There is a minimal amount of exposed skin on the visible upper lid with the eyes opended. The lateral upper lid and brow have a very full, round shape. Moreover, the smooth transition occurs without the skeletalization of the orbital rim into the adjacent temple esthetic unit [2].
Aging of the brow-upper eyelid complex is the multi-factorial process that includes the results of gravity, fat atrophy, solar damage and selective bone resorption [3]. In particular, the sunken eyelid is aggravated by uneven and site-specific resorption of the orbital rim as well as the fat atrophy of the upper eyelid. This makes individuals look older and more tired, eventually producing high or multiple folds. Moreover, the sunken eyelid may also occur due to congenital causes such as a strong bony orbital framework associated with delicate eyelids and soft tissue disproportion [4]. Therefore, young individuals may also develop the sunken eyelid with no respect to the aging process.
In a clinical setting, surgeons may often encounter patients with severe sunken upper eyelid concurrently with blepharoptosis. These patients are characterized by the increased height of eyebrow due to both conscious and unconscious actions of the frontalis muscle arising from the blepharoptosis, which may further aggravate the sunken eyelid. As described here, patients with sunken upper eyelid present with various clinical manifestations such as high or multiple fold, blepharoptosis and skin laxity. Collar et al. [5] reported that it would be necessary to use a simplified methodology based on the classification of sunken eyelid into dermatochalasis and hollowing categories. Based on these reports, we treated our clinical cases of sunken upper eyelid depending on whether there is a concurrent presence of the dermatochalasis or blepharoptosis and then performed the autologous fat grafting using either closed or open technique. Thus, we have successfully treated our cases of sunken upper eyelid.
METHODS
We conducted the current retrospective study in 53 patients who underwent autologous fat grafting for the management of sunken upper eyelid between January 2012 and April 2014. We excluded the patients with sunken upper eyelid arising from previous surgeries or trauma. The study conformed to the Declaration of Helsinki. And patients provided written consent for the use of their images.
The patients underwent preoperative evaluation at front gaze in a sitting position. To do this, we evaluated the pretarsal show, the presence of dermatochalasis, the degree of lipoatrophy and the height of superior sulcus. We measured the degree of blepharoptosis based on the marginal reflex distance 1 (MRD1) and did the levator muscle function using the Berke’s method [6]. For surgical procedures, we performed a surgical design of the most deepest sunken line and additionally did that of superior medial bony recession, commonly known as “A-frame deformity” (Fig. 1). Thus, we divided our clinical series of patients into the two groups: the Group I, comprising the patients who visited us for the correction of sunken upper eyelid only, and the Group II, comprising those who had sunken upper eyelid concurrently with dermatochalasis or blepharoptosis. And we concurrently performed the fat grafting in the patients with blepharoptosis for the following cases: (1) The patients with a sunken depth of > 0.5 cm on preoperative evaluation [7]. (2) The patients for whom it would be difficult to achieve a recovery of the symptoms through the correction of blepharoptosis due to severe orbital fat atrophy on intraoperative view.
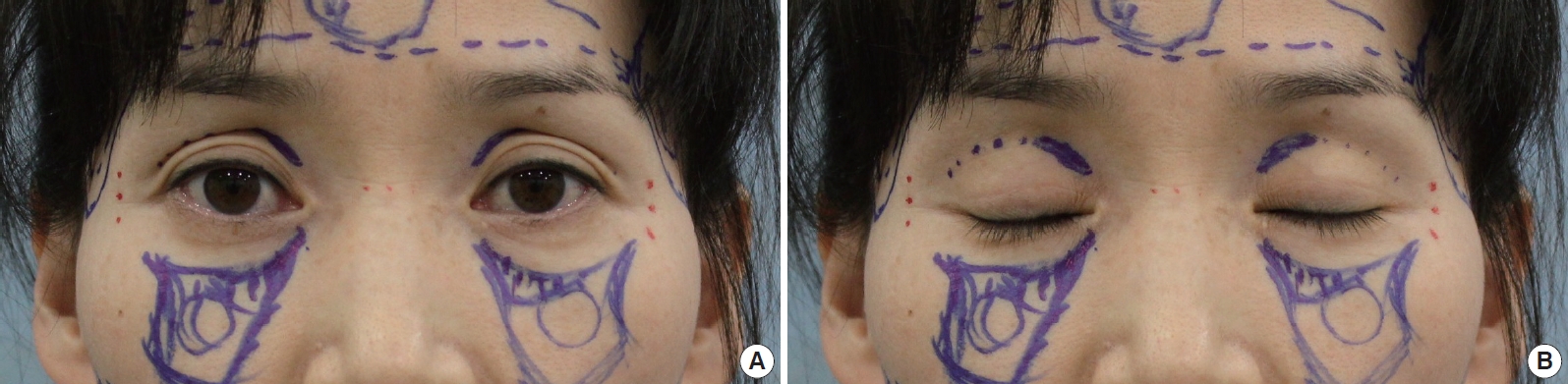
Preoperative surgical design in a 41-year-old patient. (Dotted line) The most deepest sunken line. (Continuous line) The superior medial orbital bony recession. (A) Preoperative surgical design with opened eyes. (B) Preoperative surgical design with closed eyes.
We harvested the fat from the patients placed in a prone position under local or intravenous anesthesia, for which we served the lateral thigh as the common donor site. After making a stab incision on both lateral thighs, we evenly infiltrated a 40 mL of tumescent (20 mL 1% lidocaine and 1 mL 1:1,000 epinephrine in 200 mL normal saline) on the subcutaneous plane using a tumescent infiltrator cannula of 2.0 mm×25 cm in size (Nanum Medical, Seoul, Korea). Twenty minutes later, we harvested the fat using a harvester cannula (3.0 mm×23 cm, Nanum medical, Seoul, Korea) with a 10-mL Luer-Lok syringe. After harvesting a sufficient amount of the fat, we sutured the stab incision using a 5-0 nylon. The harvested fat was centrifuged for 3 minutes at 3,000 rpm, from which the blood, oil and tumescent were discarded. Then, the residual fat was placed in a 1-mL syringe at a volume of 0.5 mL each for further fat grafting procedure.
In the upper eyelid, we induced the local anesthesia using 1% lidocaine with 1:100,000 epinephrine. Then, we performed a meticulous fat transfer for the fat grafting using a micro-injector cannula of 1.0 mm×5 cm in size (Nanum Medical, Seoul, Korea) in order to minimize the occurrence of post-procedural edema. According to the classification of the patients, we used the following injection techniques:
First, we solely performed the autologous fat grafting using the closed technique in the sunken upper eyelid only group, for which we did the injection using a micro-injector cannula on the suborbicularis plane after the puncture of the lateral end of the both sunken deformity using a 23-guaze needle. With the single passage of the cannula, we gently injected the fat at the smallest dose possible using the multiple panning technique for the purpose of preventing the occurrence of the lump. Thus, we also attempted to minimize the occurrence of edema and bruising.
Second, we performed such procedures as skin excision, orbicularis oculi muscle strip excision and levator aponeurosis advancement to manage each symptom in the sunken upper eyelid with dermatochalasis or blepharoptosis group. Simultaneously, we also made a small window in the lateral portion of the orbital septum using the open technique with metzenbaum scissors. Thus, we performed the intraseptal injection of the autologous fat. Similarly to the sunken upper eyelid only group, we performed the injection using the multiple panning technique both gradually and gently, thus attempting to minimize the occurrence of the complications.
During the fat transfer in both groups, if applicable, we recommended the patients to open and close their eyes. Thus, we confirmed the results of the correction and determined the amount of fat transfer. In addition, we converted the posture of the patients into the sitting position, if appropriate, and monitored the procedures of fat transfer.
For one to two days postoperatively, we performed the ice packing for the patients. Moreover, we instructed them not to heavily touch the upper eyelid or compress it with hands. Following the procedure, the residual fat was stored at a temperature of -20°C in a frozen state. Two months after the primary fat grafting, we performed the postoperative evaluation at a follow-up. Thus, we performed the secondary fat grafting at the sites where a greater amount of the fat was absorbed. For the secondary procedure, we dissolved the fat at room temperature after it was stored at a temperature of -20°C in a frozen state. This was followed by the centrifugation for 3 minutes at 3,000 rpm. Following this, we discarded the blood, oil and tumescent. Thus, we completed the secondary fat preparation. Furthermore, we also performed the fat grafting using the same closed technique.
RESULTS
During a period ranging from January of 2012 to April of 2014, we treated a total of 53 patients, all of whom were women. The mean age of the patients was 41 years (range, 23–76 years). We performed the primary autologous fat grafting at a mean volume of 0.7 mL (range, 0.1–2.0 mL) for one eyelid. Of the 53 patients who underwent primary fat grafting, 45 received injections of the fat using the closed technique on the suborbucularis oculi plane (Fig. 2-4). In these patients, the mean age was 40 years and the mean volume was 0.7 mL. In the remaining eight patients, we performed the intraseptal injection using the open technique, where the mean age was 48 years and the mean volume was 0.5 mL. Of the eight patients who underwent intraseptal fat injection, four concurrently did blepharoplasty for the management of the dermatochalasis (Fig. 5, 6). In the remaining four patients, we concurrently performed the levator advancement for the management of blepharoptosis (Fig. 7, 8).

A 50-year-old patient undergoing autologous fat grafting using a closed technique at a volume of 1.1 cc on the left side and 0.9 cc on the right side. (A) Preoperative view. (B) Seventeen months postoperative view.
A 50-year-old patient undergoing autologous fat grafting using a closed technique at a volume of 0.6 cc on both sides. (A) Preoperative view. (B) Nine months postoperative view.

A 42-year-old patient undergoing autologous fat grafting using a closed technique at a volume of 0.5 cc on both sides. Two months thereafter, the patient underwent secondary fat grafting using the fat, stored in a frozen state, at a volume of 0.3 cc on both sides. (A) Preoperative view. (B) One month after the primary fat grafting. (C) Twelve months after the secondary fat grafting.

A 42-year-old patient undergoing blepharoplasty concomitantly with autologous fat grafting using an open technique at a volume of 0.9 cc on the left side and 0.5 cc on the right side. (A) Preoperative view. (B) Three months postoperative view.

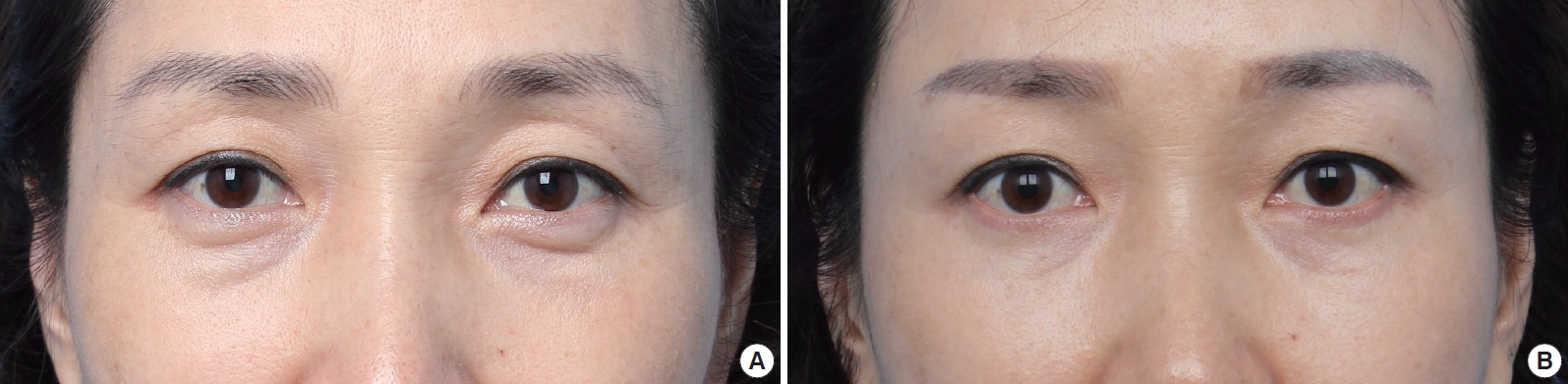
A 56-year-old patient undergoing blepharoplasty concomitantly with autologous fat grafting using an open technique at a volume of 0.5 cc on both sides. Two months thereafter, the patient underwent secondary fat grafting using the fat, stored in a frozen state, at a volume of 0.4 cc on both sides. (A) Preoperative view. (B) Four months after the secondary fat grafting.

A 58-year-old patient undergoing blepharoptosis correction concomitantly with autologous fat grafting using an open technique at a volume of 0.5 cc on both sides. (A) Preoperative view. (B) Three months after the secondary fat grafting.

A 54-year-old patient undergoing blepharoptosis correction concomitantly with autologous fat grafting using an open technique at a volume of 0.3 cc on both sides. (A) Preoperative view. (B) Nine months after the secondary fat grafting.
Of the 53 patients who underwent primary fat graft, 17 (32%) did secondary fat grafting, whose mean age was 45 years. These 17 patients underwent secondary fat grafting at a mean volume of 0.5 mL (range, 0.1–1.5 mL) for one eyelid. Of the 45 patients who underwent fat grafting on the suborbicularis oculi plane using the closed technique, 15 did secondary fat grafting at a mean volume of 0.5 mL. Moreover, of the eight patients who underwent intraseptal injection using the open technique, two did secondary fat grafting at a mean volume of 0.5 mL. Of the patients who underwent secondary fat grafting, one was in need of the fat harvesting. The remaining 16 patients underwent retouching using the fat which was stored in a frozen state.
The patients were followed up during a mean period of four months (range, 2–24 months). At a follow-up, however, there were no patients who developed notable complications such as infection, hematoma, fat embolism and blindness. Two patients developed contour irregularity, who achieved a recovery of the symptoms during the monitoring of the clinical course. There were four patients who developed transient blepharoptosis due to the edema of the upper eyelid. But these patients felt comfortable opening their eyes with the resolution of the edema. Moreover, the patients achieved improvement of asymmetry and undercorrection after undergoing secondary fat grafting two months later. Finally, there were no patients who underwent tertiary fat grafting.
DISCUSSION
Facial aging process has a multi-factorial aspect, and it shows the individual difference. Solar damage causes the fine rhytids and skin thinning [5]. The aging-related weakening of the supporting anatomical structures of lower eyelid causes the lower orbital fat bulge; this may lead to the occurrence of senile fat atrophy and senile enophthalmos [4]. On the superomedial and inferolateral aspects of the orbital rim, the site specific aging-related bone resorption increases the orbital aperture [3]. Due to these various factors, hollowing and skeletonization of the upper periorbital area occurs. This eventually leads to the occurrence of sunken eyelid deformity. Thus, patients complain of tired-looking appearance or dark circle, for which they visited hospitals.
To date, rejuvenation procedures including periorbital rejuvenation have mainly been performed to remove the excess skin or fat or to lift the soft tissue descent due to the gravitational force and atrophic laxity. But these approaches are disadvantageous in that they cause unnatural and surgically created face. With the technical advancement of the autologous fat grafting, rejuvenation procedures have been performed focusing on the volume restoration. Therefore, there are many methods for correcting the sunken upper eyelid. Currently, however, ongoing efforts are made to treat the relevant cases using autologous fat or dermal filler from perspectives of volume restoration [1,5,7-12].
Autologous fat grafting is currently a popular modality in the field of cosmetic and reconstructive surgery. But it is disadvantageous in that it causes a great variability in the survival rate. Therefore, there have been reports about various methods for increasing the survival rate; these include fat harvesting, preparation, injection and storage. With regard to the procedures of the fat harvesting, Rohrich et al. [13] and Li et al. [14] reported that there was no significant difference in the fat grafting between the donor sites, thus reaching a conclusion that it would be better to select easier, safer methods in this series. Moreover, Kurita et al. [15] reported that the optimal centrifugal force was 1,200 g for the fat processing. In addition, Son et al. [16] reported that there were no significant differences in the viability of mature adipocytes and adipose stem cells between the centrifugal force of 2,867.2 g and that of <2,867.2 g. With regard to the fat storage, Li et al. [17] reported that there was no significant difference in the cell viability between the temperatures of -20, -80, and -196°C. Based on these reports, it can be inferred that surgeons may consider our methods based on the lateral thigh as the donor site, the centrifugal force of 1,167 g and the temperature of the fat storage of -20°C.
To date, many methods have been proposed to resolve the sunken eyelid. These include the methods based on the transposition of nasal fat pedicle [18,19], fascia-fat composite graft [20] and dermofat graft [21]. In addition, Park et al. [7] performed the orbital fat repositioning concurrently with the autologous fat graft for the retro-orbicularis oculi fat (ROOF), thus reporting good treatment outcomes. Recent studies have introduced the methods based on the autologous fat grafting only [1,10,11,22] and those using hyaluronic acid [9,23].
For the treatment of sunken upper eyelid, various types of fat injection plane are used for the autologous fat grafting. In association with this, Kranendonk et al. [1] and Kim et al. [10] performed the fat grafting on the subcutaneous plane. Yoon et al. [12] performed the fat grafting in the orbital septum. Kwon et al. [11] performed a multi-layered injection extending from the orbital fat layer to orbicularis oculi muscle. In addition, Park et al. [7] performed the fat grafting for the ROOF layer. Furthermore, Kim et al. [22] performed the injection in the subcutaneous and suborbicularis oculi layer. Collar et al. [5] performed the injection on the suborbicularis oculi plane. In our series, we performed the injection of the autologous fat using the blind technique on the suborbicularis oculi plane if there were no concurrent symptoms. Moreover, we accurately performed the injection in the orbital septum in patients who were in need of the open technique because of the concurrent presence of the symptoms. As described here, we did not use the subcutaneous plane to prevent the occurrence of the lump or irregular contour.
As the complications after the autologous fat grafting, there have been reports about the contour irregularity, fat embolism, asymmetry, infection and fat migration [5]. Of these, the most frequent complication is a contour irregularity due to visible lumps. To prevent the occurrence of these complications, surgeons should avoid performing the injection in the subcutaneous layer, as described above. Moreover, they should ensure that small particles of the fat can be distributed both evenly and homogeneously in the target layer by injecting the fat as minimally as possible with the single passage of the cannula. If not much experienced, surgeons should repeatedly perform the injection of conservative amounts of fat and then gradually elevate the volume of grafting. In patients who had lumps, surgeons should wait for certain periods of time. Unless there are no resolutions, surgeons should consider the intralesional triamcinolone injection (5 mg/mL) [1].
We assume that the treatment goals for the sunken upper eyelid might be to restore the volumetric deficiency of the upper eyelid and to correct the possible concurrent presence of the dermatochalasis or blepharoptosis. There is a possibility that there might be functional problems such as the discomfort with eye opening or aesthetic ones such as the decreased size of the double eyelid following the autologous fat grafting. This leads to the speculation that the autologous fat grafting in the upper eyelid would be different from the fat grafting for other facial regions for which the volume replacement is considered a high priority.
In conclusion, our results indicate not only that surgeons should consider the fat grafting as one of eyelid-surgery procedures but also that they should perform it concurrently with blepharoplasty or blepharoptosis correction for the purposes of obtaining good treatment outcomes.
Notes
This article was presented as the 9th Symposium of Research Society for Lipoplastic and Adipose-Derived Stem cell on September 29, 2013 in Seoul, Korea.
No potential conflict of interest relevant to this article was reported.