Occurrence and Surgical Treatment of Massive Morel-Lavallée Lesion after Large-Volume Liposuction: A Rare Clinical Case
Article information
Abstract
A soft tissue injury can cause the formation of a pseudocyst in the subcutaneous tissue due to a hematoma, seroma, or liquefied fat. These cysts are Morel-Lavallée lesion. A 30-year-old male patient had previously received a large-volume Liposuction. After a couple of years, Morel-Lavallée lesion has formed on the abdomen. So after the two communicating massive sacs were resected, we advanced the upper flap inferiorly and resected a margin of the redundant tissue.
INTRODUCTION
The incidence of morbid obesity remains lower in the population of Asia than in the West, but the numbers are on a steady rise among Asians as a result of the widespread adoption of a high-calorie Western diet. The resultant increase in obese patients has led to a corresponding increase in those wanting to enhance their body shape and contour through aesthetic surgery such as large-volume liposuction. Inevitably, it follows that the incidence of complications directly associated with large-volume liposuction has increased accordingly. Morel-Lavallée lesion is a rare, late complication associated with large-volume liposuction. In this case report, we describe an incident of massive Morel-Lavallée lesion after large-volume liposuction, which was removed through resection and drainage.
CASE
A 30-year-old male patient had a liposuction for morbid obesity (body mass index [BMI] ≥35 kg/m2 in Korean men) in 2014 at a private practice. We did not have detail information on his previous liposuction practice, but through history taking, we have learned that 8,000 cc of fat and fluid was taken out through liposuction and garment was used for 2 weeks after the liposuction.
The patient was admitted to our hospital in 2016 because his abdominal discomfiture and bulging had worsened over time (Fig. 1A and 1B). At the time of admission, the patient’s BMI was 45.9, and no other particularities were seen in the patient save for hypertension. On computed tomography scans, we found a fluid-filled sac with dimensions of 20×22×10 cm on the right anterior abdominal wall and another with dimensions 20×20×9 cm on the left anterior abdominal wall; these two pseudocysts communicated at the inferior umbilicus (Fig. 2A and 2B). We decided to remove the two massive pseudocysts and carry out minimal abdominoplasty at the same time without altering the position of the umbilicus.

(A, B) A preoperative photograph of a 30-year-old male patient with massive pseudocysts in the abdomen.

(A, B) Preoperative computed tomography scans of two communicating (white arrow) pseudocysts at the anterior abdominal wall in the 2-dimensional axial view and in the 2-dimensional coronal view.
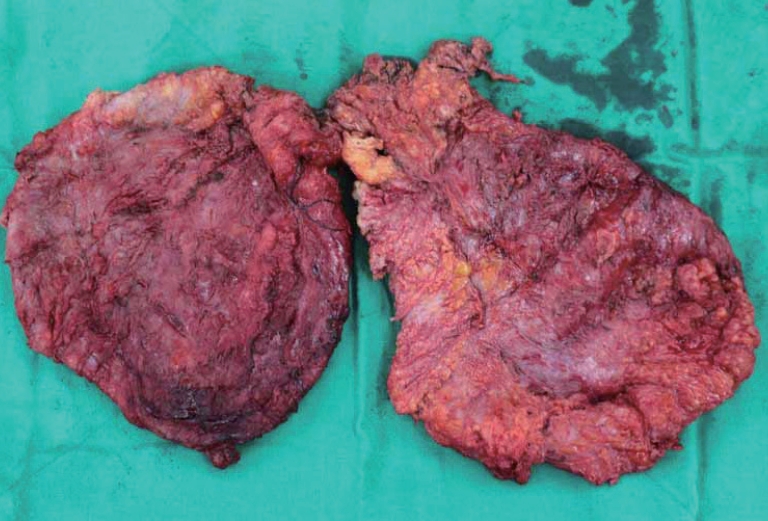
Using a scalpel, we made bilateral skin incisions from the anterior superior iliac spine to a point 2 cm superior to the superior end of the symphysis pubis. The dissection was made in the cephalic direction without compromising the Scarpa’s fascia. When the wall of the massive Morel-Lavallée lesion was reached, we carefully dissected the area surrounding the pseudocyst wall whilst preserving the umbilical stalk (Fig. 3). After the two communicating massive pseudocysts were resected (Fig. 4), we advanced the upper flap inferiorly and resected a margin of the redundant tissue. The total weight of the removed sacs was 3.3 kg, and the thickness of the sac wall was 0.6 mm. Subsequent histopathological results showed that the sac tissue had undergone fibrosis and did not have an epithelial lining. During the first postoperative month of rehabilitation, the patient was instructed to wear a compression garment throughout the whole day for the first two weeks and then only at night for the next two weeks. All drainage was complete within two weeks of the operation. Except for a secondary procedure that was carried out for partial necrosis, which occurred at the skin margin of the repair site, neither recurrence nor complication was observed during the 6-month postoperative follow-up period (Fig. 5).
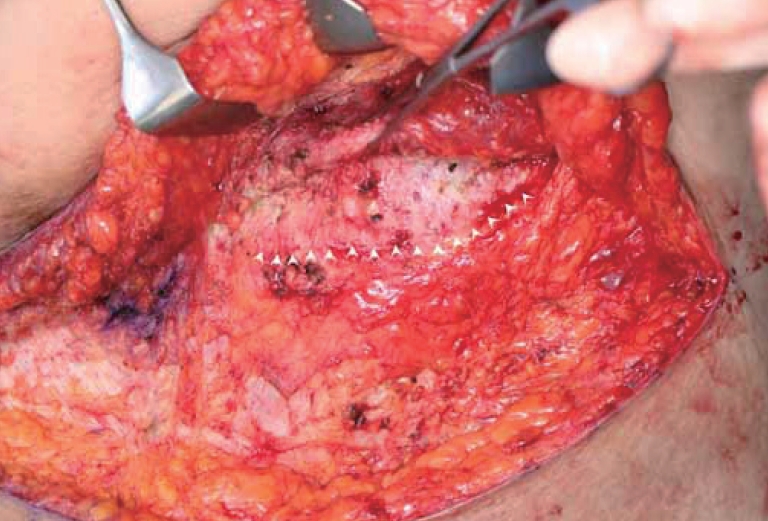
Intraoperative photographs showing the pseudocyst (white arrowheads) located on the patient’s abdominal wall.
DISCUSSION
A soft tissue injury can cause the formation of a pseudocyst in the subcutaneous tissue due to a hematoma, seroma, or liquefied fat. These cysts was first described by a French surgeon, Victor MorelLavallée in 1853 [1]. Subcutaneous fat has 2 layers separated by subcutaneous fascia. Superficial layer has compact network while deep layer has less compact network. Superficial layer has uniform thickness throughout the body regardless of location while deep layer has various thickness and structure specific to body parts and forms deep fatty compartment. This compartment develops more in abdomen, buttock, and thigh, and more in females than males. By such characteristic, Morel-Lavallée lesion is prone to develop more in thigh. Its development in trunk, buttock, lumbar, scapular area are also reported, but generally known it develops unilaterally and more to females [2,3]. Main symptoms are soft-tissue edema, topalgia, hypoesthesia. Morel-Lavallée lesion could be diagnosed within few hours or few days after injury, but took months to years for one third of cases. A differential diagnosis should be made for fat necrosis, pseudolipoma, coagulopathy-related hematoma, soft-tissue tumor. It is also reported that Morel-Lavallée lesion is developed after abdominal liposuction [4]. This may come from multiple separate tunnels and small pockets generated after abdominal liposuction under less tight compression create dead space or the space provides channels for fluids to stagnate in [5,6]. Treatment is relevant to duration, size, presence of a capsule of lesion. Small acute lesions without a capsule can be conservatively treated with application of compression bandage, but more aggressive treatment is required for capsule formed cases. These lesions may need early percutaneous drainage or even excision for cases with large sizes [7]. Also long term compression bandage application is required.
In morbidly obese patients, clinicians often overlook this in liposuction patients because pseudocysts can be difficult to discern or to palpate in patients who, despite surgery, may still have an aboveaverage volume of fat around the abdomen. Thus, a thorough physical examination for potential recurrent Morel-Lavallée lesion is required during the follow-up period in patients who undergo large-volume liposuction. The number of patients receiving large-volume liposuction in Korea is rising. Therefore, the rate at which clinicians will encounter liposuction-associated complications will also increase–a forecast for which we should be prepared. As far as our knowledge goes, the case of postoperative massive Morel-Lavallée lesion after large-volume liposuction reported here has no precedent in Korea. We reported the successful removal of a massive Morel-Lavallée lesion with concomitant minimal abdominoplasty and good clinical outcomes without any major complications or recurrence.
Notes
No potential conflict of interest relevant to this article was reported.
PATIENT CONSENT
Patients provided written consent for the use of their images.