Thermoplastic nipple splint: A simple method of maintaining nipple projection
Article information
Abstract
Maintaining projection of the reconstructed nipple is important for achieving natural and aesthetically appealing outcomes in breast reconstruction. Although various methods of avoiding mechanical force on the reconstructed nipple have been developed, the existing methods are inconvenient, crude, non-reusable, and difficult to clean or adjust. In the present study, a simple method of creating a nipple splint using a thermoplastic material is described. This splint can be easily manipulated, washed, and reused, and it is comfortable to wear for long-term use without any complications and convenient for the patient to apply.
INTRODUCTION
The nipple-areolar complex (NAC) is the most important and integral feature of the breast [1]. Therefore, NAC reconstruction is psychologically important for patients who undergo breast reconstruction and can affect the aesthetic outcomes [2].
The major concern after nipple reconstruction is loss of projection, which has been reported to range from 40% to 75%, regardless of the method [1,3,4]. After the operation, the nipple flap and surrounding tissue start to contract, and intrinsic forces cause the nipple to shrink [5]. In addition, extrinsic trauma to the nipple, such as shearing forces and mechanical compression, can lead to loss of the intact projection.
To prevent shrinkage of the reconstructed NAC, various postoperative dressings have been developed, including doughnut-shaped sponges, plastic syringes, molding casts, and silicone nipple shields [4,6-8]. However, most existing dressings are bulky, cumbersome, and inconvenient to manipulate. In addition, these dressings are non-reusable, expensive, and require fixing materials such as sutures or staples.
To maintain nipple projection more easily, we developed a simple method based on a nipple splint using a thermoplastic material, which we present herein.
IDEA
One piece of 7.6 cm (width)×7.6 cm (height)×1.7 mm (thickness) thermoplastic material (Hexaplast; Splint Lite, Megen, Korea) and a 10-mL syringe plunger were prepared (Fig. 1). All four corners of the square were cut out with scissors to make a round shape, as shown in Fig. 1. The trimmed piece was soaked in 60℃–70℃ water for 10 seconds (Fig. 2A) until it became malleable; then, it was molded into a splint. At the same time, a protrusion was made at the center of the splint using a plunger (Fig. 2B). The radius of the plunger tip was 15 mm, sufficiently wide to protect the reconstructed nipple without touching it (Fig. 2C). When needed, the splint base was resoaked in 60℃–70℃ water for a few seconds to ensure comfortable attachment onto the breast mound (Fig. 3).

Prepared materials for the nipple splint: a trimmed piece of thermoplastic material and a 10-mL syringe plunger.

(A) After soaking the trimmed thermoplastic in 60°C–70°C water for 10 seconds, the plastic becomes malleable and can be readily molded as a splint. (B) The syringe plunger used to create a protrusion in the center of the splint. (C) The protruding section can be sufficiently widened using one’s fingers.
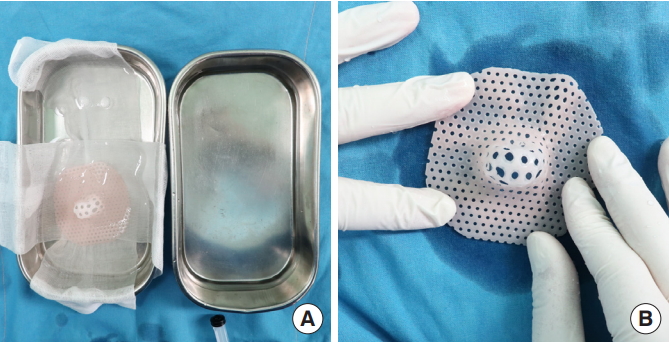
(A) The base of the splint was resoaked in 60°C–70°C water for a few seconds. (B) The base of the splint was adjusted to attach comfortably onto the breast mound.
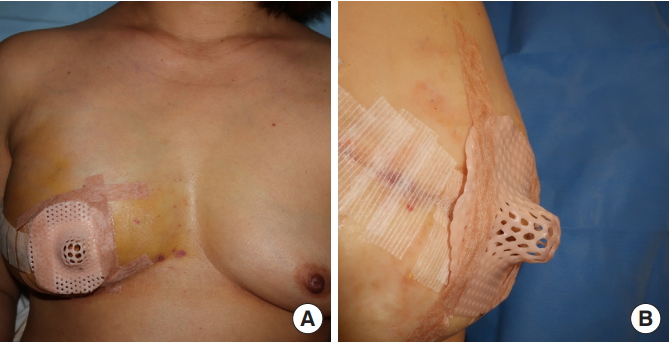
After nipple reconstruction using a modified C-V flap, dressing material was applied to the surrounding donor site and the nipple splint was placed over the nipple and fixed with paper tape (Fig. 4). If the reconstructed nipple was large and touched the splint, the protruding part of the splint was easily adjusted by resoaking it in warm water. After discharge, the patients were able to easily change the dressing by themselves. The nipple splint was semi-permanent, washable, and cleanable with an alcohol swab mounted on a stick.
DISCUSSION
For a reconstructed nipple to have an aesthetically natural appearance, the three-dimensional projection of its structure is important [9]. Both intrinsic and extrinsic mechanical forces applied to the reconstructed nipple cause difficulty in maintaining the projection of the nipple. Tissues surrounding the donor site start to retract, and their tension causes the reconstructed nipple to shrink [5].
Although numerous surgical methods, including the insertion of allogenic acellular dermis under the flap, have been developed to avoid the loss of projection [3], most trials have been unsuccessful. Extrinsic forces including gravity, direct compression, and shearing forces also decrease the projection. To maintain prolonged projection of the reconstructed nipple, both intrinsic and extrinsic factors should be addressed.
Various postoperative dressings have been reported to protect reconstructed nipples, including nipple shields filled with antibiotic ointment, silicone nipple shields, plastic guards, doughnut-shaped sponges, bolster dressings, adhesive eye protectors, thermoplastic casts, and syringe nipple splints [4,6-8]. However, many of these dressings can easily become dirty, are bulky, inconvenient, costly, often uncomfortable for patients, difficult to correct, and require suturing to be fixed. In addition, some ready-made products are difficult to manipulate for surgeons and might not fit the patient’s nipple or breast shape.
The thermoplastic nipple splint has many benefits over previous methods, including low cost, ease of manipulation, and the possibility of long-term use; patients can use it semi-permanently until the reconstructed nipple becomes stable, and again if a second operation is performed. During this period, no complications such as the occurrence of ulcers or new wounds, including skin problems, were observed. This is not only because of the inherent elasticity and softness of the material, but also because of its comfortable contact with the breast mound through the molding.
In addition, patients can easily manage the splint, wear it comfortably, and clean the splint without any medical help or specialized equipment. Lastly, the shape of the splint can be easily adjusted with projections similar to the size of the reconstructed nipple, and the splint boundary can be molded to fit the breast mound.
Notes
No potential conflict of interest relevant to this article was reported.
Ethical approval
The study was performed in accordance with the principles of the Declaration of Helsinki.
Patient consent
The patient provided written informed consent for the publication and the use of her images.