Comparative study of the prevention of seroma formation in immediate breast reconstruction with latissimus dorsi myocutaneous flaps
Article information
Abstract
Background
Latissimus dorsi (LD) flaps are often used in breast reconstruction procedures, but seroma formation is a frequent complication. To decrease the incidence of seroma formation, fibrin sealants and/or quilting sutures have been proposed, with controversial results. The primary objective of this study was to assess the effectiveness of the Harmonic scalpel in association with Tisseel and three-point deep dermal sutures in reducing the incidence of this complication.
Methods
A retrospective study was conducted of 108 patients undergoing immediate unilateral breast reconstruction with LD flaps over a 3-year period (2016–2018) by a single surgeon. In the experimental group, 37 patients underwent the procedure with a Harmonic scalpel and three-point deep dermal sutures (a modified version of quilting sutures), and the other 71 received conventional electrocautery. Fibrin sealant was applied to the donor site of all patents to reduce seroma formation.
Results
Statistically significant differences in the incidence of seroma were found between the two groups. There was a lower incidence of seroma formation in the group of patients treated with a Harmonic scalpel and three-point deep dermal sutures than in the other group. The total drainage amount and drain removal date between the two groups were not significantly different.
Conclusions
Within the limitations of this study, we suggest that Harmonic scalpel use can be a good choice among the many ways to reduce seroma formation following LD flap procedures, and that this technique will be very helpful for patients.
INTRODUCTION
Breast cancer, which is one of the most common cancers in Korean women, represents 14.8% of all newly diagnosed cancers and its proportion among all cancers is gradually increasing [1]. Many surgical procedures have been introduced for the reconstruction of breast defects after breast cancer surgery to address patients’ aesthetic and psychological concerns. These procedures can be broadly classified as autologous and prosthetic reconstructions. Myocutaneous flaps using the latissimus dorsi (LD) muscle are widely used because their high vascularity and flexibility, which make it easy to control the shape. However, LD myocutaneous flaps pose a risk of donor site morbidity on the back [2,3]. The most common complication is seroma, the incidence of which has been reported to range from 1% to 56% in previous studies [4,5].
Patients with seroma complain of serious discomfort and pain, infections, and wound dehiscence, and discomfort can result from seromas that are lump-like. Despite the high incidence of seroma, little information has been reported on the risk factors associated with seroma formation at the donor site. In several studies conducted to identify the risk factors for seroma, body mass index (BMI), smoking, specimen weight, surgical technique, and age were consistently reported to have significant relationships with donor site seroma [6,7]. Many studies have evaluated surgical techniques as controllable risk factors. Typical techniques include the use of quilting sutures at the donor site and the use of fibrin sealant. A meta-analysis of the effects of fibrin sealant and tension sutures on preventing seroma formation suggested that the use of both is effective [8]. However, this conclusion remains controversial, and further investigations into seroma formation are warranted.
It has come to our attention that the Harmonic scalpel (Ethicon Endo-Surgery, Inc., Cincinnati, OH, USA) is widely used in other surgical fields, such as general surgery and otorhinolaryngology. The Harmonic scalpel has the advantage of being able to resect tissues more accurately than is possible using electrocautery. In addition, less smoke is generated during surgery, the operative time is shorter, heat damage to the surrounding tissues is reduced, and more certain hemostasis can be achieved [9]. In recent years, a number of studies related to the effects of Harmonic scalpels have been published. According to these reports, the use of Harmonic scalpels in breast surgery, including mastectomy and lymph node dissection for breast cancer patients, reduced the incidence of postoperative bleeding and seroma formation [9-12]. To date, however, research on the effects of Harmonic scalpels to prevent seroma formation when LD myocutaneous flaps are used for breast reconstruction has been published in the United States, but not in Korea [13].
In this study, by comparing the incidence of seroma formation, the total amount of drainage, and the timing of drain removal after breast reconstruction, we intended to clarify the effect of using a Harmonic scalpel and three-point deep dermal sutures (a modified version of quilting sutures) at the donor site.
METHODS
Study design
Data were collected by chart review. This retrospective study examined data over a 3-year period from January 2016 to December 2018. A total of 153 patients who underwent immediate breast reconstruction performed by a single surgeon were reviewed. Thirty patients with missing or inaccurate data and 15 patients who were outliers in terms of risk factors (age, BMI, and the amount of tissue surgically extracted) were excluded.
Each patient underwent immediate breast reconstruction with an LD myocutaneous flap after nipple-sparing or skin-sparing mastectomy. None of the patients had a smoking history or a history of radiotherapy in the area prior to surgery.
In the control group (group A), fibrin sealant was used to seal the donor sites to reduce the incidence of seroma formation during surgery. In the experimental group (group B), in addition to fibrin sealant, a Harmonic scalpel was used to dissect and elevate the LD myocutaneous flap from the back. Three-point deep dermal sutures were used to close the donor sites in this group.
We thoroughly checked every patient’s preoperative data, including their preoperative BMI, coagulation disorder status, and history of drug-specific reactions, pregnancy, and systemic diseases. Patients with an excessively high BMI (>35 kg/m2), a preoperative history of using steroids or anticoagulants, or systemic diseases were excluded, as well as those who were pregnant or breastfeeding.
During the operation, the total weight of the excised breast tissue was measured with a consistently used scale. In every patient, the sentinel lymph nodes and axillary lymph nodes were removed. Two 200-mL Jackson-Pratt (Barovac; Sewoon Medical, Seoul, Korea) tubes were inserted into the LD muscle donor site. One tube was located in the LD muscle and the other was located in an axillary dissection donor site on the back. We always applied two drains to the donor site. The drains were removed when the amount of drainage was less than 30 mL for 2 consecutive days. The drainage amount on postoperative days (POD) 1 and 2, the timing of drain removal, and the incidence of seroma formation were collected and analyzed. To analyze and minimize the bias resulting from the effects of risk factors for seroma, data such as patients’ age, the breast specimen weight, BMI, and history of smoking were collected and analyzed.
Drainage amount was calculated only from the two drains in the back donor site. We defined seroma formation as fluid collection observed visually or ultrasonographically at the donor site after drain removal.
A Harmonic scalpel was used to dissect and elevate the LD muscle from the deep muscle of the back, rather than using an electric coagulator (Fig. 1).

The appearance of a Harmonic scalpel (Ethicon Endo-Surgery Inc., Cincinnati, OH, USA). It is an ultrasound resection method that enables hemostasis at the same time as tissue resection by using high-frequency mechanical vibrations ranging from 20,000 Hz to 60,000 Hz.
Fibrin sealant was divided into two separate syringes, one containing fibrinogen and the other one containing thrombin. We sprayed 4 mL of aerosolized fibrin into the back donor site before performing three-point deep dermal sutures (Fig. 2). Mixing the two components resulted in a viscous glue as thrombin converted fibrinogen into fibrin. A meticulous dressing was applied to the operative site every day.
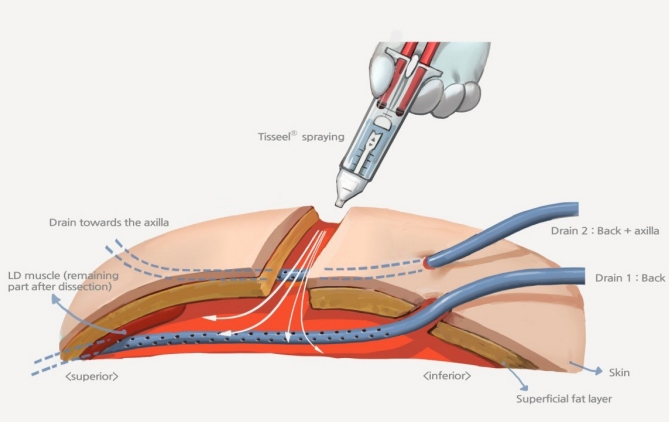
Insertion of two 200-mL Jackson-Pratt drains at the latissimus dorsi muscle donor site alone and at a donor site with the axillary dissection site on the back. Fibrin sealant was sprayed after drain insertion.
The three-point deep dermal suture technique, which is a modified version of quilting sutures, was used to attach the superficial fat layer to the bed of the removed part of the deep fat layer and the muscle with absorbable threads (Fig. 3). The interval between each thread was 2 cm. Fibrin sealant was applied to minimize the dead space that was formed after elevation of the LD muscle.
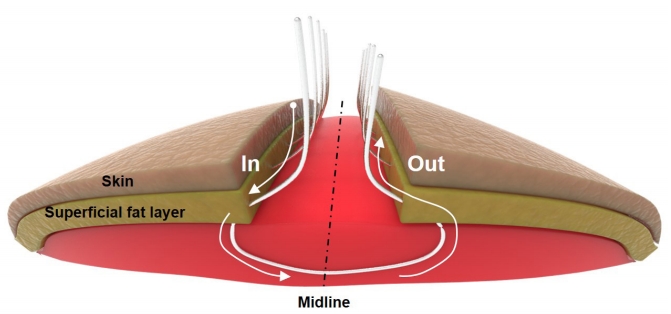
Technique of three-point deep dermal sutures. The superficial fat layer was attached to the bed of the removed part of the deep fat layer and muscle with absorbable threads.
After discharge, the formation of seroma in all patients was assessed at visits to the outpatient department two or three times a week. The patients with drain tubes who were discharged received education on how to measure and record the amount of drainage at home. All patients received a final check for seroma formation at an outpatient visit 1 month later.
Statistical analysis
The normality of the distribution of the collected data was analyzed. If the data were normally distributed, the mean values between the two groups were compared. The mean differences in variables such as age were analyzed between the two groups using the independent t-test. If the data were not normally distributed, as was the case for specimen weight and BMI, we compared differences in median values using the Mann-Whitney U test. For nominal scales, such as seroma incidence, the Fisher exact test was used to analyze differences between the two groups. In addition, the results were analyzed again using propensity score-matching to minimize the effect of bias. SPSS version 26 (IBM Corp., Armonk, NY, USA) was used for all data analyses. A P-value below 0.05 was considered to indicate statistical significance.
RESULTS
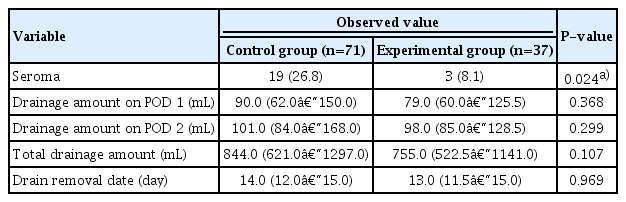
The total number of patients in this study was 108, including 71 patients in group A, in which the Harmonic scalpel and the tension technique were not used, and 37 patients in group B, in which the Harmonic scalpel and tension sutures were used. The average age of the patients was 47.8 years in group A and 45.9 years in group B. The median BMI and the amount of surgically removed tissue, which are factors that might have affected the results, were 25.3 kg/m2 and 355.0 g, respectively, in group A and 22.4 kg/m2 and 379.0 g in group B (Table 1).

Risk factors affecting seroma formation between the experimental and control groups (before propensity score-matching)
We compared the amount of drainage on POD 1 and 2, the total amount of drainage, and the time to removal of the drain. The median amounts of drainage on POD 1 and 2 in group A were 90.0 mL and 101.0 mL, respectively, and the median total amount was 844.0 mL. The median amounts of drainage on POD 1 and 2 in group B were 79.0 mL and 98.0 mL, respectively, and the median total amount was 755.0 mL. The initial and total amounts of drainage were lower in group B, but the differences were not statistically significant (P=0.368, P=0.299, and P=0.107, respectively). The drains in group B were removed slightly earlier than those in group A, but the difference in timing was not statistically significant (P=0.969).
However, the most important outcome was the incidence of seroma formation, which was significantly lower in group B (n=3, 8.1%) than in group A (n=19, 26.8%) (P=0.024) (Table 2).
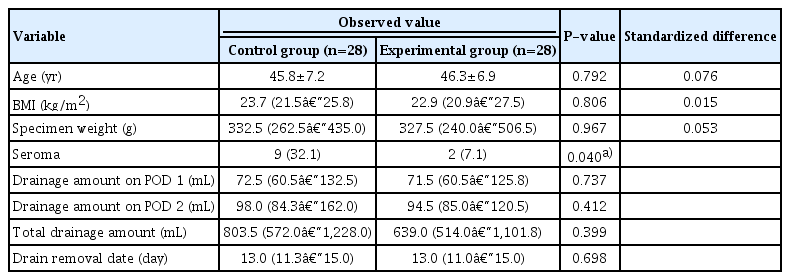
The results were analyzed once again using propensity scorematching to minimize the effect of bias. The mean and median values were compared for 28 patients in the control group and 28 in the experimental group, classified by matching variables (Table 3). In the propensity score-matched sub-analysis, the median amounts of drainage on POD 1 and 2 in group A were 72.5 mL and 98.0 mL, respectively, and the median total amount was 803.5 mL. The median amounts of drainage on POD 1 and 2 in group B were 71.5 mL and 94.5 mL, respectively, and the median total amount was 639.0 mL. The initial and total amounts of drainage were lower in group B, but the difference was not statistically significant (P=0.737, P=0.412, and P=0.399, respectively). There was no difference between the two groups in the time to drain removal, which was 13.0 days in both groups (P=0.698). However, the incidence of seroma formation was significantly lower in group B, where there were two cases (7.1%), than in group A, with nine cases (32.1%) (P=0.044).
DISCUSSION
Immediate breast reconstruction is being performed increasingly often after breast cancer surgery to compensate for changes in breast volume. This study analyzed a comparatively large patient pool of more than 100 patients who underwent immediate breast reconstruction surgery using an LD myocutaneous flap. Of particular note, this is the first study in Korea, with a relatively large patient pool, to investigate the effects of three-point deep dermal sutures and the Harmonic scalpel on postoperative complications after breast reconstruction with LD flaps.
Several mechanisms have been proposed to explain seroma formation after surgery. The donor site of the LD myocutaneous flap may have hidden bleeding after flap elevation and dissection, and prolonged lymphatic leakage may cause fluid collection. Furthermore, the shearing forces generated by the constant movement of the patient may disrupt the coaptation between the skin and subcutaneous tissue [14]. Wound dehiscence can occur after seroma formation, which not only makes patient movement uncomfortable, but also increases the infection rate [15]. Several studies have reported methods to overcome this problem, including intra-operative electrocautery, endoscopic harvesting, compression garments, repetitive aspiration, sclerotherapy, steroid injections, prolonged drainage, and capsulectomy. However, no procedure has shown a marked effect [16].
Research has been conducted on the effectiveness of fibrin sealants and quilting sutures as a way to reduce the incidence of seroma formation. According to Jain et al. [17], the use of fibrin sealant in breast surgery reduced seroma occurrence. However, the studies by Llewellyn-Bennett et al. [18] and Miri Bonjar et al. [19] suggested that using fibrin sealant alone was not effective. On the back, very strong shearing forces between the skin and the muscles in a wide area can result from the patient’s movement. Because fibrin sealant has a weaker effect on the back than in internal organs or vessels with small ranges of movement, additional ways to supplement its effect are needed.
Several studies have investigated seroma prevention by the use of quilting sutures alone or in combination with fibrin sealant [8,20, 21]. These studies have shown that quilting sutures were effective in reducing the incidence of seroma formation, and using them in combination with fibrin sealant augmented their effectiveness. The adhesion of tissue through quilting sutures minimizes the dead space and the occurrence of shearing forces between the skin and subcutaneous tissue [8]. Although quilting sutures have advantages, this technique prolongs the operation time, which can affect the rate of seroma formation. This technique is performed by making through-and-through sutures from the external skin to the bed. Therefore, we considered a modified version of quilting sutures (three-point deep dermal sutures) to minimize the dead space, while also reducing the operation time.
It is thought that performing sutures in an incorrect position or using an improper method will cause discomfort or pain to the patient. Therefore, we design the point at the midline of the back for sutures as accurately as possible, with the patient positioned perpendicularly to the operating table in the decubitus position, and the upper extremity of the affected side is attached to the body for adduction.
In addition to the use of fibrin sealant and three-point deep dermal sutures, this study considered ways to further reduce the risk of seroma formation. In many recent surgical procedures, devices for resection using high-frequency mechanical vibrations have been developed and used. A typical example is the Harmonic scalpel, an ultrasound cutting device. Whereas conventional electrocautery causes thermal damage to the surrounding tissue and imperfectly blocks blood and lymphatic vessels, the Harmonic scalpel is an ultrasound resection method that provides hemostasis at the same time as resection of the tissue by using high-frequency mechanical vibrations ranging from 20,000 to 60,000 Hz [22]. Many recent studies of the Harmonic scalpel have described its use in breast surgery, including for mastectomy and lymph node dissection, and reported that it reduced postoperative bleeding and seroma formation [9-12].
LigaSURE Precise (Valleylab, Boulder, CO, USA), which uses both electrical energy and pressure for ligation and resection of tissue, was also considered for the prevention of seroma formation. A previous study reported that both the LigaSURE and the Harmonic scalpel were safe to use, but the Harmonic scalpel significantly decreased the operation time and length of hospital stay compared to the LigaSURE device [23].
To date, only one study on the effects of the Harmonic scalpel on seroma formation and complications in breast surgery using LD muscle flaps has been reported in the United States [16]. According to Longo et al. [13], when comparing and analyzing the total amount of drainage after the operation and the timing of drain removal, the use of the Harmonic scalpel was effective in reducing complications after surgery. This study was not able to compare and analyze the operation time due to the unavailability of accurate data. Nonetheless, several studies have reported that Harmonic scalpel use reduced both the operation time and postoperative complications [24,25].
A significantly lower rate of seroma formation was found in the experimental group (8.1%), in which the Harmonic scalpel and tension sutures were used, than in the control group (26.8%). Although not statistically significant, the total amount of drainage was less and the time until drain removal was also shorter. In this study, both the Harmonic scalpel and three-point deep dermal sutures were used in the experimental group. Further study is needed to determine whether the Harmonic scalpel was effective, or whether the already-known effect of three-point deep dermal sutures was sufficient. However, this study is meaningful as it is the first study to add Harmonic scalpel use to the use of three-point deep dermal sutures and fibrin sealant, which are already known to be effective measures for reducing the incidence of seroma formation.
Although this study controlled relevant risk factors through propensity score-matching, a limitation is that it was a retrospective analysis, not a prospective study.
Therefore, in the future a large prospective, randomized, double-blind study is needed to obtain more reliable results on the effects of the Harmonic scalpel in reducing seroma formation and other complications in breast reconstruction using LD myocutaneous flaps.
The Harmonic scalpel is already widely used in various surgical fields, and reduces operation time and postoperative complications compared to conventional electrocautery. Many studies have also shown that tension sutures are effective in reducing seroma incidence in breast reconstruction using LD myocutaneous flaps.
Although several efforts have been made to reduce the rate of seroma formation after the use of LD flaps for breast reconstruction, seroma formation is important to minimize because it causes great pain to patients. Therefore, further research is needed to address this problem. Although there are some limitations to this study, we believe that the using a Harmonic scalpel can be a good choice to reduce seroma formation following LD flap procedures and that this technique will be very helpful for patients.
Notes
No potential conflict of interest relevant to this article was reported.
Ethical approval
The study was and performed in accordance with the principles of the Declaration of Helsinki.
Patient consent
The patient provided written informed consent for the publication and the use of her images.