Evaluation of Elastic Lift for Neck Rejuvenation
Article information
Abstract
Background
The neck is not only the first area to show aging but it also represents the persona of the individual. The understanding of the aging process of the neck is essential for neck rejuvenation. The purpose of this study was to evaluate the outcomes and safety of elastic lift in relation to neck region lifting.
Methods
Forty-seven patients with sagging and laxity of the neck skin treated by elastic lift were enrolled in this study from November 2015 to February 2016. To evaluate the safety of elastic lift, a retrospective chart review was conducted. We used an automatic skin diagnosis system to evaluate the efficacy of elastic lift.
Results
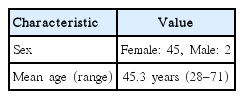
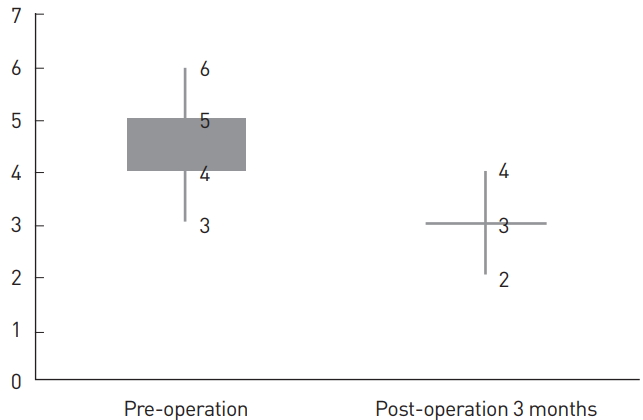
Forty-five patients were female and 2 patients were male. The mean age of the patients was 45.3 years and their mean follow-up period was 3 months. There were no major complications requiring the removal of the elastic thread during the follow-up period. The median skin laxity grade score was 5 (4-5) preoperatively; the median skin laxity grade score was 3 at 3 months postoperatively. In comparing the skin grade score at these two points in time, there was a statistically significant difference (P < 0.01).
Conclusions
Neck rejuvenation using elastic lift is a safe and effective procedure in selected patients with moderate sagging and laxity of the neck skin.
INTRODUCTION
The neck is not only the first anatomical area to show aging but also contributes to the persona of the individual. The understanding the aging process of the neck is essential for neck rejuvenation.
Multiple neck rejuvenation techniques have been reported in the literature. In 1974, Skoog [1] described the anatomy of the superficial musculoaponeurotic system (SMAS) and its role in the aging of the neck. Recently, many patients have expressed interest in minimally invasive surgery with a low risk of complications and short recovery period. The use of thread for neck rejuvenation and the concept of the suture suspension neck lift have become widespread as a convenient and effective procedure; nevertheless, complications have also been reported such as recurrence, inadequate correction, and palpability of the sutures.
In this study, we analyzed a new type of thread lift: elastic lift that uses elastic thread (Elasticum®; Korpo SRL, Genova, Italy). We already use this new technique for the midface lift and can confirm its efficacy and safety in that context. The purpose of this study was to evaluate the outcomes and safety of the elastic lift technique for neck region lifting.
METHODS
Of the patients who underwent neck rejuvenation using elastic lift between November 2015 and February 2016, 47 patients who could be observed and followed for longer than 3 months were enrolled in this study. Patients who had active systemic or local infections, local skin disease that might alter wound healing, a history of psychiatric illness, or soft tissue augmentation material were excluded from this study.
The medical charts and operative records of the participants were reviewed retrospectively to evaluate postoperative outcomes and complications. The study conformed to the Declaration of Helsinki. Written consent was obtained from each patient for both the operation and publication of the photographs of the results.
Elastic thread
The elastic thread used was nonabsorbable suture material (Elasticum® [Korpo SRL]) and a two-tipped long needle (Jano needle®). Elasticum is composed of silicone and sheathed with polyester in a braided fashion which continues to the center portion of the needle. On the needle, there are scale marks which enable the surgeon to measure the distance from the skin into the soft tissue during the procedure.
Surgical procedure
Preoperative design
The preoperative design was applied with the patient seated in an upright position. We drew two lines from the earlobe junction: the first line running to a point near the angle of the mandible where the posterior margin of the platysma muscle runs through the mandible border, and the second line running more inferiorly and at greater length to the platysma muscle’s margin.
Surgical technique
All operations were performed under conscious sedation. Local anesthesia with 2% lidocaine and 1:100,000 epinephrine was infiltrated into both incision sites and along the previously designed line. We began by performing a 2-cm incision at the posterior region of the earlobe, which was located in the tympanoparotid fascia posteriorly. Sharp Metzenbaum scissors were used to dissect caudally and anteriorly to the preauricular region. The tympanoparotid fascia is a fibrous structure that provides a suitable point of anchorage for the elastic thread. The incision and dissection was carried out symmetrically in the contralateral region. A small incision was made with a No.15 blade in the center of the preoperative design line between the submental region and the anterior cervical region. A 16.5-cm Jano needle® was passed superficially from the incision of the earlobe posteriorly to the preauricular region. The needle was then extracted at the preauricular region until about 5 mm of the tip remained in the tissue and the elastic thread had been pulled through. The needle was next rotated towards the previous small incision in the central region of the neck. The needle was passed through the tympanoparotid fascia at the preauricular region in order to anchor the elastic thread. The needle was then passed along the line drawn previously. The surgeon moved the needle up and down slightly to check that it was progressing at the correct depth. The thread must not be implanted too superficially. The Jano needle emerged from the small incision made in the central region of the neck, and the elastic thread was pulled through. The tip of the needle was then reinserted into the small incision, and the needle was passed back to the postauricular incision following a pathway a few centimeters below the previous one. The needle emerged from the incision in the postauricular region. A loop was formed as the elastic thread returned (Fig. 1). The same procedure was performed in the contralateral region. The needle was inserted under the line of the preoperative design between the submental and anterior cervical regions. The elastic thread was pulled through, and the needle was completely withdrawn from the small central incision. The needle was then passed through the loop formed by the first thread and returned in the opposite direction along a pathway a few millimeters below the first one.
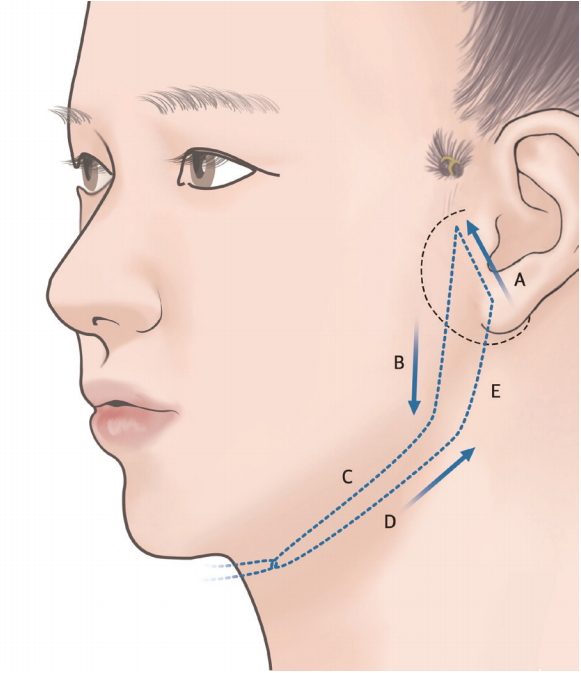
Schematic drawing of the operative procedure. The dotted line indicates the range of dissection. The operative procedure was conducted in the following order: A→B→C→D→E.
The two threads placed in opposite directions were put under traction simultaneously by the surgeon and surgeon’s assistant. Once the thread was pulled, it was knotted. Because this was a minimally invasive procedure, the surgical field where the thread was anchored was not fully visible. Almost blindly, about 1 cm of the thread was anchored to the tympanoparotid fascia, and the surgeon then pulled the thread to ensure that it was secure. The traction exerted by the elastic threads recreated a pleasing cervical angle. When the patient had remarkable fat deposition, we performed liposuction. The incisions at the postauricular area were sutured with No. 6-0 nylon. The head was wrapped with a 3-inch elastic bandage, and the patient was taken to the recovery room.
Evaluation of outcomes
We evaluated the patients using an automatic skin diagnosis system (A-One Lite®; Bomtech Electronics Co., Seoul, Korea) before surgery and 3 months after surgery. The automatic skin diagnosis system evaluates skin laxity using a skin scanner. The sagging and laxity of patients were graded from 1 to 6 using the automatic skin diagnosis system. A high skin grade score means severe sagging and laxity of patient skin.
Statistical analysis
Statistical analyses were performed using SPSS Statistics for Windows version 20.0 (IBM Corp., Armonk, NY, USA). The Wilcoxon signed rank test was used to compare the grade scores of patients before surgery and 3 months after surgery. A P-value less than 0.05 was considered statistically significant.
RESULTS
Of the 47 patients that were treated using elastic lift, 45 patients were female and 2 patients were male. The mean age of the patients was 45.3 years (range, 28–71 years) and their mean follow-up periods were 3 months (range, 3–4 months) (Table 1). Six patients immediately presented mild postoperative asymmetry. This was corrected by slight compression therapy.
There were no major complications that would have required the removal of the elastic thread during the follow-up period (Fig. 2-4). Ecchymosis was the most frequent minor complication, in 19 patients (40%). This ecchymosis disappeared after a maximum of 3 weeks and did not require any treatment. In 10 patients (21%), a small amount of bleeding showed immediately after the insertion of the thread in the subcutaneous layer. This was treated by mechanical compression. All of the patients were able to return to their daily activities 3 days after surgery.

(A) A 48-year-old female patient with moderate skin sagging and wrinkling. Preoperative frontal photographic findings. The patient was examined by an automatic skin diagnosis system and a skin grade score was assigned (left). Three months after surgery: postoperative frontal photographic findings (right). (B) Preoperative oblique photographic findings (left). Postoperative oblique photographic findings (right). (C) Preoperative lateral photographic findings (left). Postoperative lateral photographic findings (right).

(A) A 29-year-old female patient with mid-skin sagging. Preoperative frontal photographic findings. The patient was examined by the automatic skin diagnosis system and a skin grade score was assigned (left). Three months after surgery, postoperative frontal photographic findings (right). (B) Preoperative oblique photographic findings (left). Postoperative oblique photographic findings (right). (C) Preoperative lateral photographic findings (left). Postoperative lateral photographic findings (right).

(A) A 71-year-old female patient with severe skin sagging and wrinkling. Preoperative frontal photographic findings. The patient was examined by an automatic skin diagnosis system and a skin grade score was assigned (left). Three months after surgery, postoperative frontal photographic findings (right). (B) Preoperative oblique photographic findings (left). Postoperative oblique photographic findings (right). (C) Preoperative lateral photographic findings (left). Postoperative lateral photographic findings (right).
The median skin laxity grade score was 5 (4-5) preoperatively; the median skin laxity grade score was 3 at 3 months postoperatively (Fig. 5). The skin grade score improved statistically significantly between the two points in time (P<0.01).
DISCUSSION
Since Sulamanidze and Sulamanidze [2] suggested a minimally invasive procedure for face rejuvenation using bidirectional barbed sutures, numerous procedures have been developed. In 1976, Mitz and Peyronie [3] defined SMAS and developed the SMAS lift and soft tissue repositioning. In the 1980s, Dedo [4] suggested a classification for anatomic assessment of the neck. Feldman [5] introduced corset platysmaplasty in 1990, after which Giampapa et al. [6] utilized minimally invasive surgery by submental and postauricular incision in order to use permanent interlocking sutures. Patients prefer convenient surgical treatments that require only a short recovery time, which has spurred the development of new techniques in aesthetic surgery, especially for the neck lift, with a focus on more minimally invasive techniques [7].
Existing short scar neck lift techniques using thread suturing have had some complications such as persisting skin laxity, inadequate correction, and palpability of the sutures [8]. Stuzin et al. [9] also noted that the thread suture could tear the SMAS layer if the sutures had been inserted under tension.
Recently, not only neck lift using thread, whether invasive or not, but also other simple methods, such as liposuction, microfocused ultrasound (MFU), botulinum toxin, or dermal fillers, have been developed. However, liposuction is of limited value because of the fibrotic character of the neck lift area and difficulty of the technique in a deeper plane. Botulinum toxin or dermal fillers are just alternative methods for skin tightening and not long-lasting techniques [10-12].
The elastic lift has the advantage of longevity, convenience, and efficacy in comparison to previous methods. First, the elastic thread is composed of nonabsorbable suture material covered with polyester. The polyester surface is braided, not barbed, so the surrounding connective tissue grows into the interstices of the braided suture much like a ligament [13]. Therefore, more sustained elevation of the ptotic soft tissue was achieved using elastic thread. Second, elastic thread can be readily removed because the surface is braided, not barbed, up to 2 weeks post-surgically. Third, an elastic lift is more effective in repositioning the soft tissue. Previous thread lifting involved suspension of the ptotic soft tissue using barbed sutures, but in elastic lifting, the silicone’s elastic character repositions the soft tissue. In our experiences of mid-face lifting using elastic threads, all of the patients were satisfied with their results and there were no major complications during the follow-up period. Furthermore, objective results using a skin laxity grade score were improved postoperatively [14].
The elastic lift has many advantages, but it should not be used in all cases. An elastic lift is a minimally invasive surgical procedure that uses just a few sutures, so excision of redundant skin should not be necessary. Therefore, patients who have severe skin sagging cannot be treated by elastic lift. Because the lower portion of the soft tissue is repositioned upward and more laterally, it is recommended that patients with retrognathia not undergo elastic lift. For that reason, patient selection is very important. In our experience, elastic lifting is best indicated for a patient who does not need redundant skin excision.
Our study has two limitations. First, we excluded patients with severe skin sagging. These patients underwent more invasive procedures because elastic lift should not be used with redundant skin excision. Second, our study had a brief follow-up period. Longer follow-up will be needed to confirm a definite effect and the longevity of elastic lift. Despite these limitations, elastic lift is very effective and safe for neck rejuvenation, and this is the first study of elastic lift on the neck area that has been published.
CONCLUSIONS
Although further long-term studies are required to confirm the efficacy and longevity of elastic lift, neck rejuvenation using elastic lift is an effective and safe procedure in selected patients.
Acknowledgements
This work was supported by the Soonchunhyang University Research Fund.
Notes
No potential conflict of interest relevant to this article was reported.
PATIENT CONSENT
Patients provided written consent for the use of their images.