Preliminary results of alternative treatment for postmastectomy pain syndrome: stromal vascular fraction-enriched fat grafting
Article information
Abstract
Postmastectomy pain syndrome (PMPS) is defined as chronic pain lasting more than 3 months after surgery. PMPS reduces the quality of life for patients and affects their daily life. Although the pathogenesis of PMPS has not been clearly elucidated, it is strongly suggestive of neuropathic pain caused by damage to the intercostobrachial nerve. While previous studies have used stromal vascular fraction (SVF)-enriched fat grafts in patients with neuralgia, few studies have used it for PMPS. Therefore, the present study evaluated the use of SVF-enriched fat, which includes adipose-derived stem cells with good differentiation capacity, in patients with PMPS to improve quality of life and reduce neuropathic pain. In three patients, the fat was mixed with concentrated SVF using a centrifuge and injected into the primary pain sites. After surgery, in all three cases, the subjective pain scale score decreased significantly over time.
INTRODUCTION
Postmastectomy pain syndrome (PMPS) is defined as chronic pain that persists for more than 3 months after breast cancer surgery. PMPS occurs in 25% to 60% of patients [1-3] and presents as dull, burning, and aching sensations in the chest, axilla, and ipsilateral upper extremity [4]. Although the exact mechanism of PMPS is not known, based on several studies, it is presumably related to damage to the intercostobrachial and axillary nerves during surgical dissection or to postoperative neuroma and fibrotic scar formation [2,4]. Several studies have investigated the psychosocial effects of PMPS and its negative effects on patients’ quality of life, emphasizing the importance of research into the treatment of PMPS [4,5]. The primary treatment for PMPS has been pharmacological symptom control targeting nociceptive factors with nonsteroidal anti-inflammatory drugs, selective serotonin-norepinephrine reuptake inhibitors, gabapentin, and pregabalin [4]. Regional anesthesia and botulinum toxin injection therapy have also been evaluated. However, these pharmacological treatments have produced only temporary pain relief [6].
Due to the limitations of pharmacological treatments, some studies have introduced fat grafting as an alternative treatment for PMPS. However, the exact mechanism of pain relief exhibited in patients after fat grafting has not been elucidated, and the effectiveness of fat grafting alone on PMPS remains controversial [7-10].
In this report, we describe preliminary results in three patients with PMPS who received a fat graft enriched with stromal vascular fraction (SVF), which is a fat extract rich in adipose-derived stem cells (ADSCs) with multipotent differentiation capacity [11,12].
CASE REPORT
Three patients who suffered from PMPS for more than 1 year after nipple- or skin-sparing mastectomy with subsequent reconstruction (implants in one patient and pedicled transverse rectus abdominis myocutaneous [TRAM] flaps in two patients) were selected and injected with SVF-enriched autologous fat. In each process, anesthesia included local anesthesia with a dilute solution of lidocaine with epinephrine (1:100,000), sedation and pain control with midazolam (10 mg) and pethidine (25 mg), and a tumescent solution consisting of 1 L of Hartmann’s solution, epinephrine (1 mg), and lidocaine (500 mg) injected into the fat harvest site and the graft site, respectively. To extract the SVF, 50 mL of fat was harvested from the patient’s abdomen, from which 3 mL of SVF was concentrated using an automated SVF isolation system (Cellunit; CGBio, Seoul, Korea). The number of cells in 10 μL of extracted SVF was counted using a fluorescence cell counter device (Luna-FL; Logos Biosystems, Anyang, Korea). The SVF was mixed with additional fat and injected into the fat layer of the postmastectomy pain site. Self-assessment using a numeric rating scale (NRS) was performed from 1 to 24 weeks postoperatively to estimate the pain pattern and intensity at the postmastectomy pain site.
Case 1
The patient was a 52-year-old woman diagnosed with left breast cancer without underlying disease. The patient underwent skin-sparing mastectomy and immediate breast reconstruction surgery with a pedicled TRAM flap. She then received adjuvant hormonal therapy with tamoxifen. The patient had suffered from PMPS for 13 months. Before the fat graft surgery, the patient’s overall NRS pain score was 4 in the left breast: 4 for the upper medial side, 5 for the upper lateral side, 4 for the lower medial side, and 5 for the lower lateral side. The pain was described as a moderate stabbing, annoying, stinging, and sensitive sensation. Fat was harvested from the patient’s abdomen and grafted to the upper pole of the left breast, and 12 mL of centrifuged fat added to 3 mL of SVF (cell count: 2.44×105 cells/mL, extracted from 50 mL of fat) was injected into each pain site. The patient’s NRS pain score gradually decreased. At 16 weeks after surgery, a pain-free state was attained with an NRS pain score of 0 (Fig. 1).
Case 2
A 52-year-old female patient had suffered PMPS in her right breast for 24 months after nipple-sparing mastectomy and immediate breast reconstruction surgery with silicone implants. The patient’s overall NRS pain score before the fat graft surgery was 8. The pain sites were the right shoulder, the right axilla, the inner side of the upper arm, and the lower and lateral sides of the right breast. The pattern of pain was very diverse, described as a severe stabbing, sharp, heavy, and sensitive sensation. Fat was harvested from the patient’s abdomen, and 9 mL of centrifuged fat mixed with 3 mL of SVF (cell count: 2.8×107 cells/mL; extracted from 50 mL of fat) was injected into the upper lateral pole of the right breast. The patient’s NRS pain score gradually decreased and at 24 weeks postoperatively, only a stabbing pain and heavy sensation of pain were reported (Fig. 2).
Case 3
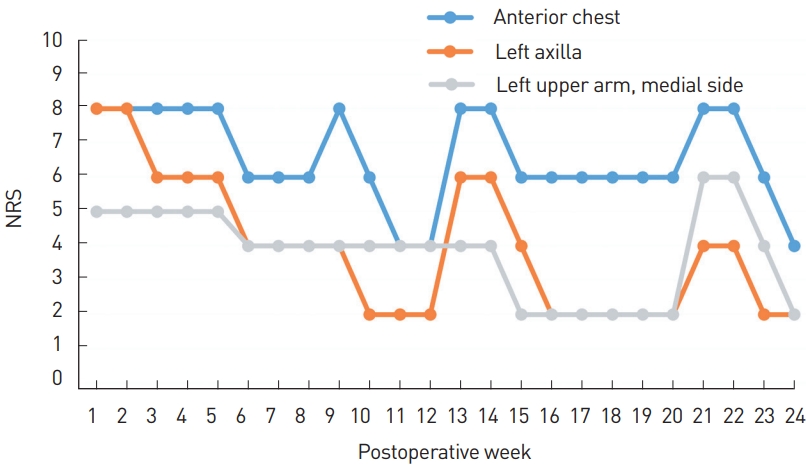
A 51-year-old patient was diagnosed with PMPS associated with a skin-sparing mastectomy of the left breast and immediate breast reconstruction surgery with a TRAM flap and contralateral reduction mammoplasty. She also underwent adjuvant chemotherapy and hormonal therapy with tamoxifen postoperatively. The patient suffered from PMPS for 17 months. The patient’s preoperative overall NRS pain score was 6. The upper and lateral sides of the left breast had the highest NRS pain score of 8, followed by the left shoulder with an NRS pain score of 6, and the left axilla and upper medial side of the breast each with an NRS pain score of 4. The patient described most of the pain patterns as throbbing, burning, heaviness, and tearing, all of which were severe. By harvesting fat from the patient’s abdomen, a total of 37.5 mL of fat was grafted to the upper pole of the left breast, which included 3 mL of SVF extracted from the 50 mL of fat. Pain in the breast area decreased after the SVF-enriched fat grafting. The NRS pain score of the axilla area markedly decreased from 8 to 2 postoperatively (Fig. 3).
DISCUSSION
Although the exact mechanism of pain relief in fat grafting has not been elucidated, it has been observed that fat grafting not only has its own cushioning effect, but also reduces neuropathic pain by resolving nerve entrapment through scar remodeling and neuroinflammation through the anti-inflammatory action of the ADSCs in fat [13].
SVF is a heterogeneous mixture of cells containing many ADSCs. Although the neuroprotective effects of SVF are like those of ADSCs, in terms of immunomodulation, SVF exhibits superior effects compared to ADSCs alone. Therefore, the focus of research has shifted to fat graft studies using SVF. There are four known mechanisms of SVF: angiogenesis, differentiation potential, immunomodulatory properties, and secretion of extracellular matrix [8,12].
Several studies have reported that the SVF contained in fat tissue has a multipotent differentiation capacity for scar remodeling and anti-inflammatory action. Remodeling of the posttraumatic scar occurs after fat grafting, resulting in nerve release and adjacent soft tissue regeneration that reduces pain [9,10]. In one study, SVF-enriched fat grafting was performed in five patients with damage to the superficial branch of the radial nerve, resulting in pain relief that persisted for 3 years [14].
In recently published randomized controlled trials, autologous fat grafting alone did not show a significant effect on PMPS. However, these studies mainly evaluated PMPS cases without breast reconstruction [10,12].
The present case study evaluated PMPS in cases with both breast reconstruction surgery and mastectomy, and pain reduction at the mastectomy site was observed in all three patients. The findings suggest that SVF plays a role in reinforcing scar remodeling and promoting the anti-inflammatory action of ADSCs, which may be insufficient with fat grafting alone. These results must be verified in trials comparing a control group, a fat graft-only group, and an SVF-enriched fat graft group. Establishing the efficacy of SVF-enriched fat grafting, would improve the quality of life for patients suffering from PMPS.
Notes
This research was funded and supported by CGBio Co., Ltd., Seoul, Republic of Korea. No other potential conflicts of interest relevant to this article were reported.
Ethical approval
The study was exempted from approval by the Institutional Review Board of Asan Medical Center (IRB No. 2019-0653). The patients provided written informed consent for publication of their cases.